Abstract
Background: Exercise stress testing is used as a diagnostic and prognostic tool. We determined the prognostic significance of exercise test findings for cardiovascular (CVD) and all-cause mortality in men and women.
Material and methods: 3033 subjects underwent a symptom-limited bicycle exercise test. Exercise capacity was defined as the mean of last four minutes of exercise workload.
Results: During an average follow-up of 19 years, 186 (11.6%) CVD and 370 (20.6%) all-cause deaths in men and 57 (5.0%) CVD and 155 (12.5%) all-cause deaths in women occurred. Among exercise test variables (workload, ECG, BP, HR), exercise capacity was the strongest predictor of mortality. Low exercise capacity (1st quartile) was associated with a hazard ratio of 4.2 (95% CI: 1.7, 10.8) for CVD and 4.0 (95% CI: 2.5, 6.4) for all-cause mortality compared with high exercise capacity (4th quartile) among men and in women with a 5.4-fold (95% CI: 1.2, 24.0) risk for CVD and 2.3-fold (95% CI: 1.2, 4.3) risk for all-cause mortality, respectively. The relationship between other exercise test variables and mortality was much weaker.
Conclusions: Among exercise test variables exercise capacity was the strongest predictor of CVD and all-cause mortality in both genders, and especially CVD deaths in women.
Exercise capacity was the most powerful predictor of CVD and all-cause mortality in both men and women.
Low exercise capacity is a strong predictor of CVD death, especially among women.
Key Messages
Introduction
Exercise stress testing is widely used as a diagnostic and prognostic tool in subjects with cardiovascular symptoms, but its prognostic value may have been underestimated for asymptomatic subjects (Citation1). Some studies have explored which of the variables assessed during exercise testing and recovery are most important markers associated with cardiovascular (CVD) or all-cause mortality. Only a few studies have focused on women who were referred exercise testing due to clinical reasons. This information would provide clinically important information to show if gender differences in the risk estimation of CVDs could have been existed in population undergoing exercise testing (Citation2).
Exercise test findings in addition to ST-segment depression on electrocardiogram (ECG) have been shown to be associated with CVD and all-cause mortality (Citation3–5). Although ST depression during exercise has been a significant predictor of acute myocardial infarction, sudden cardiac death (Citation6–8) and CVD mortality in men (Citation3,Citation5,Citation9–13), inability to achieve 85% of age-predicted maximal heart rate during an exercise test has also been suggested to be an independent predictor of all-cause death (Citation14). Some other non-ECG variables such as chronotropic incompetence and heart rate recovery may predict CVD and all-cause mortality (Citation1,Citation14–20). A similar association between exercise capacity, CVD and all cause death has been presented in few studies performed among women (Citation9,Citation10,Citation21,Citation22). However, there is not enough evidence about the relationship between non-ECG related exercise test variables and mortality in both genders referred due to clinical indications.
The aim of this study was to determine which exercise test variables are strongest predictors of CVD or all-cause mortality. Our hypothesis was that, in addition to ST-depression, low exercise capacity, as well as impaired exercise-related heart rate and blood pressure (BP) responses are associated with CVD or all-cause mortality.
Material and methods
Study population
The study cohort consists of 3033 subjects (1792 men, 1241 women) who were referred for exercise testing and who underwent clinical bicycle exercise tests between 1988 and 1994 at the Department of Sports and Exercise Medicine, Oulu Deaconess Institute, Finland. The mean age of the men was 50.5 (standard deviation (SD) 10.3, range 16–80) years and women 52.4 (SD 8.9, range 16–80) years, respectively. The reasons for testing included diagnostic purposes (1592 men, 1118 women), evaluation of working ability (239 men, 151 women) or appropriate medical treatment (7 men, 3 women). Of these test reasons occurred among 21.8%, 3.9%, and 16.7% subjects, respectively.
Data collection and follow-up
The data of this study is based on assessment of clinical risk factors while referring subjects to exercise testing, the information collected and measured during the tests, as well as data from death records. The information on chronic diseases connected to CVDs was gathered from the Social Insurance Institution of Finland and it consists of received reimbursements for medicines used for diabetes, hypertension, coronary heart disease (CHD) and hypercholesterolemia between January 1988 and August 2010. Death certificates listing causes of death as CVD-related or all-cause formed the outcomes of interest. Vital status was determined for all subjects of the cohort as of May 1, 2012 by obtaining the information from the Cause of Death Register maintained by Statistics Finland. CVD deaths were coded using the Tenth International Classification of Diseases codes I00-I99.
Research ethics
The ethics committee of the Northern Osthrobothnia Hospital District was consulted. It stated that as the exercise testing and related measurements had been performed as part of routine clinical work, and the study participants were not contacted, ethics committee statement or written consent were not needed.
Exercise stress testing
All subjects were instructed not to eat two hours before exercise testing and to avoid smoking. They were also instructed to abstain from using alcohol 24 hours prior to the exercise testing. The use of beta-blockers was ceased for a minimum one day before coming to the exercise test. The use of other drugs was instructed separately by the referring doctor. The subjects arriving for an evaluation of working ability were on their normal medication.
Information on the participant’s health and medication was collected by the medical doctor before the exercise test. This included personal information (age, height, weight, occupation), referring institution, reason for testing (diagnostic, assessment of working ability, therapeutic), previous diseases and medication (history of myocardial infarction and diagnosed heart failure along with previous coronary bypass surgery or percutaneous coronary intervention (PCI) and use of β-blockers).
Height and weight were measured and body mass index (BMI) was computed as the ratio of weight in kilograms to the square of height in meters. BP was measured with a mercury sphygmomanometer at rest in supine position and after 3 and 5 minutes of standing. Baseline HR was measured at the same time.
The study subjects underwent a maximal symptom-limited bicycle exercise test. A standard 12-lead ECG was obtained continuously during exercise. The test started with a power output of 50 watts (W) that was raised by 50 W for men and 25 W for women every fourth minute up to the point of cessation of the test. Heart rate and BP were measured every second minute throughout the test, as well as after four and ten minutes post-exercise.
Most of the exercise tests were supervised by two persons. During the test, possible pains, shortness of breath or fatigue were documented and a summary statement of the test was made by the supervising doctor. The reason of cessation was documented as abnormal HR reaction, dyspnoea, ST-segment depression in ECG, chest pain or other reason (most commonly fatigue). ECG findings were classified based on ST-changes as normal, uncertain and pathological. The definition for pathological ischemic ECG finding was at least 1 mm ST segment depression. ST segment depression was defined as planar or downsloping ST segment shift of greater than 1 mm in magnitude measured 0.06 s after the J point (if HR <130/min, 0.08 s after the J point). Subject's exercise capacity was estimated as the mean (W) of last four minutes of exercise workload.
Statistical methods
Differences in baseline characteristics between deceased and living men and women were analyzed using the Student’s independent-samples t-test for continuous and the chi-square test or Fisher’s exact test for categorical variables. Descriptive data are presented as means (SD) and numbers (percentages).
Patients were divided into quartiles according to exercise capacity defined by workload (watts) achieved in the exercise test. The following categories of exercise capacity were used in men: the first quartile, less than 125 W; the second quartile, from 125 W to 161.9 W (125 W to 162.4 W for CVD death) the third quartile, from 162 W to 187.4 W (162.5 W to 189.1 W for CVD death); and the fourth quartile, more than 187.4 W (189.1 W for CVD death). The corresponding division was used for women: the first quartile, less than 81 W; the second from 81 W to 99.9; the third from 100 W to 112.4 W; and the fourth more than 112.4 W. The reference group for all models was the fourth quartile i.e. the patients in the best physical condition.
Risk factors for main outcomes were analyzed using Cox proportional-hazard regression models. Cox models were adjusted for age and BMI that were selected on the basis of their well-defined role as a predictive factor of mortality.
Exercise capacity was entered into the models as quartiles. We examined if ischemic ST-depression during exercise testing, resting and exercise systolic and diastolic BP and HR, diagnosed diseases, history of myocardial infarction, coronary bypass surgery or PCI and use of β-blockers were predictors of death in analysis adjusted for age and BMI. All variables significantly (p < 0.05) related to the outcome were entered in the multivariate models using the stepwise-method. From alike variables, we chose the one with the strongest correlation to death. If possible, covariates were entered uncategorized into the models. All tests for statistical significance were two-sided. The data were analyzed using IBM SPSS Statistics 19 (Armonk, NY).
Results
The characteristics of the study population according to all-cause mortality status are presented in and the baseline resting and exercise stress test characteristics are shown in . Exercise tests were performed mostly for diagnostic purpose (1592 men, 1118 women). Any specific reasons for exercise testing were not associated with mortality. The mean maximal workload was 157.4 W (SD 44.8, range 44.0–350.0 W) in men and 97.9 W (SD 24.8, range 28.0–212.5 W) in women. The average follow-up time to death or the end of follow-up was 19.1 years (range 0.02–24.4 years) in men and 19.9 years (range 0.6–24.4 years) in women. During the follow-up, there were 370 all-cause deaths in men and 155 in women, from which 186 (50.3%) deaths in men and 57 (36.8%) deaths in women were due to CVD reasons.
Table 1. Characteristics of the study population (n = 3033) according to all-cause mortality events.
Table 2. Baseline resting and exercise characteristics of the study population (n = 3033) according to all-cause mortality events.
Predictors of mortality
The following factors were associated with all-cause and CVD mortality in men after adjustment for age and BMI: exercise capacity (all-cause and CVD, p < 0.001), maximal heart rate (all-cause, p < 0.001), resting systolic BP (all-cause, p = 0.001), prevalent CHD (all-cause and CVD, p = 0.026–0.016), history of myocardial infarction (all-cause and CVD, p = 0.049–0.021), ischemic ST-depression (CVD, p < 0.001), low heart rate reserve (CVD, p = 0.001), coronary bypass surgery/PCI (CVD, p = 0.037) and use of β-blockers (CVD, p = 0.038). In women heart rate reserve (p = 0.006) was inversely related to the risk of all-cause death. Exercise capacity (p = 0.055), ischemic ST-depression (p = 0.047) and systolic BP recovery (p = 0.015) were associated with CVD mortality in women after adjustment for age and BMI. After adjustments for the abovementioned predictors of mortality for men and women, exercise capacity remained as a significant independent risk factor for mortality.
Exercise capacity and mortality
The HRs for CVD and all-cause mortality according to the quartiles of exercise capacity based on multivariate analyses adjusted for age, BMI and other factors significantly associated with mortality in univariate analyses are presented in . In univariate analyses, men with low exercise capacity had a 22-fold risk for CVD and a 10-fold risk for all-cause deaths compared with those who had high exercise capacity, respectively. Furthermore, women with low exercise capacity had a 22-fold risk for CVD and a six fold risk for all-cause death compared to those with highest exercise capacity as shown in . Cumulative survival curves (proportions) of CVD and all-cause mortality according to the quartiles of maximal workload are depicted in . Exercise capacity was inversely associated with risk for CVD (p = 0.004) and all-cause deaths across the quartiles (p for trend <0.001) in men. Men with low exercise capacity had an increased risk for CVD (HR 4.2, 95% CI: 1.7, 10.8; p = 0.002) and for all-cause deaths (HR 4.0, 95% CI: 2.5, 6.4; p < 0.001) (). Men with highest exercise capacity had an 8% lower risk for CVD and 20% lower risk for all-cause deaths compared with those in the lowest fitness category ().
Figure 1. All-cause and CVD deaths are presented by Cox multivariate proportional hazard regression models according to achieved maximal workload (watts) during maximal exercise testing. (a) shows all-cause mortality in men and (b) in women. (c) shows CVD mortality in men and (d) in women. The cut-off values concerning CVD mortality for men were <125 W (n = 274), 125–162.49 W (n = 441), 162.5–189.12 W (n = 415) and ≥189.12 W (n = 378) and for women <81 W (n = 206), 81–99.99 W (n = 264), 100–112.49 W (n = 285) and ≥112.5 W (n = 311) according to quartiles. The cut-off values for all-cause mortality among men were <125 W (n = 348), 125–161.99 W (n = 485), 162–187.49 W (n = 404) and ≥187.5 W (n = 446) and in women <81.0 W (n = 240), 81–99.99 W (n = 293), 100–112.49 W (n = 304) and ≥112.50 W (n = 319).
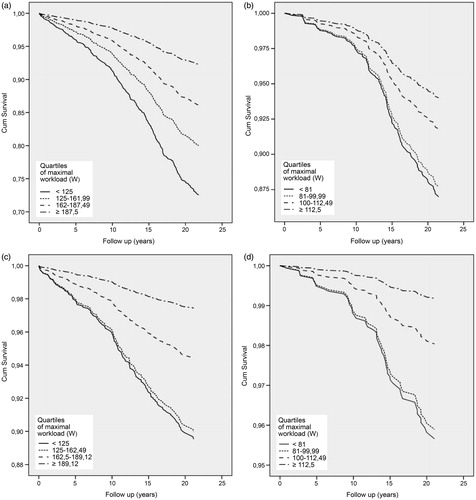
Table 3. Sex-specific adjusted hazard ratios and their 95% CI for the association of exercise capacity during exercise stress test with CVD and all-cause mortality among the study population (n = 3033).
Consistently, exercise capacity was inversely associated with all-cause mortality across the quartiles (p for trend = 0.031) among women. Low exercise capacity was related to a 5-fold (HR 5.4, 95% CI: 1.2, 24.0; p = 0.027) risk for CVD and a 2-fold (HR 2.3, 95% CI: 1.2, 4.3; p = 0.012) risk for all-cause death (). Women with highest exercise capacity had a 4% lower risk for CVD and a 7% lower risk for all-cause death when compared with those in the lowest fitness category ().
Discussion
The main finding of this study was that among all exercise test variables exercise capacity was the strongest predictor of CVD and all-cause mortality consistently associated with an increased risk in both genders, and especially CVD deaths in women.
Exercise capacity as a predictor of all-cause and cardiovascular mortality
On the basis of our recent study, the risk for CVD deaths in the lowest exercise capacity quartile was 4-fold in men and 5-fold in women. Our results are in accordance with a recent study which demonstrated that low exercise capacity was an independent predictor of increased CVD mortality (Citation23). An inverse association between exercise capacity and mortality has been suggested and therefore, fitness has been considered as an indicator of life-expectancy. Moderate levels of fitness even seem to protect against the influence of other predictors of mortality (smoking, elevated cholesterol levels and BP) both in men and women (Citation9). Furthermore, a recent meta-analysis suggested that fitness strongly predicted mortality regardless of the level of BMI (Citation24). Although the relationship between exercise capacity and mortality is well established among men, some studies have suggested that low exercise capacity is independently associated with increased CVD and all-cause mortality among women (Citation9,Citation10,Citation21,Citation22,Citation25). Our results showed that exercise capacity was the strongest predictor of CVD and all-cause mortality among women. We observed that exercise workload above the second quartile (>100 W) compared with the highest exercise capacity reduced both CVD and all-cause mortality, emphasizing an inverse association between exercise capacity and CVD and all-cause mortality.
In men, exercise capacity has been shown to have a strong, graded, inverse association with overall, CVD and non-CVD related mortality (Citation3,Citation5,Citation9–13). Our study demonstrated that already an increase in exercise capacity above the 1st quartile (125 W women and 163 W men) reduced all-cause mortality in women and CVD mortality among men in a dose-dependent manner. Previous studies have demonstrated that low exercise capacity is an independent predictor of CVD and of comparable importance with that of diabetes mellitus and other CVD risk factors in men (Citation13). Exercise capacity seems to be a powerful risk factor for future stroke, nonfatal and fatal cardiovascular events such as sudden cardiac death beyond that predicted by many conventional risk factors in men (Citation6,Citation8,Citation26–28).
Low exercise capacity seemed to be a strong predictor of premature CVD death in women. Possible differences in risk assessment between men and women may be explained by biological mechanisms such as hormonal effects on exercise test responses and ECG parameters (Citation29). There are also differences in CVD event manifestations (e.g. type and timing) among men and women (Citation2) which could possibly affect the association between exercise capacity and mortality, but the exact mechanistic pathways for the proposed differences are still unclear. However, consistently with a previous study (Citation30) it is recommended to focus on exercise capacity in CVD risk assessment among women.
Other exercise test findings and outcomes
Exercise induced ST depression has been suggested to be a significant predictor of acute myocardial infarction (Citation31) and observed among men who subsequently died (Citation3–5). Furthermore, ST-segment depression during exercise test was a strong predictor of sudden cardiac death in men with any conventional risk factor but no previously diagnosed CHD (Citation7).
We observed that heart rate reserve was related to fatal CVD events in men and all-cause mortality in women, although heart rate recovery after exercise testing was not a significant predictor. This finding is in accordance with a study demonstrating that poor fitness predicts CVD mortality in healthy men (Citation32). Furthermore, maximal heart rate has also been shown to predict all-cause mortality (Citation3). In previous studies, heart rate during recovery has been suggested to be associated with CVD and all-cause mortality events, as well as the risk of sudden death (Citation1,Citation14–16,Citation22,Citation32–34).
We found an association between systolic BP recovery and CVD deaths in women. In accordance with this finding, an elevated systolic BP after exercise was shown to be a predictor of CVD death and the risk of acute myocardial infarction (Citation7,Citation35). In addition, excessive increase in BP was shown to be associated with stroke (Citation36) and other CVD outcomes (Citation35).
Strengths and limitations
The strength of this study is a long follow-up of a large sample of subjects referred to a bicycle exercise test. Furthermore, the tests were performed at the same clinic and in most of the cases by the same doctor. A limitation of this study is that we did not have information about smoking and possible changes occurring during follow-up in patient characteristics that may affect mortality risk. Information on diagnosed diseases was complemented through gathering data about underlying diseases from Finnish register data. Exercise capacity was assessed by using the grade of the bicycle ergometer rather than by directly measuring oxygen consumption, which might be more accurate. Our findings may differ from other studies because we used bicycle ergometer which is commonly used in Europe, whereas in the USA treadmill is preferred (Citation1). Finally, the study population was derived from a single managed care organization and the patients were referred for the exercise test due to clinical indications.
Conclusion
It is important for a physician to be aware of the significance of exercise capacity as a predictor for premature death. Assessment of exercise capacity provides clinically important risk information and a useful, relatively low cost and safe tool for improving risk assessment both in men and women. Low exercise capacity warrants further clinical investigations, as well as exercise counseling for the patients. This study suggests that increasing physical activity and improving physical fitness is recommendable. Hence, physicians should also make efforts to persuade policy makers to better integrate the value of physical activity into the healthcare paradigm.
Funding information
This study was funded by the Northern Ostrobothnia Hospital District and Oulu Deaconess Institute.
Disclosure statement
The financiers had no control on the conduct or the publication of the study. The authors declare that they have no conflicts of interest regarding this article.
References
- Palatini P. Exercise testing in asymptomatic subjects: from diagnostic test to prognostic tool? Eur Heart J. 2008;29:1803–6.
- Leening MJ, Ferket BS, Steyerberg EW, Kavousi M, Deckers JW, Nieboer D, et al. Sex differences in lifetime risk and first manifestation of cardiovascular disease: prospective population based cohort study. BMJ. 2014;349:g5992. doi:10.1136/bmj.g5992.
- Prakash M, Myers J, Froelicher VF, Marcus R, Do D, Kalisetti D, et al. Clinical and exercise test predictors of all-cause mortality: results from >6,000 consecutive referred male patients. Chest. 2001;120:1003–13.
- Savonen KP, Kiviniemi V, Laukkanen JA, Lakka TA, Rauramaa TH, Salonen JT, et al. Chronotropic incompetence and mortality in middle-aged men with known or suspected coronary heart disease. Eur Heart J. 2008;29:1896–902.
- Spin JM, Prakash M, Froelicher VF, Partington S, Marcus R, Do D, et al. The prognostic value of exercise testing in elderly men. Am J Med. 2002;112:453–9.
- Laukkanen JA, Kurl S, Salonen R, Rauramaa R, Salonen JT. The predictive value of cardiorespiratory fitness for cardiovascular events in men with various risk profiles: a prospective population-based cohort study. Eur Heart J. 2004;25:1428–37.
- Laukkanen JA, Mäkikallio TH, Rauramaa R, Kurl S. Asymptomatic ST-segment depression during exercise testing and the risk of sudden cardiac death in middle-aged men: a population-based follow-up study. Eur Heart J. 2009;30:558–65.
- Minkkinen M, Nieminen T, Verrier RL, Leino J, Lehtimäki T, Viik J, et al. Impaired exercise capacity predicts sudden cardiac death in a low-risk population: enhanced specificity with heightened T-wave alternans. Ann Med. 2009;41:380–9.
- Blair SN, Kampert JB, Kohl HW 3rd, Barlow CE, Macera CA, Paffenbarger RS Jr, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276:205–10.
- Blair SN, Kohl HW 3rd, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262:2395–401.
- Laukkanen JA, Lakka TA, Rauramaa R, Kuhanen R, Venäläinen JM, Salonen R, et al. Cardiovascular fitness as a predictor of mortality in men. Arch Intern Med. 2001;161:825–31.
- Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801.
- Wei M, Kampert JB, Barlow CE, Nichaman MZ, Gibbons LW, Paffenbarger RS Jr, et al. Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA. 1999;282:1547–53.
- Adabag AS1, Grandits GA, Prineas RJ, Crow RS, Bloomfield HE, Neaton JD, et al. Relation of heart rate parameters during exercise test to sudden death and all-cause mortality in asymptomatic men. Am J Cardiol. 2008;101:1437–43.
- Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS. Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med. 1999;341:1351–7.
- Cole CR, Foody JM, Blackstone EH, Lauer MS. Heart rate recovery after submaximal exercise testing as a predictor of mortality in a cardiovascularly healthy cohort. Ann Intern Med. 2000;132:552–5.
- Kiviniemi AM, Tulppo MP, Hautala AJ, Mäkikallio TH, Perkiömäki JS, Seppänen T, et al. Long-term outcome of patients with chronotropic incompetence after an acute myocardial infarction. Ann Med. 2011;43:33–9.
- Myers J, Tan SY, Abella J, Aleti V, Froelicher VF. Comparison of the chronotropic response to exercise and heart rate recovery in predicting cardiovascular mortality. Eur J Cardiovasc Prev Rehabil. 2007;14:215–21.
- Savonen KP, Lakka TA, Laukkanen JA, Halonen PM, Rauramaa TH Salonen JT, et al. Heart rate response during exercise test and cardiovascular mortality in middle-aged men. Eur Heart J. 2006;27:582–8.
- Savonen KP, Lakka TA, Laukkanen JA, Rauramaa TH, Salonen JT, Rauramaa R. Usefulness of chronotropic incompetence in response to exercise as a predictor of myocardial infarction in middle-aged men without cardiovascular disease. Am J Cardiol. 2008;101:992–8.
- Gulati M, Pandey DK, Arnsdorf MF, Lauderdale DS, Thisted RA, Wicklund RH, et al. Exercise capacity and the risk of death in women: the St James Women Take Heart Project. Circulation. 2003;108:1554–9.
- Mora S, Redberg RF, Cui Y, Whiteman MK, Flaws JA, Sharrett AR, et al. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: a 20-year follow-up of the lipid research clinics prevalence study. JAMA. 2003;290:1600–7.
- Minkkinen M, Nieminen T, Verrier RL, Leino J, Lehtimäki T, Viik J, et al. Prognostic capacity of a clinically indicated exercise test for cardiovascular mortality is enhanced by combined analysis of exercise capacity, heart rate recovery and T-wave alternans. Eur J Prev Cardiol. 2015;22:1162–70.
- Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN. Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis. 2014;56:382–90.
- Peterson PN, Magid DJ, Ross C, Ho PM, Rumsfeld JS, Lauer MS, et al. Association of exercise capacity on treadmill with future cardiac events in patients referred for exercise testing. Arch Intern Med. 2008;168:174–9.
- Kurl S, Laukkanen JA, Rauramaa R, Lakka TA, Sivenius J, Salonen JT. Cardiorespiratory fitness and the risk for stroke in men. Arch Intern Med. 2003;163:1682–8.
- Laukkanen JA, Mäkikallio TH, Rauramaa R, Kiviniemi V, Ronkainen K, Kurl S. Cardiorespiratory fitness is related to the risk of sudden cardiac death: a population-based follow-up study. J Am Coll Cardiol. 2010;56:1476–83.
- Sui X, LaMonte MJ, Blair SN. Cardiorespiratory fitness as a predictor of nonfatal cardiovascular events in asymptomatic women and men. Am J Epidemiol. 2007;165:1413–23.
- Bokhari S, Bergmann SR. The effect of estrogen compared to estrogen plus progesterone on the exercise electrocardiogram. J Am Coll Cardiol. 2002;40:1092–6.
- D'Amore S, Mora S. Gender-specific prediction of cardiac disease: importance of risk factors and exercise variables. Cardiol Rev. 2006;14:281–5.
- Laukkanen JA, Kurl S, Salonen R, Lakka TA, Rauramaa R, Salonen JT. Systolic blood pressure during recovery from exercise and the risk of acute myocardial infarction in middle-aged men. Hypertension. 2004;44:820–5.
- Engeseth K, Hodnesdal C, Grundvold I, Liestøl K, Gjesdal K, Erikssen G, et al. Heart rate reserve predicts cardiovascular death among physically unfit but otherwise healthy middle-aged men: a 35-year follow-up study. Eur J Prev Cardiol. 2016;23:59–66.
- Jouven X, Empana JP, Schwartz PJ, Desnos M, Courbon D, Ducimetière P. Heart-rate profile during exercise as a predictor of sudden death. N Engl J Med. 2005;352:1951–8.
- Morshedi-Meibodi A, Larson MG, Levy D, O'Donnell CJ, Vasan RS. Heart rate recovery after treadmill exercise testing and risk of cardiovascular disease events (The Framingham Heart Study). Am J Cardiol. 2002;90:848–52.
- Sharman JE, LaGerche A. Exercise blood pressure: clinical relevance and correct measurement. J Hum Hypertens. 2015;29:351–8.
- Kurl S, Laukkanen JA, Rauramaa R, Lakka TA, Sivenius J, Salonen JT. Systolic blood pressure response to exercise stress test and risk of stroke. Stroke. 2001;32:2036–41.
