Abstract
Objectives: To investigate the impact of sex on clinical outcomes after drug-eluting stent (DES) implantation in real-world patients.
Methods and results: A total number of 4720 patients (3365 males and 1355 females) undergoing the second-generation cobalt-chromium sirolimus-eluting stent (CoCr-SES) implantation from the FOCUS registry were included in this analysis. The cumulative incidences of major adverse cardiovascular event (MACE) (1.5% vs. 2.4%; p = .03), cardiovascular death (0.5% vs. 1.0%; p = .02) and target vessel revascularization (TVR) (0.3% vs. 0.8%; p = .01) within six months were significantly higher in females and the risks of MACE (adjusted hazard ratio [HR] 0.5 (0.3–0.9); p = .01) and TVR (adjusted HR 0.1(0.0–0.5); p = .001) remained significant in multivariate analysis. Reversely, the cumulative incidences of MACE (5.4% vs. 4.8%; p = .04) and any revascularization (5.1% vs. 3.3%; p = .01) were significantly higher in males beyond six months and the risks of all-cause death (adjusted HR 1.6 (1.1–2.5); p = .03) and cardiovascular death (adjusted HR 1.9 (1.1–3.6); p = .03) turned out to be significant in multivariate analysis. Notes: All cumulative incidences were presented as male vs. female; all HRs were calculated as male relative to female.
Conclusions: Females were associated with higher risk of early adverse events, while, males were associated with higher risk of late adverse events.
Females undergoing PCI are typically older, have more cardiovascular risk factors, while, males in need of PCI are more frequently associated with complex lesions.
The overall three-year cumulative incidences of adverse events are not significantly different between males and females but numerically higher in males.
Females are associated with significantly higher risks of MACE and TVR within six months, while, males are associated with significantly higher risk of all-cause mortality and cardiac mortality beyond 6 months.
Key messages
Introduction
Since the era of balloon angioplasty, the impact of sex on clinical outcomes after percutaneous coronary intervention (PCI) was continuously investigated. Early studies (Citation1–3) demonstrated that female sex was associated with worse clinical outcomes as compared with male sex, while, the results seemed to be reversed after the adoption of bare-metal stent (BMS) (Citation4,Citation5). In the past two decades, the advent of drug-eluting stent (DES) has greatly broadened the indication of PCI to high-risk patients. Nevertheless, the hot debate on sex-related differences in clinical outcomes after PCI among interventional cardiologists was far from over (Citation6).
To date, many trials aimed at investigating the impact of sex on clinical outcomes after PCI with DES have been conducted. Nonetheless, these studies included only a limited number of females and confined to patients with fewer risk factors and less complex lesions (Citation7,Citation8). Therefore, we performed an analysis using the large prospective multicenter FOCUS registry (ClinicalTrials.gov Identifier: NCT 00868829) data (Citation9,Citation10) to investigate the impact of sex on clinical outcomes after DES implantation in real-world patients.
Methods
Study design and patient population
A detailed design of the FOCUS registry has published elsewhere (Citation9,Citation10) and will not be elaborated here. In brief, the FOCUS registry was a large-scale, prospective study involving 83 clinical centers in three Asian countries (China, Thailand, and Indonesia). From March 2009 to February 2010, a total number of 5084 patients eligible to receive the second-generation cobalt-chromium sirolimus-eluting stent (CoCr-SES) were consecutively enrolled into the FOCUS registry. Thereby, the study population included real-world patients with severe complications and complex lesions who were usually excluded in randomized clinical trials.
The study was conducted according to the ethic guidelines of the Declaration of Helsinki. Prior to study initiation, the registry was approved by the Research Ethics Committee at each participating clinical centers depending on regional requirements. Written informed consents were obtained from all participating subjects.
Procedures and medications
All recruited patients were prescribed with antiplatelet therapy before the procedure of PCI according to the standard care of each center. Procedures and visual estimation of lesion characteristics were performed by experienced senior interventional cardiologists. One or more CoCr-SESs were allowed to be implanted into the target vessels according to the interventional clinicians’ discretions. Angiographic success was defined as a residual stenosis ≤30% by visual analysis in the presence of Thrombosis In Myocardial Infarction (TIMI) flow grade 3. Dual antiplatelet therapy (DAPT) with clopidogrel 75 mg and aspirin 100 mg per day was required to last for at least 12 months for all subjects and aspirin was required indefinitely after the end of DAPT. The follow-up of the study was scheduled at 30 days, six months, one year, two years and three years and conducted by telephone interview or hospital visit. Angiographic follow-up was not mandatory in the protocol.
Study endpoints and definitions
The primary endpoint was major adverse cardiovascular event (MACE), a composite of cardiovascular death, non-fatal MI and target vessel revascularization (TVR). The secondary endpoints included each individual component of MACE, all-cause death, any revascularization and definite/probable stent thrombosis (ST). All endpoints were defined according to Academic Research Consortium (ARC).
Data collection and management
Date was collected via electronic data capture in a web-based case report form. For quality control purposes, all participating centers were randomly monitored to detect and correct any inaccuracies in the reported data and to check for any infra-reporting of events. Approximately 10% of recorded data in each center was source-verified against the patients’ medical records and other applicable source documentation. All monitoring activities were conducted for all sites by an independent clinical research organization (China Cardiovascular Research Foundation, CCRF, Beijing, China). All events relating to endpoints were reported to and adjudicated by an independent clinical endpoints committee, which consisted of cardiologists not taking part in the study. These measures insured the accuracy of the data reported in this paper.
Statistical analysis
Normally distributed continuous variables were presented as means ± SD and were analyzed using the independent sample t test. Categorical variables were expressed as numbers and relative frequencies (percentage) and were compared using chi-square test or Fish’s exact test for independent groups. Kaplan–Meier analysis was used to calculate cumulative incidence of primary and secondary clinical outcomes to time and log-rank test was used to compare between groups. Landmark analysis was performed to evaluate the cumulative incidences of primary as well as secondary endpoints beyond six months among event-free survival patients. Cox proportional hazard methods were used to estimate crude and adjusted risk ratio of clinical events at each time point in relation to sex. Models were adjusted for age, body mass index, current smoking, hypertension, diabetes, family history of coronary artery disease, previous PCI, previous MI, previous coronary artery bypass graft (CABG), stable angina, acute coronary symptom, treatment of left main artery lesion, chronic total occlusion, bifurcation lesion, American Heart Association classification B2/C lesion, long lesion and small vessel lesion. Cox proportional–hazard models adjusted with the same variables were used to assess hazard ratios of MACE at three years in male sex compared with female sex among patient subgroups. All statistical analyses were performed with SPSS version 20.0 (IBM Corp., Amonk, NY) for windows.
Results
Baseline characteristics
Among 4720 patients included in this analysis, 3365 (71.3%) were males and the remaining 1355 (28.7%) were females. As shown in , females were approximately five years older; more frequently had diabetes, hypertension and stable angina, while, males were more frequently associated with obesity, current smoking, previous MI, and previous PCI.
Table 1. Baseline characteristics: male vs. female.
As demonstrated in , complex lesions except for small vessel lesion were more frequently presented in males. In addition, target vessels in males were significantly longer in length, greater in extent of diameter stenosis, while, target vessels in females were significantly smaller in diameter. Other detailed information about the baseline characteristics was depicted in and .
Table 2. Lesion characteristics: male vs. female.
Clinical outcomes
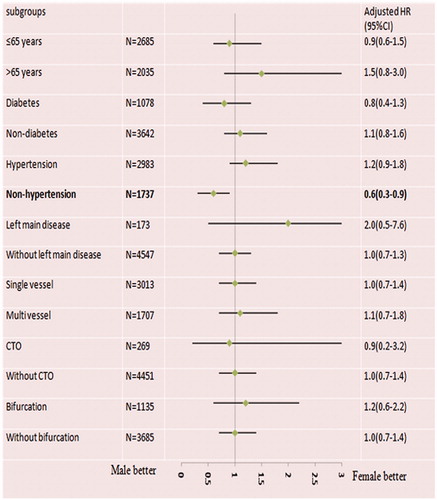
As illustrated in and , the three-year cumulative incidence of MACE (males 7.9% vs. females 7.2%; crude hazard ratio (HR) 1.1; 95% confidence interval (CI): 0.8–1.3; p = .59) was insignificantly different between males and females. So did the cumulative incidence of all-cause death, cardiovascular death, MI, TVR, and ARC definite/probable ST. However, further analysis within six months ( and ) revealed that the cumulative incidence of MACE (males 1.5% vs. females 2.4%; crude HR 0.6; 95% CI: 0.4–0.9; p = .03) was significantly greater in females. So did the incidences of cardiovascular death (males 0.5% vs. females 1.0%; crude HR 0.5; 95% CI: 0.2–0.9; p = .04) and TVR (males 0.3% vs. females 0.8%; crude HR 0.3; 95% CI: 0.1–0.8; p = .01). No difference for all-cause death, MI, any revascularization and ARC definite/probable ST was observed between males and females within six months, but all tended to be numerically higher in females. Reversely, the landmark analysis demonstrated that the cumulative incidence of MACE beyond six months (males 5.4% vs. females 4.8%; crude HR 1.4; 95% CI: 1.1–1.9; p = .04) was significantly higher in males. So did the incidence of any revascularization (males 5.1% vs. females 3.3%; crude HR 1.5; 95% CI: 1.1–2.1; p = .01). The incidences of all-cause death, cardiovascular death, MI, TVR, and ARC definite/probable ST tended to be numerically greater in males.
Figure 1. Survival analysis: Kaplan–Meier curves for cardiovascular death (A), myocardial infarction (B), target vessel revascularization (C) and major adverse cardiovascular event (D) at three years comparing males and females.
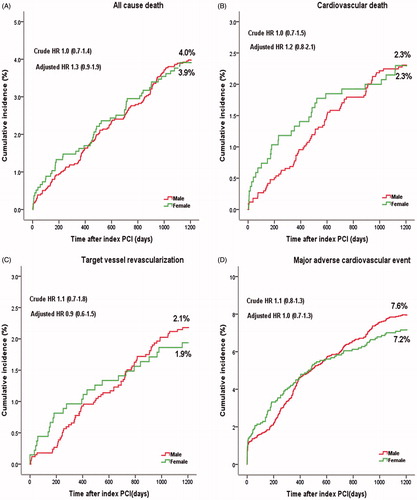
Figure 2. Survival analysis within six months and landmark analysis beyond six months for all-cause death (A), cardiovascular death (B), target vessel revascularization (C) and major adverse cardiovascular event (D).
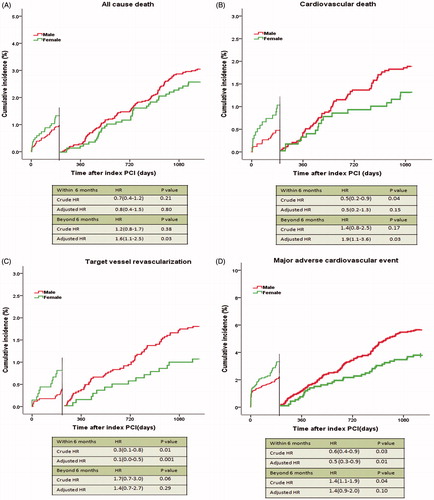
Table 3. Clinical outcomes comparing male and female for the entire three years follow-up, within six months and beyond six months.
Multivariate analysis
As presented in , at three years, the risks of MACE, all-cause death, cardiovascular death, MI and TVR remained insignificantly different between males and females. The risk of ARC definite/probable ST (adjusted HR 0.5 (0.2–1.3); p = .14) seems higher in females but still not powered enough to show significance. Within six months, the significantly higher risk of MACE (adjusted HR 0.5 (0.3–0.9); p = .01) and TVR (adjusted HR 0.1 (0.0–0.5); p = .001) in females remained significant in multivariate analysis. The risk of other adverse events also tended to be higher in females within six months although not powered enough to be significant. Beyond six months, the risks of MACE (adjusted HR 1.4 (0.9qh–2.0); p = .10) and any revascularization (adjusted HR 1.2 (0.8–1.8); p = .35) became insignificantly in multivariate analysis, but still tended to be higher in males. Notably, the insignificantly higher risks of all-cause death and cardiovascular death in univariate analysis in males turned to be significant (adjusted HR 1.6 (1.1–2.5); p = .03 for all-cause death and adjusted HR 1.9 (1.1–3.6); p = .03 for cardiovascular death) in multivariate analysis.
Figure 3. Forrest plots for adjusted hazard ratio (HR) of male relative to female for adverse events at entire three years follow-up, within six months and beyond six months. CI: confidence interval; MI: myocardial infarction; TVR: target vessel revascularization; MACE: major adverse cardiovascular event.
Subgroup analysis
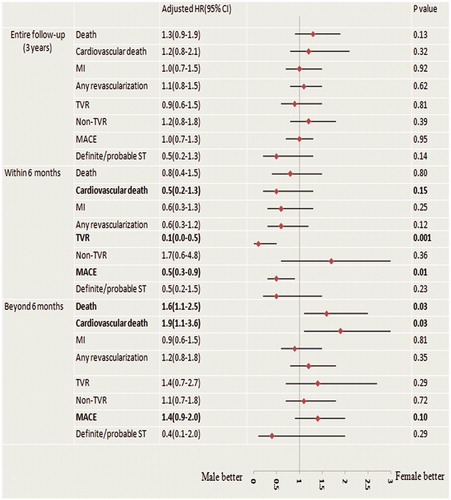
presents the results of subgroup multivariate analysis at three years. The risk of MACE was not significantly different between males and females in all subgroups except for patients without hypertension, in which male sex conferred a significant benefit for MACE (adjusted HR 0.6 (0.3–0.9)).
Discussion
The present analysis investigated the impact of sex on three-year clinical outcomes in real-world patients undergoing PCI with the second-generation CoCr-SES from the large prospective multicenter FOCUS registry. The main findings of the current study can be summarized as follows: First, females undergoing PCI are typically older, have more cardiovascular risk factors like hypertension and diabetes except for smoking habits and obesity, while, males in need of PCI are more frequently associated with complex lesions like left main lesion, chronic total occlusive lesion, and long lesion except for small vessel lesion. Second, the overall three-year cumulative incidences of adverse events are not significantly different between males and females but numerically higher in males. Third, females are associated with significantly higher risks of adverse events within six months, while, males are associated with significantly higher risk of cardiac mortality beyond six months.
In the era of balloon angioplasty, a number of studies revealed that female sex was a strong independent predictor of in-hospital mortality (Citation11). As compared with males, females were associated with lower rate of angiographic success, higher incidence of procedural complications and worse long-term clinical outcomes after PCI (Citation12,Citation13). Thereafter, studies focusing on performance of BMS found that implantation of BMS reduced sex-based differences in outcomes for patients undergoing PCI (Citation14–17). A study (Citation14) performed in patients treated with BMS concluded that female sex had a long-term survival advantage over male sex after PCI despite the higher rate of cardiac risk factors. Recently, another registry (Citation18) comparing long-term outcomes between males and females after BMS implantation reported significantly higher adjusted 10-year risks for all-cause death, MI, and TLR in males.
Currently, DES has been widely applied to clinical settings (Citation19,Citation20). However, most studies investigating sex-based differences after DES implantation failed to detect differences by sex in clinical outcomes (Citation7,Citation8,Citation21–26). A comprehensive analysis (Citation21) investigating the impact of sex on clinical outcomes after PCI with BMS and DES demonstrated no differences by sex for risk of all-cause death, MI and TVR at the entire three-year follow-up in both BMS- and DES-treated group. Similarly, another registry (Citation23) pooled individual data of all-comers with the unrestricted use of DES from three large comprehensive registries reported comparable long-term safety and efficacy among males and females at two years. Moreover, angiographic follow-up also showed no differences in terms of in-stent late loss and in-segment binary restenosis between males and females (Citation27). All these evidences seem to indicate that clinical outcomes after PCI are largely independent of sex in the era of DES. However, none of these studies has focused on short-term as well as long-term clinical outcomes simultaneously. In our study, the overall three-year outcomes are generally in accordance with the previous literatures. However, as demonstrated in the Kaplan–Meier curve (), there is a distinctive intercross between males and females, which means at some time point, the ascending speed of the cumulative incidence of adverse events was reversed between males and females. So we actually analyzed all the time points (in-hospital, 30 days, six months, one year and two years), and fortunately, we found that the results within six months and beyond six months strongly supported our hypothesis that females were associated with higher incidences of early adverse events, while, males were associated with higher incidences of late adverse events. Therefore, the overall three-year clinical outcomes belied the actually existed sex-related differences in clinical outcomes within six months and beyond six months, which may partially explain the insignificant differences observed at two or three years in previous reports(Citation21,Citation23,Citation28,Citation29).
In addition, females in the present study were more frequently associated with advanced age, diabetes and hypertension, resulting in an overall higher clinical risk profile at baseline. And the latter may translate into higher crude event rates among females. That’s may serve to explain why the significantly higher risk of cardiovascular death in females within six months became no longer significant after adjustment for baseline differences, while, the insignificantly higher risk of all-cause death and cardiovascular death in males beyond six months turned to be significant in the multivariate analysis. Meanwhile, in our study, males generally presented with more complex lesion, a strong independent predictor for repeat revascularization. Therefore, it was reasonable that the significantly higher risk of any revascularization in males beyond six months lost its significance in multivariate analysis, while the significantly higher risk of TVR in females within six months became even pronounced in multivariate analysis.
To further investigate the influence of sex in high-risk patients, Cox proportional–hazard regression analyses were also performed in subgroups in the present analysis. The results observed in subgroups were generally consistent with that observed in entire population. This may be attributable to excellent performance of the second-generation DES in general patients as well as high-risk patients. Whereas, it was noteworthy that males were associated with a lower risk of MACE in patients without hypertension, while, for the patients with hypertension, the risk of MACE tended to be higher in males, although not powered enough to show significance, indicating that hypertension was a stronger independent risk factor in males than in females.
Limitation
First, the intrinsic limitation of nonrandomized study is inevitable in our analysis, although we have performed multivariate analysis to adjust baseline differences between males and females, we cannot eliminate all confounding factors that may influence the overall clinical outcomes. Second, the fact that 7.2% of the initially enrolled patients had been lost at three-year follow-up and not included in this analysis should be acknowledged as a main factor affecting the results of the three-year analysis. Last but not least, as this is a large, multicenter registry involving 83 clinical centers from three countries and including a large population of patents, it is inevitable that some data like bleed events and the use of vascular closure devices are not complete in the database, in order to avoid making inaccurate conclusions, these data are not included in this analysis. This is, somehow, a limitation of the present analysis.
Conclusion
The overall three-year cumulative incidences of adverse events are insignificantly different between males and females. Further analysis demonstrated that females were associated with higher risk of early adverse events, while, males were associated with higher risk of late adverse events.
Acknowledgements
This work was supported by the National Natural Science Foundation [No. 81101133] and the Science and Technology Cooperation Project from the Shanghai Science and Technology Development [No. 14695840800].
Disclosure statement
The authors have no conflicts of interest to declare.
References
- Malenka DJ, O'Connor GT, Quinton H, Wennberg D, Robb JF, Shubrooks S, et al. Differences in outcomes between women and men associated with percutaneous transluminal coronary angioplasty. A regional prospective study of 13,061 procedures. Northern New England Cardiovascular Disease Study Group. Circulation. 1996;94:99–104.
- Cowley MJ, Mullin SM, Kelsey SF, Kent KM, Gruentzig AR, Detre KM, et al. Sex differences in early and long-term results of coronary angioplasty in the NHLBI PTCA Registry. Circulation. 1985;71:90–7.
- Kelsey SF, James M, Holubkov AL, Holubkov R, Cowley MJ, Detre KM. Results of percutaneous transluminal coronary angioplasty in women. 1985–1986 National Heart, Lung, and Blood Institute's Coronary Angioplasty Registry. Circulation. 1993;87:720–7.
- Jacobs AK, Johnston JM, Haviland A, Brooks MM, Kelsey SF, Holmes DJ, et al. Improved outcomes for women undergoing contemporary percutaneous coronary intervention: a report from the National Heart, Lung, and Blood Institute Dynamic registry. J Am Coll Cardiol. 2002;39:1608–14.
- Mehilli J, Kastrati A, Bollwein H, Dibra A, Schuhlen H, Dirschinger J, et al. Gender and restenosis after coronary artery stenting. Eur Heart J. 2003;24:1523–30.
- Grines CL, Schreiber T. Sex differences in the drug-eluting stent era: do they still exist? JACC Cardiovasc Interv. 2012;5:311–12.
- Lansky AJ, Costa RA, Mooney M, Midei MG, Lui HK, Strickland W, et al. Gender-based outcomes after paclitaxel-eluting stent implantation in patients with coronary artery disease. J Am Coll Cardiol. 2005;45:1180–5.
- Solinas E, Nikolsky E, Lansky AJ, Kirtane AJ, Morice MC, Popma JJ, et al. Gender-specific outcomes after sirolimus-eluting stent implantation. J Am Coll Cardiol. 2007;50:2111–16.
- Zhang F, Ge J, Qian J, Ge L, Zhou J. Real-world use of the second-generation cobalt-chromium sirolimus-eluting stents: 12-month results from the prospective multicentre FOCUS registry. EuroIntervention. 2012;8:896–903.
- Zhang F, Yang J, Qian J, Ge L, Zhou J, Ge J. Long-term performance of the second-generation cobalt-chromium sirolimus-eluting stents in real-world clinical practice: 3-year clinical outcomes from the prospective multicenter FOCUS registry. J Thorac Dis. 2016;8:1609–18.
- Lempereur M, Magne J, Cornelis K, Hanet C, Taeymans Y, Vrolix M, et al. Impact of gender difference in hospital outcomes following percutaneous coronary intervention. Results of the Belgian Working Group on Interventional Cardiology (BWGIC) registry. EuroIntervention. 2016;12:e216–23.
- Bell MR, Holmes DJ, Berger PB, Garratt KN, Bailey KR, Gersh BJ. The changing in-hospital mortality of women undergoing percutaneous transluminal coronary angioplasty. JAMA. 1993;269:2091–5.
- Weintraub WS, Wenger NK, Kosinski AS, Douglas JJ, Liberman HA, Morris DC, et al. Percutaneous transluminal coronary angioplasty in women compared with men. J Am Coll Cardiol. 1994;24:81–90.
- Berger JS, Brown DL. Gender-age interaction in early mortality following primary angioplasty for acute myocardial infarction. Am J Cardiol. 2006;98:1140–3.
- Mehilli J, Kastrati A, Dirschinger J, Bollwein H, Neumann FJ, Schomig A. Differences in prognostic factors and outcomes between women and men undergoing coronary artery stenting. JAMA. 2000;284:1799–805.
- Mehilli J, Kastrati A, Dirschinger J, Pache J, Seyfarth M, Blasini R, et al. Sex-based analysis of outcome in patients with acute myocardial infarction treated predominantly with percutaneous coronary intervention. JAMA. 2002;287:210–15.
- Malenka DJ, Wennberg DE, Quinton HA, O'Rourke DJ, McGrath PD, Shubrooks SJ, et al. Gender-related changes in the practice and outcomes of percutaneous coronary interventions in Northern New England from 1994 to 1999. J Am Coll Cardiol. 2002;40:2092–101.
- Yamaji K, Shiomi H, Morimoto T, Toyota T, Ono K, Furukawa Y, et al. Influence of sex on long-term outcomes after implantation of bare-metal stent: a multicenter report from the Coronary Revascularization Demonstrating Outcome Study-Kyoto (CREDO-Kyoto) Registry Cohort-1. Circulation. 2015;132:2323–33.
- Katz G, Harchandani B, Shah B. Drug-eluting stents: the past, present, and future. Curr Atheroscler Rep. 2015;17:485. doi: 10.1007/s11883-014-0485-2.
- Byrne RA, Joner M, Kastrati A. Stent thrombosis and restenosis: what have we learned and where are we going? The Andreas Grüntzig Lecture ESC 2014. Eur Heart J. 2015;36:3320–31.
- Onuma Y, Kukreja N, Daemen J, Garcia-Garcia HM, Gonzalo N, Cheng JM, et al. Impact of sex on 3-year outcome after percutaneous coronary intervention using bare-metal and drug-eluting stents in previously untreated coronary artery disease: insights from the RESEARCH (Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital) and T-SEARCH (Taxus-Stent Evaluated at Rotterdam Cardiology Hospital) Registries. JACC Cardiovasc Interv. 2009;2:603–10.
- Mikhail GW, Gerber RT, Cox DA, Ellis SG, Lasala JM, Ormiston JA, et al. Influence of sex on long-term outcomes after percutaneous coronary intervention with the paclitaxel-eluting coronary stent: results of the “TAXUS Woman” analysis. JACC Cardiovasc Interv. 2010;3:1250–9.
- Stefanini GG, Kalesan B, Pilgrim T, Raber L, Onuma Y, Silber S, et al. Impact of sex on clinical and angiographic outcomes among patients undergoing revascularization with drug-eluting stents. JACC Cardiovasc Interv. 2012;5:301–10.
- Sato H, Kasai T, Miyauchi K, Kubota N, Kajimoto K, Miyazaki T, et al. Long-term outcomes of women with coronary artery disease following complete coronary revascularization. J Cardiol. 2011;58:158–64.
- Funakoshi S, Furukawa Y, Ehara N, Morimoto T, Kaji S, Yamamuro A, et al. Clinical characteristics and outcomes of Japanese women undergoing coronary revascularization therapy. Circ J. 2011;75:1358–67.
- Toyota T, Furukawa Y, Ehara N, Funakoshi S, Morimoto T, Kaji S, et al. Sex-based differences in clinical practice and outcomes for Japanese patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ J. 2013;77:1508–17.
- Brown RA, Williams M, Barker CM, Mauri L, Meredith IT, Fajadet J, et al. Sex-specific outcomes following revascularization with zotarolimus-eluting stents: comparison of angiographic and late-term clinical results. Catheter Cardiovasc Interv. 2010;76:804–13.
- Regueiro A, Fernandez-Rodriguez D, Brugaletta S, Martin-Yuste V, Masotti M, Freixa X, et al. Sex-related Impact on clinical outcome of everolimus-eluting versus bare-metal stents in ST-segment myocardial infarction. Insights From the EXAMINATION Trial. Rev Esp Cardiol (Engl Ed). 2015;68:382–9.
- Ferrante G, Presbitero P, Corrada E, Campo G, Bolognese L, Vassanelli C, et al. Sex-specific benefits of sirolimus-eluting stent on long-term outcomes in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention: insights from the Multicenter Evaluation of Single High-Dose Bolus Tirofiban Versus Abciximab With Sirolimus-Eluting Stent or Bare-Metal Stent in Acute Myocardial Infarction Study trial. Am Heart J. 2012;163:104–11.