Abstract
Purpose: The purpose of this study is to compare midlife predictors of old age dementia with or without concomitant atherosclerotic cardiovascular disease (ASCVD).
Design: In the Helsinki Businessmen Study (men born in 1919–1934, n = 3309), death certificates (n = 1885) during up to 49-year follow-up (through 31 December 2013) were screened for dementia (n = 365) and ASCVD, and categorized as (1) AD without ASCVD (“pure” AD, n = 93), (2) AD + ASCVD (n = 126), (3) vascular dementia (VD, n = 82), (4) other or undefined etiology (n = 64). Using Cox analyses, death without dementia and dementia types were compared for the prediction by midlife ASCVD risk factors. Men without diagnosed dementia during follow-up were used as reference.
Results: ASCVD risk factors predicted death without dementia during follow-up. Midlife cholesterol was higher in AD + ASCVD and VD as compared with men surviving to old age without known dementia. None of the midlife factors including cholesterol and glucose tolerance predicted pure AD, but midlife cholesterol predicted AD + ASCVD, both as a continuous (hazard ratio [HR] per SD 1.24, 95% CI, 1.04–1.47), and dichotomous variable (cutpoint 6.5 mmol/L; HR 1.67, 95% CI, 1.16–2.40).
Conclusion: Midlife cholesterol predicted dementia with vascular features, but midlife vascular risk factors and glucose intolerance were not related to pure Alzheimer disease without concomitant atherosclerotic cardiovascular disease.
Heterogenous etiology of dementia, which in old age is usually a clinical diagnosis, may confound the role of long-term risk factors.
In a longitudinal study with autopsy records, midlife cholesterol predicted dementia with features of atherosclerotic cardiovascular disease but not “pure“ Alzheimer disease
Glucose tolerance in midlife was not associated with pure Alzheimer’s disease.
Key messages
Introduction
The most common diagnosis for progressing cognitive disorders (“dementia”) is probable Alzheimer disease (AD), which in older people is usually established clinically without neuropathological verification. Because AD is estimated to increase dramatically (Citation1), an intensive search for prevention is ongoing. Risk factors of atherosclerotic cardiovascular disease (ASCVD) have been suggested to predict AD in observational studies (Citation1–3). Accordingly, risk factors in midlife – high blood pressure (BP), hypercholesterolemia, obesity, physical inactivity, smoking, stroke, and diabetes – have been related to late-onset dementia, including AD. However, the results have been mixed. This may be due to the clinical variability of dementia in old age, where pathology stems from both neurodegenerative and vascular processes (Citation4–7). For example, two recent studies came to opposite conclusions about the relationship between glucose and dementia. High glucose and diabetes were identified as risk factors for clinical dementia (Citation8), but not for neuropathologically verified AD (Citation9), indicating etiological heterogeneity in dementia.
This heterogeneity can be reduced by studying homogenous cohorts and better discerning dementia types. Our hypothesis was that using an initially healthy, same gender, and socioeconomically similar cohort (the Helsinki Businessmen Study [HBS] (Citation10,Citation11)), detailed information from death certificates, and exceptionally long follow-up would give a more focused insight of the relationship between ASCVD risk and glucose tolerance in midlife and dementia in old age. The use of death certificates – where dementia diagnosis practically reflects a specialist (neurologist or geriatrician) diagnosis according to national guidelines – also gives an advantage over clinical examinations, because non-attendance does not disturb results.
Patients and methods
The Helsinki businessmen study
A cohort of 3490 initially healthy men has been followed-up since the 1960s for ASCVD risk factors, mortality, morbidity, and health-related quality of life (Citation10,Citation11). Initially, HBS was a pragmatic health examination cohort from the Institute of Occupational Health in Helsinki. Between 1964 and 1973 (average 1968), the men participated in volunteer health check-ups including clinical and laboratory examinations.
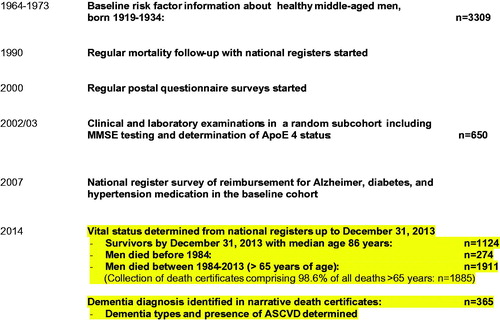
The follow-up has been approved by the Ethics Committee of the Helsinki University Hospital, Department of Medicine, and registered as ClinicalTrials.gov identifier NCT02526082. The flow chart of the present analyses is in .
Participants
All participants were Caucasian men, born 1919–1934, from the highest social strata being mainly businessmen or executives. Consequently, the cohort can be considered socioeconomically homogenous. The cohort for the present analyses includes 3309 men [94% of the total cohort] with information of baseline risk factors. Part of men (n = 612) participated in a 5-year ASCVD intervention study during the 1970s (Citation10), but their exclusion did not alter the present conclusions, and all were included in the analyses to improve statistical power.
Baseline measurements
The procedures between 1964 and 1973 included questionnaires, clinical examinations and laboratory tests after a 12-h fast (Citation10). Height and weight were measured and body mass index (BMI) calculated as weight/height squared (kg/m2). Smoking history was self-reported. BP was measured with a mercury sphygmomanometer in the sitting position after a 10 min rest. During the 1960s, serum cholesterol concentration was determined using the method of Huang et al., where after routine analyses with enzymatic methods have been used. The older method gave 8.3% higher values, and the corrected values were used here (Citation12). Glucose tolerance (1-h glucose) was measured as blood glucose (mmol/L) after 1 h of an oral glucose load (1 g per kg); it has predicted development of diabetes in our cohort (Citation13).
Follow-up procedures
Since 2000, postal questionnaires have been sent regularly to survivors (Citation10). The response rate in the first survey was 81%, but decreased thereafter due to aging and increasing morbidity. The latest questionnaire survey was performed in winter 2014 to 950 survivors, and the response rate was 73% (n = 690).
After the postal questionnaire survey in 2002/2003, a random subcohort (n = 650) visited the clinic whereupon Mini-Mental State Examination (MMSE) and laboratory investigations including Apolipoprotein (APO) E genotyping were performed (Citation10).
Mortality 1964–2014
The mortality has been followed-up from the date of baseline measurement between 1964 and 1973 through 31 December 2013. The personal identification number assigned for every resident in Finland was used to link data with the mortality registry (Population Information System). The assessment of vital status is very reliable for people having their permanent place of residence in Finland (over 95% of the present cohort) irrespective of whether they die in Finland or abroad.
Death certificates, dementia, and ASCVD
In winter 2014, death certificates of men who had died between 1 January 1984 and 31December 2013 were retrieved from the Cause-of-Death Registry of Statistics Finland where doctors and hospitals send the death certificates. In addition to cause(s) of death, the death certificates are required to contain a narrative of the decedent’s history, important diseases (such as AD and dementia) and circumstances surrounding death. It was known from earlier analyses that the first death with dementia diagnosis appeared in 1985 when the cohort was 51–66 years old. Diagnosis of dementia is in Finland routinely made by a neurologist or geriatrician – not a general practitioner or any non-specialist – so the diagnosis of dementia in death certificates is very likely to reflect a specialist diagnosis.
A total number of deaths were 1911, but because the sending of death certificates to Statistics Finland lags behind, 26 certificates were not retrieved, and our analytical sample was 1885 (96.5%). First, the certificates were screened for any mention or diagnosis of AD, vascular dementia (VD), dementia, or cognitive (memory) disorders, totaling 365 cases. The certificates were then perused by a geriatrician (T. E. S.) and a neurologist (K. R.) and after consensus categorized into the following groups. (1) Diagnosis of AD without any hint of ASCVD ("pure" AD, n = 93), (2) diagnosis of AD specified either as a cause of death or in the narrative, with any concomitant ASCVD – not only cerebrovascular disease (n = 126), (3) diagnosis of VD specified as a cause of death or in the narrative (n = 82), (4) dementia or memory disorder mentioned in the certificate but not as a specific diagnosis (n = 27), (5) Parkinson disease (PD) as a cause of dementia with or without signs of other types of dementia (n = 15), (6) Lewy body disease (LBD) with or without signs of other types of dementia (n = 14), (7) other specific diagnosis for dementia or memory disorder (n = 8).
The motivation for this categorization was that ASCVD is a systemic disease, and also, for example, coronary artery disease is associated with VD (Citation14). In order to avoid heterogeneity and small numbers, we included in the subsequent analyses the three largest groups, pure AD, AD-ASCVD, and VD.
Because of the gradual development of cognitive impairment (Citation15), exact time of onset is necessarily arbitrary. We used the year of diagnosis if given in the death certificate, or if the year of drug reimbursement for dementia was available; otherwise clinical judgment of the geriatrician and neurologist was used. The distributions of age and onset of dementia are in . Data of survivors through 31 December 2013 and those who had died without known diagnosis of dementia are shown for comparison. The median age of onset was slightly higher in AD-ASCVD than in other groups. The median age of survivors was clearly above the median age of onset of dementia in our cohort.
Table 1. Study groups and types of dementia in the Helsinki businessmen study follow-up.
Diagnosis of dementia in Finland
Since 1989, there have been national guidelines for diagnosis of dementia in Finland, and the first Current Care Guidelines were published in 2004. The diagnosis of dementia is based on the DSM-IV criteria, the probable and possible AD on the NINCDS-ADRDA criteria, and NINDS-AIREN criteria for VD. The NINCDS-ADRDA criteria are known to bias diagnosis toward AD-type dementia (Citation5). In Finland, the initial diagnosis is routinely made by a specialist, usually by a neurologist if the patient is below 65 years, and by a geriatrician or neurologist in persons over 65 years.
Reimbursement for dementia drugs (vide infra) started in February 1999 required a diagnosis made by a specialist, and this has had a nation-wide impact for further harmonizing the diagnosis of cognitive disorders. Therefore, the mention of a cognitive disorder in the death certificate is very likely to reflect a specialist diagnosis.
Drug reimbursement
The Drug Reimbursement Register is maintained by the Finnish Social Insurance Institution and it includes the date, when a patient becomes entitled to a reimbursement for a specified chronic condition. All dementia drugs available in Finland are included in the reimbursement system, which requires diagnosis by a specialist physician [neurologist or geriatrician] and structurized diagnostic procedures (neuropsychological and laboratory tests, and brain imaging) (Citation16). Reimbursement can be given to patients with a diagnosis of AD or AD with vascular features, but also to dementia with Parkinson’s disease.
In the cohort, we have data from the Drug Reimbursement Register for use of dementia drugs, but also for antihypertensive and diabetes drugs up to 31 December 2007. The sensitivity for AD in the register has been reported to be 63.5% and positive predictive value 97.1% (Citation16).
Statistical analyses
Baseline variables were compared using ANOVA (adjusted for age at baseline visit), and post-hoc comparisons assessed by Bonferroni correction. Mortality and dementia rates were based on person years from the first baseline visit until the date of dementia diagnosis, death for any cause, or 31 December 2013, whichever came first. ASCVD risk factors and their dichotomized groups were compared for survival time, and time to dementia diagnosis with Cox proportional hazards model. Hazard ratios (HR) with their 95% confidence intervals (CI) were calculated. The proportionality assumption was considered to be met after visual inspection of the survival curves, but we also evaluated the assumption with Schoenfeld residuals. In the analyses for the specific dementia groups, other dementia groups were excluded and men with specific dementia (e.g., pure AD) were compared with men without diagnosed dementia (dead or alive by 31 December 2013). These analyses were adjusted for age at first visit and all risk factors (smoking, BMI, systolic BP, and cholesterol) were simultaneously (either continuous or dichotomous) in the model. For continuous variables, HR was calculated per SD, and logarithmic values were used for 1-h glucose and triglycerides. For dichotomous values, we used the cutpoints 6.5 mmol/L and 160 mmHg for cholesterol and systolic BP, respectively (Citation17). Cutpoints of 30 kg/m2, and 9.0 mmol/L were used for BMI and 1-h glucose, respectively. Because 1-h glucose was measured in a smaller number of men at baseline (n = 2034), the Cox analyses were performed separately and adjusted for baseline age and smoking only.
Statistical analyses were performed with NCSS version 8.0.2. statistical software (NCSS, Kaysville, UT, www.ncss.com). Significance was defined as 2-sided p <.05.
Results
Midlife characteristics
The baseline characteristics of the study groups in midlife are shown in . Men with pure AD did not differ from of old age survivors without diagnosed dementia, for example, their average cholesterol glucose tolerance and cholesterol values in midlife were similar. In contrast, the AD-ASCVD group had significantly higher cholesterol at baseline.
Table 2. Midlife characteristics of the study cohort according to later dementia type and survival status.
APOE ɛ4 allele and MMSE in the subcohort 2002/2003
In the 2002/2003, random subcohort the APOE ɛ4 allele was found in 31.5% (n = 121 out of 384) of the men who survived through 31 December 2013 without known dementia. The proportions were 42.9% (n= 9 out of 21), 51.4% of the (n = 19 out 37), and 45.5% (n = 5 out of 11) among men with pure AD, AD-ASCVD, and VD, respectively (p = .06 between groups). Age-adjusted MMSE scores in 2002/2003 were 28.5 (SE 0.09), 26.2 (0.4), 27.4 (0.3), and 25.8 (0.6) among the old age survivors, pure AD, AD-ASCVD, and VD groups, respectively (p < .001 between groups).
Drug reimbursement for AD, hypertension, and diabetes
Proportions of men receiving drug reimbursement up to the year 2007 for AD, hypertension and diabetes are in . Men assessed to have pure AD in our current analyses had the highest use of AD drugs (71.0%), and men with VD had the highest use of both hypertension and diabetes drugs. The latter proportions were lower in men with pure AD than in men surviving to old age without known dementia.
Table 3. Proportion of drug reimbursement in study groups.
Predictors of dementia
The predictive value of baseline risk factors (smoking, BMI, systolic BP, and cholesterol) for various dementia types and death without dementia during follow-up are shown in . For each dementia type, the reference group in the Cox analyses was men without diagnosed dementia (dead or alive by 31 December 2013). Both continuous and dichotomous values of all risk factors significantly predicted all-cause mortality without dementia. In contrast, none of the baseline risk factors were significantly associated with pure AD or VD. However, risk of AD-ASCVD was significantly predicted by midlife cholesterol: 24% increase per 1 SD increase in cholesterol. High cholesterol (≥6.5 mmol/L) increased risk by 67% as compared with lower cholesterol level. None of the other risk factors significantly predicted AD-ASCVD or the combination with VD.
Table 4. Risk of incident dementia and death without diagnosed dementia during follow-up according to midlife risk factors.
Because of mixed data on glucose and diabetes in previous studies we studied the impact of 1-h glucose adjusted only for age and smoking to avoid over adjustment (). One-hour glucose significantly predicted mortality without dementia, but did not statistically significantly predict any type of dementia. However, the point estimates were over 1 for AD-ASCVD and VD, but below 1 for pure AD ().
Discussion
An important finding of this long-term follow-up was that in men the development of “pure” AD without ASCVD was not associated with cholesterol level, blood pressure, glucose tolerance, or diabetes. The development of AD with ASCVD, in contrast, was significantly associated with midlife cholesterol. Our results may help to understand previous controversies on the associations between vascular risk factors, diabetes, and dementia in old age.
Some characteristics of our study deserve emphasis. First, we perused detailed death certificates to assess the presence of cognitive and memory disorders thus circumventing non-participation in a clinical study, and lack of cognitive disorder as a specific cause of death. Second, we divided AD diagnosis on death certificates to those with or without history or signs of any concomitant ASCVD. Third, we compared men with various dementia types to those who died or survived to old age without known dementia diagnosis.
Both primarily neurodegenerative and vascular processes contribute to dementia and the overlap of these may confuse researchers and clinicians (Citation1,Citation5–9). The results of the Nun Study were pioneering to widen the scope of old age dementia as a balance between neural and vascular pathology: little AD pathology with much vascular pathology and vice versa may lead to a similar clinical picture of a cognitive disorder (Citation4). The long-term studies have strongly promoted the idea of AD as a vascular state (Citation18) and consequently, sporadic late-onset AD is now considered a potentially preventable condition (Citation19).
However, the diagnosis of old age AD and dementia is predominantly clinical and the prevailing criteria do not discern pathophysiology (Citation1). In our material, half of cognitive dementia in old age had partially vascular etiology (AD-ASCVD plus VD constituted 57% of dementias) and would thus be amenable to prevention. However, vascular risk factors were not related to pure AD, a quarter of dementia cases, and their prevention should be sought elsewhere. Our results highlight the discussion of the repeated failure of the anti-amyloid therapy to retard AD and cognitive decline (Citation20). The trial populations may have had patients with predominantly vascular cause for their dementia.
That cholesterol was associated with the AD-ASCVD and the combined AD-ASCVD plus VD groups in our study is plausible, because cholesterol (specifically low-density lipoprotein [LDL] cholesterol) is the causative, predisposing factor for ASCVD (Citation21). In the brain, ASCVD induces hypoperfusion (Citation14), a risk factor for cognitive impairment, and midlife cholesterol has been shown to predict cognitive disorders in other long-term studies (Citation17,Citation22). Our study emphasizes, however, that midlife cholesterol would not be related to pure AD without signs of ASCVD.
An obvious question then arises why BP and smoking did not increase risk as in some other studies (Citation1,Citation17,Citation23–25). One possibility is competitive mortality. Hypertension and smoking were significant risk factors for mortality in this male cohort () and hypertensive and smoking men may simply not get old enough to develop clinical dementia. Another possibility is the modulation by drug treatment (and smoking cessation), which affect risk factors differently. There are also other studies where hypertension or smoking have not been associated with an increased rate of dementia (Citation22,Citation26).
Our finding that glucose and diabetes were not related to pure AD – but tended to associate with AD-ASCVD and VD – may help to explain some earlier data. Observational studies, where the diagnosis of dementia and AD has apparently included both neurodegenerative and vascular pathologies, have generally indicated a significant connection with glucose, diabetes, and dementia (Citation1–3,Citation8). However, glucose homeostasis may not be related to verified AD pathology. In the Vantaa 85 + study, older individuals with diabetes had more vascular pathology at autopsy, but were less likely to have beta-amyloid or tangles in their brains (Citation27). In the Baltimore Longitudinal Study of Aging, brain beta-amyloid load was not associated with glucose and insulin homeostasis, or frank diabetes (Citation9). A recent, large autopsy study also supported the idea that diabetes is associated with cerebrovascular, but not AD pathology (Citation28). That diabetes may be rare in AD was suggested already during the 1990s (Citation29), and recently reported association between weight loss in midlife and dementia (Citation30) may also offer a mechanism to less diabetes.
Strengths and limitations
The strengths of our study include the long-term follow-up from early midlife to old age and the collection of a relatively large number of endpoints from death certificates, where dementia diagnosis reflects a specialist diagnosis according to national guidelines. The frequency, age of onset and distribution of less frequent dementia types are in line with other epidemiological data of dementia, and subcohort data of MMSE and APOE ɛ4 allele support our categorization. The homogeneity of the cohort reduces confounding due to education and socioeconomic factors, and gives reliability to self-reported data.
The cohort size may be a limitation, although the number of dementias was large comparable to many other studies. The socioeconomic and male selection limit generalizability, and the numbers of men with low risk in midlife were limited, because of the 1960s lifestyle in Finland. Diagnosis of dementia and ASCVD was based on death certificates, which may be incomplete, and the number of survivors through 31 December 2013 with dementia is unknown. These omissions, however, are prone to dilute rather than increase the differences between the diagnostic groups.
Conclusions
Our long-term follow-up showed that of midlife risk factors cholesterol predict old age dementia associated with ASCVD, whereas a role of ASCVD risk factors and glucose tolerance was not observed in pure AD. These findings do not contradict the importance of modifiable ASCVD risk factors in over half of dementia cases, but at least in a quarter of patients with late-onset dementia other types of prevention and treatment must be sought for.
Acknowledgements
The authors would like to thank Hannu Kautiainen, PhD, for statistical advice.
Disclosure statement
None related to this epidemiological study.
Additional information
Funding
References
- Winblad B, Amouyel P, Andrieu S, Ballard C, Brayne C, Brodaty H, et al. Defeating Alzheimer's disease and other dementias: a priority for European science and society. Lancet Neurol. 2016;15:455–532.
- Kloppenborg RP, van den Berg E, Kappelle LJ, Biessels GJ. Diabetes and other vascular risk factors for dementia: which factor matters most? A systematic review. Eur J Pharmac. 2008;585:97–108.
- Exalto LG, Quesenberry CP, Barnes D, Kivipelto M, Biessels GJ, Whitmer RA. Midlife risk score for the prediction of dementia four decades later. Alzheimers Dement. 2014;10:562–70.
- Snowdon DA, Greiner LH, Mortimer JA, Riley KP, Greiner PA, Markesbery WR. Brain infarction and the clinical expression of Alzheimer disease. The Nun Study. JAMA 1997;277:813–17.
- Hachinski V. Shifts in thinking about dementia. JAMA 2008;300:2172–3.
- Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P, et al. Revising the definition of Alzheimer's disease: a new lexicon. Lancet Neurol. 2010;9:1118–27.
- Hachinski V, Sposato LA. Dementia: from muddled diagnoses to treatable mechanisms. Brain 2013;136:2652–6.
- Crane PK, Walker R, Hubbard RA. Glucose levels and risk of dementia. N Engl J Med. 2013;369:540–8.
- Thambisetty M, Jeffrey Metter E, Yang A, Dolan H, Marano C, Zonderman AB, et al. Glucose intolerance, insulin resistance, and pathological features of Alzheimer disease in the Baltimore Longitudinal Study of Aging. JAMA Neurol. 2013;70:1167–72.
- Strandberg TE, Salomaa V, Strandberg AY, Vanhanen H, Sarna S, Pitkälä K, et al. Cohort Profile: The Helsinki Businessmen Study [HBS]. Int J Epidemiol. 2016;45:1074.
- Huohvanainen E, Strandberg AY, Stenholm S, Pitkälä KH, Tilvis RS, Strandberg TE. Association of self-rated health in midlife with mortality and old age frailty: a 26-year follow-up of initially healthy men. J Gerontol A Biol Sci Med Sci. 2016;71:923–8.
- Hyttinen L, Strandberg TE, Strandberg AY, Salomaa VV, Pitkälä K, Tilvis RS, et al. Effect of cholesterol on mortality and quality of life up to a 46-year follow-up. Am J Cardiol. 2011;108:677–81.
- Strandberg TE, Pienimäki T, Strandberg AY, Salomaa VV, Pitkälä KH, Tilvis RS, et al. One-hour glucose, mortality, and risk of diabetes: a 44-year prospective study in men. Arch Intern Med. 2011;171:941–3.
- Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:2672–713.
- Beason-Held LL, Goh JO, An Y, Kraut MA, O’Brien RJ, Ferrucci L, et al. Changes in brain function occur years before the onset of cognitive impairment. J Neurosci. 2013;33:18008–14.
- Solomon A, Ngandu T, Soininen H, Hallikainen M, Kivipelto M, Laatikainen T. Validity of dementia and Alzheimer disease diagnoses in Finnish national registers. Alzheimers Dement. 2014;10:303–9.
- Kivipelto M, Helkala EL, Hänninen T, Laakso MP, Hallikainen M, Alhainen K, et al. Midlife vascular risk factors and Alzheimer's disease in later life: longitudinal, population based study. BMJ 2001;322:1447–51.
- De la Torre J. Vascular risk factors: a ticking time bomb to Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2013;28:551–9.
- Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. 2011;10:819–28.
- Karran E, Hardy J. Antiamyloid therapy for Alzheimer's disease-are we on the right road? N Engl J Med. 2014; 370:377–8.
- Goldstein JL, Brown MS. A century of cholesterol and coronaries: from plaques to genes to statins. Cell 2015;161:161–72.
- Strand BH, Langballe EM, Hjellvik V, Handal M, Næss O, Knudsen GP, et al. Midlife vascular risk factors and their association with dementia deaths: results from a Norwegian prospective study followed up for 35 years. J Neurol Sci. 2013;324:124–30.
- Cataldo JK, Prochaska JJ, Glantz SA. Cigarette smoking is a risk factor for Alzheimer's disease: an analysis controlling for tobacco industry affiliation. J Alzheimers Dis. 2010;19:465–80.
- Shah NS, Vidal JS, Masaki K, Petrovich H, Ross GW, Tilley C et al. Midlife blood pressure, plasma β-amyloid, and the risk for Alzheimer disease: the Honolulu Asia Aging Study. Hypertension 2012;59:780–6.
- Tzourio C, Laurent S, Debette S. Is hypertension associated with an accelerated aging of the brain? Hypertension 2014;63:894–903.
- Doll R, Peto R, Boreham J, Sutherland I. Smoking and dementia in male British doctors: prospective study. BMJ 2000;320:1097–102.
- Ahtiluoto S, Polvikoski T, Peltonen M, Solomon A, Tuomilehto J, Winblad B, et al. Diabetes, Alzheimer disease, and vascular dementia: a population-based neuropathologic study. Neurology 2010;75:1195–202.
- Abner EL, Nelson PT, Kryscio RJ, et al. Diabetes is associated with cerebrovascular but not Alzheimer’s disease neuropathology. Alzheimer Dement. 2016;12:882–9.
- Nielson KA, Nolan JH, Berchtold NC, Sandman CA, Mulnard RA, Cotman CW. Apolipoprotein-E genotyping of diabetic dementia patients: is diabetes rare in Alzheimer's disease? J Am Geriatr Soc. 1996;44:897–904.
- Strand BH, Wills AK, Langballe EM, Rosness TA, Engedal K, Bjertness E. Weight change in midlife and risk of mortality from dementia up to 35 years later. J Geront A Biol Sci Med Sci. 2016;pii: glw157. [Epub ahead of print].