Abstract
Objective: CHA2DS2-VASc is the extension of the CHADS2 score developed by Birmingham 2009. This risk stratification schema is often used in clinical setting when considering additional risk factors for developing stroke in AF patients. However, its role in the non-AF population is unknown. This study was designed to evaluate the accuracy of the CHADS2 and the CHA2DS2-VASc scoring systems.
Methods: Studies designed for CHADS2 and CHA2DS2-VASc score in stratifying the risks for stroke development in non-AF patients were included.
Results: Among the 114 studies identified, six trials were chosen finally and included for meta-analysis. The pooled diagnostic odds ratio (DOR) for CHADS2 and CHA2DS2-VASc was 2.86 (95% CI =1.83–4.28) and 2.80 (95% CI =1.83–4.28), respectively. CHA2DS2-VASc score was of better sensitivity than CHADS2 score (0.920 vs. 0.768). However, both scores were showed to have inherent heterogeneity and poor specificity.
Conclusions: Though having good diagnostic accuracy, the clinical application of the CHADS2 and CHA2DS2-VASc scores in predicting risk of stroke development in non-AF patients still needs further validation.
The overall diagnostic accuracy of CHADS2 and CHA2DS2-VASc in stroke-risk stratification was good in patients with non-atrial fibrillation.
Key message
Introduction
According to a recent update from the American Heart Association, the age-adjusted death rate for stroke as an underlying cause of death was 37.9 per 100,000 (Citation1). The prominent risk factors for stroke include high blood pressure, diabetes mellitus, atrial fibrillation, high blood cholesterol, etc. Atrial fibrillation (AF) alone increases the risk of stroke by five-fold throughout all ages (Citation2) and the risk substantially underestimated as AF is often asymptomatic and mostly undetected clinically (Citation3). There has been great interest in developing stroke-risk prediction schemes for identifying patients at high risk of stroke, such as AF (Citation4). CHADS2 (Congestive heart failure, hypertension, age ≥75 years, diabetes, prior stroke/transient ischemic attack (TIA; double score)) and CHA2DS2-VASc (congestive heart failure, hypertension, age ≥75 years (double score), diabetes, prior stroke or TIA (double score), vascular disease, age 65–74 years, sex class (female)) scoring systems have gained prominent status as key prediction tools for stroke-risk stratification in AF (Citation5,Citation6). In both systems, patient stratification falls under three risk categories, 0 score is low risk, 1 is intermediate and ≥2 is high risk (Citation7).
Reports indicate that both CHADS2 and CHA2DS2-VASc can predict thromboembolic events after supraventricular arrhythmia (Citation8). However, the CHADS2 scheme has many limitations, including classification of a large proportion of patients as being at intermediate risk and does not include many stroke-risk factors (Citation9,Citation10). But, the CHA2DS2-VASc extends the stroke-risk factors of CHADS2, to include vascular diseases, age 65–74 years, and sex class, females. The CHA2DS2-VASc scheme has been shown to be as good as (and possibly better than) the CHADS2 scheme in predicting high risk patients with AF who develop stroke and thromboembolism (Citation4,Citation11). Chen et al. suggested that though the clinical utility of the CHADS2 and CHA2DS2-VASc scores are similar in predicting stroke and thromboembolism (TE), CHA2DS2-VASc has an advantage of identifying extremely low-risk patients with AF (Citation12). Studies elsewhere also suggest that CHA2DS2-VASc is often best to identify patients at ‘truly low risk’ of stroke/TE (Citation13,Citation14). It has also been shown to be effective in identifying patients at lower risk of poor outcomes and serious cardiac complications within three months following ischemic stroke, irrespective of the presence or absence of AF (Citation15).
Lip et al. have suggested that stroke-risk stratification schema used for AF can also be applied to non-AF populations with a similar (modest) predictive value. Owing to their simplicity, CHADS2 scores could potentially be used for a 'quick' evaluation of stroke risk in non-AF populations, in a similar manner to AF populations (Citation4). Recent reports provide further evidence for the clinical utility of CHADS2 and CHA2DS2-VASc scores in stroke-risk stratification (Citation16–18). CHADS2 also had been shown to have an impact on all-cause mortality after stroke, regardless of whether patients had AF (Citation19,Citation20). In fact, the CHADS2 score, which was originally developed for AF has been shown to have even greater prognostic value in patients who do not have AF (Citation19).
While meta-analysis and systematic reviews on the diagnostic accuracy of CHADS2 and CHA2DS2-VASc scores in patients with AF are available (Citation7,Citation12), systematic reviews on the accuracy of CHADS2 and CHA2DS2-VASc in non-AF population is lacking. The present study was undertaken to evaluate the accuracy of the CHADS2 and the CHA2DS2-VASc scoring systems in stratifying the stroke risk of patients with non-AF.
Methods
Selection criteria
We performed a literature search of the PubMed, Central, and EMBASE databases from inception until January 8, 2015, using a combination of the terms “CHADS2 OR CHA2DS2-VASc score AND stroke AND predict OR sensitivity OR specificity; and CHADS2 OR CHA2DS2-VASc AND stroke NOT atrial fibrillation”. Only studies in patients without AF, where the incidence of stroke or any other thromboembolic event was predicted using CHADS2, CHA2DS2-VASc scores, or both were included. A quantitative outcome was necessary for inclusion and the primary endpoints were defined as stroke or thromboembolic events.
We excluded letters, comments, editorials, case reports, proceedings, personal communications, as well as studies with no quantitative outcome. We also excluded trials where the study population was primarily patients with AF, or cannot distinguish patients without AF from the whole population included.
Study selection and data extraction
Studies identified by the search strategy were hand-selected and data extracted by two independent reviewers. Where there was uncertainty regarding eligibility, a third reviewer was consulted. The information like, the first author, year of publication, and the journal, study design, number of participants, participants’ age and gender, follow-up time, incidence of prior stroke, and the outcome measures were extracted.
The outcome measures analyzed were the endpoint events, like a stroke or any thromboembolic events, or hospitalization for stroke or transient ischemia.
Data analysis
Diagnostic odds ratio (DOR) was used as the index of diagnostic performance of CHADS2 and CHA2DS2-VASc scores in predicting stroke. DOR is defined as the ratio of odds of being tested positive in those who have a disease to the odds of being tested positive in those who do not have a disease; and therefore it is a single index that summarizes statistics for the accuracy of a diagnostic test (i.e., sensitivity and specificity). DOR >1 indicates good diagnostic performance in distinguishing stroke. Summary receiver operating characteristic (SROC) was also plotted for the overall testing accuracy. Larger area under SROC curve, ranging from 0.5 to 1.0, indicates good diagnostic performance. The pooled estimate of DOR was calculated by DerSimonian and Laird random-effects model and a two-sided p value <0.05 was considered statistically significant. Heterogeneity was assessed by using the Cochran Q and the I2 statistic. For the Q statistic, p < 0.10 was considered statistically significant for heterogeneity. The I2 statistic indicates the percentage of the observed between-study variability due to heterogeneity. The suggested ranges are as follows: no heterogeneity (I2 = 0–25%), moderate heterogeneity (I2 = 25–50%), large heterogeneity (I2 = 50–75%), and extreme heterogeneity (I2 = 75–100%). All statistical analyses were performed using the statistical software Meta-Disc 1.4 (XI Cochrane Colloquium, Barcelona, Spain) and Comprehensive Meta-Analysis, version 2.0 (Biostat, Englewood, NJ).
Quality assessment
The quality of included studies was assessed according to QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies) (Citation21). Data extraction and quality assessment were carried out independently by the same two investigators, and disagreements were resolved by consensus.
Results
Literature search
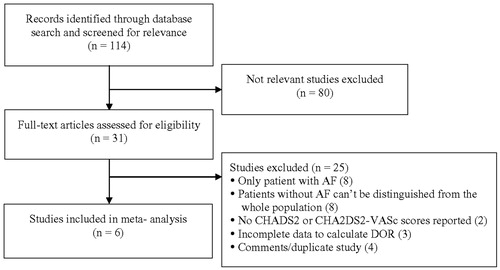
Of the 114 studies identified through the database, 80 studies were excluded due to lack of relevancy. After assessing 31 articles for full text reviewing, we excluded 25 studies, for reasons like, only patients with AF (n = 8), patients cannot be distinguished from the whole population (n = 8), no reported CHADS2 or CHA2DS2-VASc scores (n = 2), incomplete data to calculate DOR (n = 3), and comments or duplicate studies (n = 4). Six studies were included in the final meta-analysis. The flow diagram of the selection of trials is shown in .
Study characteristics
The basic characteristics of the six studies included in this meta-analysis are summarized in . All of them provided information about the CHADS2 score and four of them provided CHA2DS2-VASc score. Except for one small study (Citation8) (n = 108), five studies recruited at least 800 study participants (Citation4,Citation18,Citation19,Citation22,Citation23). The mean or median age of study participants ranged from 54.8 to 72.5 years. The proportion of males ranged from 47% to 80.72%. Three large cohort studies followed participants for up to 19 years. The proportion of stroke history ranged from 2.6% to 15.7% ().
Table 1. Summary of the basic characteristics of selected studies for meta-analysis.
Meta-analysis
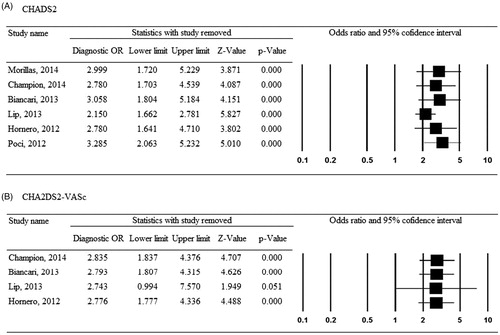
In five of the included studies, the cut-off point for CHADS2 score was 1, and a CHADS2 score equal to or greater than 1 was defined as positive results, otherwise it was defined as negative. The cut-off point was set to 2 for the other one study (Morillas et al.), as there were no participants having CHADS2 score of 0 (Citation22). Four of the six individual studies showed significantly better diagnostic performance of CHADS2 score in predicting stroke (DOR =1.93–5.00). The pooled DOR summarized by DerSimonian and Laird random-effects model was 2.86 (95% CI =1.79–4.55) with large heterogeneity across studies (Cochran-Q = 16.78, p = 0.0049, I2 = 70.2%) (). The SROC illustrated that the area under the curve was 0.6728 (standard error [SE] = 0.0609) (). The pooled sensitivity was 0.768 (95% CI =0.731–0.803) and the pooled specificity was 0.420 (95% CI =0.410–0.429; data not shown).
Figure 2. Meta-analysis for the diagnostic performance of CHADS2 in predicting stroke. (A) Forest plot; (B) summary receiver operating curve.
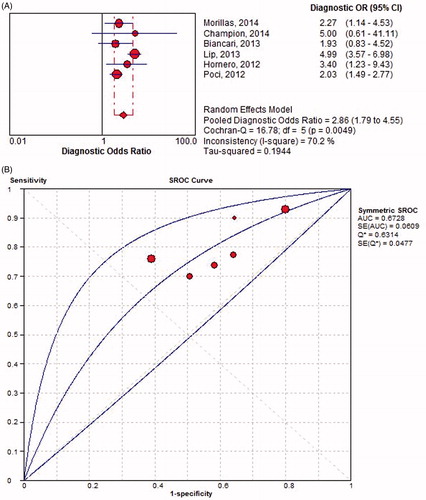
There was no evidence of heterogeneity between four individual studies (Cochran-Q = 0.10, p = 0.9918, I2 = 0%). The pooled DOR was 2.80 (95% CI = 1.83–4.28), indicating good test accuracy of CHA2DS2-VASc score (). The area under SROC was 0.6655 (SE = 0.0326) (). The pooled sensitivity and specificity was 0.920 (95% CI = 0.884–0.948) and 0.159 (95% CI = 0.151–0.167), respectively (data not shown).
Figure 3. Meta-analysis for the diagnostic performance of CHA2DS2-VASc in predicting stroke. (A) Forest plot; (B) summary receiver operating curve.
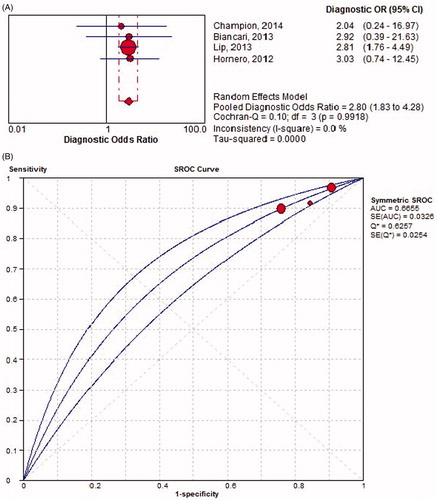
The pooled estimate for the test accuracy of CHADS2 score was stable as depicted by the leave-one-out sensitivity analysis; the magnitude and direction of DOR did not change considerably when any one individual study was removed (). However, for CHA2DS2-VASc score, the study by Lip et al. (Citation4) had slight influence on the pooled DOR ().
Quality assessment
The quality assessment analysis of the studies included is shown in . The selection bias and performance bias were relatively low in all the studies. However, all patients were not included in the final analysis of two studies, and it was unclear in one of the studies, indicating attrition bias. Similarly, there was high concern regarding the applicability of the studies included.
Table 2. Quality assessment.
Discussion
The present meta-analysis assessed the clinical utility of CHADS2 and CHA2DS2-VASc scoring system for predicting stroke and other thromboembolic events in patients with non-AF. The validity of CHADS2 and CHA2DS2-VASc scores on stroke-risk stratification in patients with AF has been well documented (Citation5–8,Citation12,Citation24,Citation25). However, the application of CHADS2 and CHA2DS2-VASc schema in patients with non-AF is relatively new and a few studies have explored this relatively simple method of risk assessment in non-AF population (Citation4,Citation17,Citation19,Citation22). The current review is the first to systematically analyze the existing literature and to evaluate the accuracy of the CHADS2 and the CHA2DS2-VASc in stroke-risk stratification in patients with non-AF.
The results reveal that the pooled DOR and SROC for both scoring systems were relatively close (DOR: CHADS2 2.86, CHA2DS2-VASc 2.80; SROC: CHADS2 0.6728, CHA2DS2-VASc 0.6655), suggesting that both CHADS2 and CHA2DS2-VASc were equally reliable and accurate in predicting stroke and other thromboembolic events in patients with non-AF ( and ). CHA2DS2-VASc score showed better sensitivity, as compared to CHADS2 (0.920 vs. 0.768; ). However, the specificity of both scores was not so good, with CHA2DS2-VASc score worse than the CHADS2 (0.159 vs. 0.420), which is probably because the risk factor profile of non-AF patients is not similar to that of AF patients and therefore, it is necessary that the risk factors for scoring schemes must be modified accordingly.
The studies included in the current meta-analysis comprised of a wider patient population, in terms of race and ethnicity, etiology of stroke/thromboembolism, risk profiles, treatment care and setting, use of anticoagulants, follow-up times, and primary endpoints. Two of the studies were retrospective analysis (Citation18,Citation23), while the rest were either prospective (Citation8,Citation19,Citation22) or registry-based with prospective follow-up (Citation4). However, all of them except for Biancari et al. (Citation18), did not consider the subtype of stroke (ischemic or hemorrhagic) while analyzing their results. The presence of these confounding factors may account for the heterogeneity observed in the current analysis. Nevertheless, the overall results reveal the diagnostic accuracy of CHADS2 and the CHA2DS2-VASc in non-AF patients as well, as demonstrated previously for the AF patient population (Citation7,Citation12,Citation13).
In a cohort study comprising of patient population with and without AF, Poci et al. have demonstrated that CHADS2 scores had even greater prognostic value in non-AF patients than in the AF patients, for whom it was originally developed for (Citation19). Further, they have also shown that the 10-year all-cause mortality was also strongly associated with the CHADS2 score in these two patient populations. The clinical utility of CHADS2 and the CHA2DS2-VASc scores were also indicated in critically ill patients in the intensive care unit, where it has been shown that they are predictive of supraventricular arrhythmia-related arterial thromboembolism (Citation8). CHADS2 has also been validated in hypertensive patients for estimating the risk of stroke or transient ischemic attack (Citation22).
Hornero and colleagues have compared CHADS2 and the CHA2DS2-VASc scoring systems with other predictive models for surgical coronary artery bypass grafting (CABG) stroke in patients undergoing isolated CABG and have found that CHADS2 and the CHA2DS2-VASc have good accuracy in predicting perioperative post-CABG stroke similar to other more complicated models of risk assessment (Citation23). Biancari et al. assessed the risk of stroke at later periods after CABG (Citation18). Through a systematic follow-up of patients post-surgery, they have found that freedom from stroke at 30 days, and at 1-, 5-, and 10-year follow-ups were 97.5%, 96.8%, 92% and 87%, respectively, and CHADS2 and the CHA2DS2-VASc were able to predict both immediate and late strokes as well as any fatal strokes (c-statistics: CHADS2, 0.641 and CHA2DS2-VASc, 0.716). Our pooled diagnostic ratio further validates these individual study results, where CHADS2 and the CHA2DS2-VASc scoring was shown to identify patients of high risk of stroke and can be used as a quick evaluation tool for stroke risk in both AF and non-AF populations, as suggested by Lip et al. (Citation4).
There are other comparable studies that explored the diagnostic accuracy of CHADS2 and CHA2DS2-VASc in this patient population (Citation15–17), however we did not include them because of incomplete data reporting. Similarly, our present analysis did not assess the role of stroke in increased mortality, as none of the studies included reported the distribution of patient deaths at each level of CHADS2 and CHA2DS2-VASc scores. The utility of pre-stroke CHADS2 and CHA2DS2-VASc scores in predicting long-term outcomes in non-AF patients with acute ischemic stroke has been previously reported (Citation16). Patients in the intermediate (pre-stroke CHADS2 and CHA2DS2-VASc scores = 1) and high risk (≥2) subgroups had a higher 5-year mortality and stroke recurrence. Reports elsewhere also demonstrate the benefit of CHADS2 (Citation26) and CHA2DS2-VASc (Citation27) in predicting in-hospital and short-term mortality rate in patients with AF. Though, it should be noted that this benefit was not observed in pre-stroke-risk assessment. Reports suggest that CHADS2 scoring was not reliable in predicting in-hospital mortality or risk for thrombus formation, especially in patients with low CHADS2 scores (Citation26,Citation28). In a retrospective analysis of 559 cardiac resynchronization therapy and implantable defibrillator patients, Perini et al., have shown that the risk of hospitalization and death is double for patients whose CHA2DS2-VASc score is >5. However, no such association was observed for the CHADS2 score (Citation29).
There are several limitations to the current analysis. Besides the heterogeneity of the included studies mentioned before, the cut-off points in each study were also varied, thus making it difficult to have a subgroup analysis of different risk levels. One of the main limitations for the application of CHADS2 is that it cannot differentiate between intermediate and low risk level, and patients with a score of 1 or 2 may have a stroke risk close to or even below the threshold for net benefit, thus potentially exposing them to unnecessary risk and burden of anticoagulant therapy (Citation10,Citation30,Citation31). The present review failed to offer any additional evidence for the utility of CHADS2 and CHA2DS2-VASc scores in discriminating patients of low and intermediate risk. Another major limitation to this study is that, we did not have enough individual patient data to do the subgroup analysis to account for the wide range of variations in the patient population. Similarly, most studies did not classify data based on the etiology or the stroke subtypes, nor did they provide data on the therapeutics administered, as anticoagulants and other vitamin K antagonists may affect the stroke outcome. In addition, we combined stroke and thromboembolism as one primary endpoint and the average incidence of different risk stratifications in this meta-analysis may not be the true stroke rate, thus introducing a possible bias. Further, our attempts to conduct meta-analysis on the role of stroke and increased mortality as assessed by CHADS2 and CHA2DS2-VASc scores in this patient population were not successful, due to the lack of mortality data. The distribution of the number of patient deaths at each score level of CHADS2 and CHA2DS2-VASc was not provided by the included studies.
In summary, the current analysis indicates that in patients with non-AF, the overall diagnostic accuracy of CHADS2 and CHA2DS2-VASc in stroke-risk stratification was good. However, due to the heterogeneity of the included studies and the low specificity, the present results need to be further validated in multicentric trials, with a larger cohort of patient population and after adjusting for variations in risk profiles, stroke subtypes and other potential confounding factors.
Funding information
This work was financially supported by the National Natural Science Foundation of China (Nos. 81271302 and 81070914, to J. R. Liu), the ‘‘Science and Technology Project’’ of the Shanghai Pudong New Area Health Bureau (Pudong New Area Population and Family Planning Commission) (No. PW 2013D-4, to J. R. Liu), Research Innovation Project from Shanghai Municipal Science and Technology Commission (No. 14JC1404300, to J. R. Liu), Open Fund of National Key Laboratory of Medical and Neurobiology of Fudan University (No. SKLMN2014001, to J. R. Liu), and project (2015) from SHSMU-ION Research Center for Brain Disorders (to J. R. Liu), and Clinical Science and Technology Innovation Project of Shanghai Shen Kang Hospital Development Center (No. SHDC12015310, to J. R. Liu).
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart Disease and Stroke Statistics—2015 Update: a report from the American Heart Association. Circulation. 2015;131:e29–322.
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8.
- Elijovich L, Josephson SA, Fung GL, Smith WS. Intermittent atrial fibrillation may account for a large proportion of otherwise cryptogenic stroke: a study of 30-day cardiac event monitors. J Stroke Cerebrovasc Dis. 2009;18:185–9.
- Lip GY, Lin HJ, Chien KL, Hsu HC, Su TC, Chen MF, et al. Comparative assessment of published atrial fibrillation stroke risk stratification schemes for predicting stroke, in a non-atrial fibrillation population: the Chin-Shan Community Cohort Study. Int J Cardiol. 2013;168:414–19.
- Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–70.
- Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137:263–72.
- Zhu WG, Xiong QM, Hong K. Meta-analysis of CHADS2 versus CHA2DS2-VASc for predicting stroke and thromboembolism in atrial fibrillation patients independent of anticoagulation. Tex Heart Inst J. 2015;42:6–15.
- Champion S, Lefort Y, Gaüzère BA, Drouet D, Bouchet BJ, Bossard G, et al. CHADS2 and CHA2DS2-VASc scores can predict thromboembolic events after supraventricular arrhythmia in the critically ill patients. J Crit Care. 2014;29:854–8.
- Lip GY, Halperin JL. Improving stroke risk stratification in atrial fibrillation. Am J Med. 2010;123:484–8.
- Karthikeyan G, Eikelboom JW. The CHADS2 score for stroke risk stratification in atrial fibrillation-friend or foe? Thromb Haemost. 2010;104:45–8.
- Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124.
- Chen JY, Zhang AD, Lu HY, Guo J, Wang FF, Li ZC. CHADS2 versus CHA2DS2-VASc score in assessing the stroke and thromboembolism risk stratification in patients with atrial fibrillation: a systematic review and meta-analysis. J Geriatr Cardiol. 2013;10:258–66.
- Xiong Q, Chen S, Senoo K, Proietti M, Hong K, Lip GY. The CHADS2 and CHA2DS2-VASc scores for predicting ischemic stroke among East Asian patients with atrial fibrillation: a systemic review and meta-analysis. Int J Cardiol. 2015;195:237–42.
- Olesen JB, Torp-Pedersen C, Hansen ML, Lip GY. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a Nationwide Cohort Study. Thromb Haemost. 2012;107:1172–9.
- Tu HT, Campbell BC, Meretoja A, Churilov L, Lees KR, Donnan GA, et al. Pre-stroke CHADS2 and CHA2DS2-VASc scores are useful in stratifying three-month outcomes in patients with and without atrial fibrillation. Cerebrovasc Dis. 2013;36:273–80.
- Ntaios G, Lip GY, Makaritsis K, Papavasileiou V, Vemmou A, Koroboki E, et al. CHADS2, CHA2S2DS2-VASc, and long-term stroke outcome in patients without atrial fibrillation. Neurology. 2013;80:1009–17.
- Mitchell LB, Southern DA, Galbraith D, Ghali WA, Knudtson M, Wilton SB, et al. Prediction of stroke or TIA in patients without atrial fibrillation using CHADS2 and CHA2DS2-VASc scores. Heart. 2014;100:1524–30.
- Biancari F, Asim Mahar MA, Kangasniemi OP. CHADS2 and CHA2DS2-VASc scores for prediction of immediate and late stroke after coronary artery bypass graft surgery. J Stroke Cerebrovasc Dis. 2013;22:1304–11.
- Poci D, Hartford M, Karlsson T, Herlitz J, Edvardsson N, Caidahl K. Role of the CHADS2 score in acute coronary syndromes: risk of subsequent death or stroke in patients with and without atrial fibrillation. Chest. 2012;141:1431–40.
- Henriksson KM, Farahmand B, Johansson S, Asberg S, Terent A, Edvardsson N. Survival after stroke-the impact of CHADS2 score and atrial fibrillation. Int J Cardiol. 2010;141:18–23.
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
- Morillas P, Pallarés V, Fácila L, Llisterri JL, Sebastián ME, Gómez M, et al. The CHADS2 score to predict stroke risk in the absence of atrial fibrillation in hypertensive patients aged 65 years or older. Rev Esp Cardiol (Engl Ed). 2015;68:485–91.
- Hornero F, Martin E, Paredes F, Gil O, Cánovas S, García R, et al. Stroke after coronary artery bypass grafting: preoperative predictive accuracies of CHADS2 and CHA2DS2VASc stroke risk stratification schemes. J Thorac Cardiovasc Surg. 2012;144:1428–35.
- Keogh C, Wallace E, Dillon C, Dimitrov BD, Fahey T. Validation of the CHADS2 clinical prediction rule to predict ischaemic stroke. A systematic review and meta-analysis. Thromb Haemost. 2011;106:528–38.
- Boriani G, Botto GL, Padeletti L, Santini M, Capucci A, Gulizia M, et al. Improving stroke risk stratification using the CHADS2 and CHA2DS2-VASc risk scores in patients with paroxysmal atrial fibrillation by continuous arrhythmia burden monitoring. Stroke. 2011;42:1768–70.
- Yarmohammadi H, Varr BC, Puwanant S, Lieber E, Williams SJ, Klostermann T, et al. Role of CHADS2 score in evaluation of thromboembolic risk and mortality in patients with atrial fibrillation undergoing direct current cardioversion (from the ACUTE Trial Substudy). Am J Cardiol. 2012;110:222–6.
- Sadeghi R, Parsa Mahjoob M, Asadollahi M, Abbasi Z. Prevalence, main determinants, and early outcome of patients with atrial fibrillation hospitalized with ischemic stroke: evaluation of the value of risk assessment scores for predicting risk of stroke or major bleeding following anticoagulation therapy. Acta Biomed. 2015;86:162–9.
- Yaghi S, Sherzai A, Pilot M, Sherzai D, Elkind MS. The CHADS2 components are associated with stroke-related in-hospital mortality in patients with atrial fibrillation. J Stroke Cerebrovasc Dis. 2015;24:2404–7.
- Paoletti Perini A, Bartolini S, Pieragnoli P, Ricciardi G, Perrotta L, Valleggi A, et al. CHADS2 and CHA2DS2-VASc scores to predict morbidity and mortality in heart failure patients candidates to cardiac resynchronization therapy. Europace. 2014;16:71–80.
- Go AS, Hylek EM, Chang Y, Phillips KA, Henault LE, Capra AM, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA. 2003;290:2685–92.
- Baruch L, Gage BF, Horrow J, Juul-Möller S, Labovitz A, Persson M, et al. Can patients at elevated risk of stroke treated with anticoagulants be further risk stratified? Stroke. 2007;38:2459–63.