Abstract
Introduction: Identifying Brugada electrocardiographic pattern (BrP) early is crucial to prevent sudden cardiac death. Two different diagnostic criteria proposed by International Society for Holter and Noninvasive Electrocardiography (ISHNE) and Heart Rhythm Society/European Heart Rhythm Association/Asia-Pacific Heart Rhythm Society (HRS/EHRA/APHRS) were widely used in clinical practice. The difference in prevalence and prognosis of BrP by applying the two different criteria was never studied before.
Methods: This study was prospectively conducted in a nationwide large-scale stratified random sampling community-based cohort (HALST) from Han Chinese population in Taiwan from December 2008 to December 2012. We compared the prevalence and prognosis of BrP defined by the two diagnostic criteria.
Results: A total of 5214 adults were enrolled (2530 men) with mean age of 69.3 years. Four had spontaneous type 1 BrP (0.077%). By the HRS/EHRA/APHRS criteria, 68 individuals have type 2 BrP (1.30%) and 101 have type 3 BrP (1.94%) whereas by the ISHNE criteria, 46 individuals exhibited type 2 BrP (0.88%). When applying the ISHNE criteria, the number of individuals with BrP decreased by 71%. However, all-cause mortality and cardiovascular mortality were not different between individuals with or without BrP, irrespective of the criteria used.
Conclusions: The two different criteria may impact the diagnostic yield of individuals with BrP, but do not affect the prognosis of the individuals with BrP.
Comparing with the use of HRS/EHRA/APHRS criteria, the number of individuals with Brugada ECG patterns was decreased by 71% when applying the ISHNE criteria.
The prognosis of individuals with Brugada ECG patterns defined by 2012 ISHNE or 2013 HRS/EHRA/APHRS criteria were not different.
Key messages
Introduction
Brugada syndrome (BrS), which causes sudden cardiac death (SCD) in patients with structurally normal heart, is a disease entity accompanied by arrhythmogenic channelopathy that was first reported by Brugada et al. in 1992 [Citation1]. It is responsible for 4% of all sudden deaths and for up to 20% of sudden deaths in patients without structural cardiac disease [Citation2].
The diagnosis of BrS is mainly based on its unique electrocardiographic (ECG) pattern. One of the definition of Brugada ECG pattern (BrP) was proposed by the Heart Rhythm Society/European Heart Rhythm Association/Asia-Pacific Heart Rhythm Society (HRS/EHRA/APHRS) in 2013 [Citation3], in which type 1 BrP with coved-type ST-segment elevation is diagnostic for BrS, either spontaneous or provoked by drug challenge whereas type 2 and 3 BrP with saddle-back ST-segment elevation can only be used for suspicion of BrS. Although many individuals with type 1 BrP are asymptomatic, they still have annual rate of cardiac events ranging from 0.8% to 2.7% [Citation4–7]. Therefore, understanding the prevalence of Brugada-type electrocardiogram is warranted to prevent SCD by setting up the screening strategy.
In the past two decades, epidemiologic data showed that the prevalence of type 1 BrP of apparently healthy populations is higher in Asia (0.11%) [Citation8–22], followed by Europe (0.018%) [Citation23–31] and Americas (0.015%) [Citation32–36] defined by the second consensus of HRS/EHRA in 2005 (Supplementary Table 1) [Citation37]. In our previous study, we used a nationwide community-based cohort in Taiwan (HALST cohort) to investigate the prevalence and prognosis of BrP defined by HRS/EHRA/APHRS 2013 criteria in elder Han Chinese population [Citation38]. We found that the prevalence of type 1 BrP in adults 55 years and older was similar to the average worldwide prevalence (0.077% vs. 0.07%), but the combined prevalence of type 2 and 3 BrP was significantly higher than the average of the world (3.24% vs. 0.28%). Although the prevalence of type 2 and 3 BrP was higher in Han Chinese population, it was not associated with increased mortality. We wondered if the type 2 and 3 BrP is truly benign in elderly population, or the prognostic value of the BrP may be influenced by applying different diagnostic criteria. Moreover, the differentiation between non-type 1 BrP and incomplete right bundle branch block (ICRBBB) is always challenging, which may contribute to false positivity and overestimate the prevalence of BrP. This problem would be more prominent in elder population since ICRBBB could be caused by degeneration of the conductive system due to the aging process, pulmonary hypertension or prior myocardial injury. Chevallier et al. reported that the r’ angle with a cut-off value of >58° had a sensitivity of 92% and a specificity of 87% for the diagnosis of BrS, and it increased the positive predictive value from 34% to 79% [Citation39]. Furthermore, since type 2 or type 3 BrP alone is not diagnostic, and there is no prognostic difference between the two patterns [Citation2], it is logical to join them in one unique pattern. As a result, International Society for Holter and Noninvasive Electrocardiography (ISHNE) proposed diagnostic criteria in 2012(40) which used the same criteria for the diagnostic type 1 BrP and joined previously defined type 2 and type 3 in 2005 into a new type 2 BrP (saddle-back pattern) with a wide r’ angle.
Currently, both diagnostic criteria are widely used in clinical practice. The difference in prevalence and prognosis of BrP by applying the two different criteria was never studied before. In this study, we compared the difference on the prevalence and prognosis of individuals with BrP defined by the ISHNE criteria with HRS/EHRA/APHRS criteria in a community-based Han Chinese population.
Materials and methods
Study cohort
The Healthy Aging Longitudinal Study in Taiwan (HALST) is an ongoing prospectively community-based longitudinal study of adults aged ≥55 years that began data collection from December 2008. The study is designed to thoroughly examine the determinants of late-life health in a Han Chinese population. Using a stratified random sampling method, a sample of community-dwelling adults with diverse social demographic backgrounds were recruited from multiple areas across Taiwan, including 2 areas in the northern region, 2 in the central region, 2 in the southern region, and 1 in the eastern region (Supplementary Figure 1). Briefly, townships located within 2 km of the study hospital in the geographic areas were stratified by age, gender and education levels, and respondents were selected from each stratum by the system random sampling method. To be eligible, an individual had to be aged ≥55 years. Exclusion criteria included having highly contagious infectious diseases, severe illnesses including malignancy undergoing active treatment, being bed-bound or too frail to stand and ambulate, and being institutionalized or hospitalized. Individuals with severe hearing, speech, mental or cognitive impairments were also excluded because of their inability to answer questions accurately. All individuals provided informed consent prior to participating in the study. After recruitment, all individuals underwent physical performance assessments; interviewer-administered questionnaires including social demographic status, health status and lifestyle factors; and three serial 12-lead ECGs. During the follow-up, the causes of death were recorded by International Statistical Classification of Diseases code, 10th edition. This study protocol was in accordance with the Declaration of Helsinki and was approved by the local ethical committee of Taiwan National Health Research Institutes and participating hospitals.
Electrocardiographic analysis
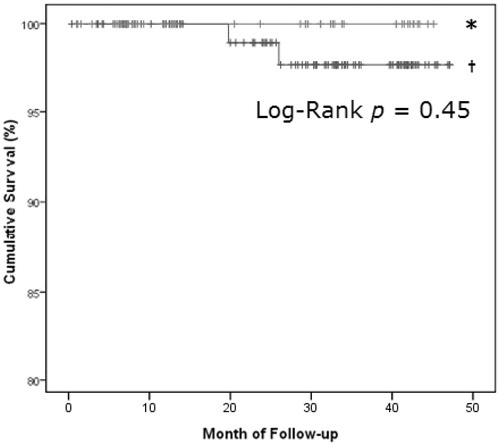
The 12-lead ECGs were recorded in the standard setting of 10mm/mV and 25mm/s, and PR, QRS, and corrected QT interval by Bazett’s formula were computed automatically. We analysed the individuals enrolled between January 2009 and December 2012, and excluded the individuals with complete atrioventricular block, pacing rhythm or poor image quality. Since this prospective study was started from 2008, earlier than the HRS/EHRA/APHRS 2013 expert consensus which suggested upward placement of lead V1-2 to the third and second intercostal space to enhance the diagnostic sensitivity, the lead V1-2 in this study was placed exclusively at the standard position (fourth intercostal space). For the definition of BrP, we used two different criteria adopted currently and analysed, respectively. The first criteria were proposed by the HRS/EHRA/APHRS 2013 expert consensus [Citation3], which analyses right precordial leads (i.e. V1–2) and classifies the patterns into types 1–3 as follows: type 1 BrP has coved-type ST-segment elevation with J point elevation >0.2 mV, followed by a negative T wave; type 2 BrP has saddle-back ST-segment elevation with J point elevation >0.2 mV, followed by a gradually descending ST-segment elevation >0.1 mV and a positive or biphasic T wave; and type 3 BrP has either a saddle-back or coved appearance but with ST-segment elevation <0.1 mV (). The second criteria were the adopted criteria proposed by ISHNE in 2012 [Citation40], which analyse lead V1–2 and redefined BrP into two types as follows: the type 1 BrP (coved pattern) is identical to the classic type 1 BrP; the type 2 BrP (saddle-back pattern) gives a clear definition of the morphology, which has high take-off of r’>2 mm and a minimal ST-segment amplitude of >0.5mm, with a wide angle of r’, defined by a β angle of >58° or the duration of the base of triangle of r’ at 5 mm from the high take-off of >3.5 mm, followed by positive T wave in V2 and variable morphology in V1 (). As a result, the ECG is fitting the HRS/EHRA/APHRS 2013 criteria with a β angle <58° or J point elevation <0.2 mV would be excluded when applying the ISHNE 2012 criteria. Examples of excluded BrP defined by the HRS/EHRA/APHRS 2013 criteria are shown in . All ECGs were analysed and interpreted by two cardiologists independently and blindly.
Figure 1. Comparisons of the HRS/EHRA/APHRS 2013 and ISHNE 2012 Brugada syndrome ECG criteria. (A). HRS/EHRA/APHRS 2013: Type 1 ECG (coved type); type 2 ECG (saddleback type); type 3 ECG (saddleback with ST-segment elevation <1 mm). (B). ISHNE 2012: Type 1 ECG (coved pattern); type 2 ECG (saddleback pattern) with β angle >58°. ECG = electrocardiographic; HRS/EHRA/APHRS = Heart Rhythm Society/European Heart Rhythm Association/Asia-Pacific Heart Rhythm Society; ISHNE = International Society for Holter and Noninvasive Electrocardiography.
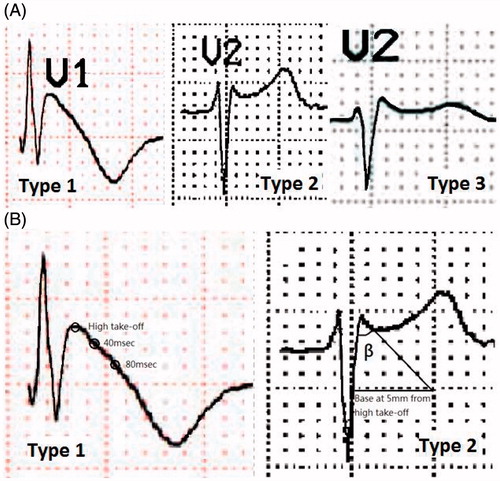
Figure 2. (A). An example of an excluded Brugada-type ECG pattern due to β angle <58° in a 74-year-old woman. (B). An example of an excluded Brugada-type ECG pattern due to J point elevation <0.2 mV in a 66-year-old man. (C). Difference in the numbers of individuals with Brugada-type ECG between 2013 HRS/EHRA/APHRS and 2012 ISHNE criteria. ECG = electrocardiographic; HRS/EHRA/APHRS = Heart Rhythm Society/European Heart Rhythm Association/Asia-Pacific Heart Rhythm Society; ISHNE = International Society for Holter and Noninvasive Electrocardiography.
Statistical analysis
Since HALST is an ongoing population-based longitudinal study started from December 2008, we performed statistical analysis on the collected data from January 2009 to December 2012. Chi-square or Fisher’s exact tests were used to compare categorical variables and Student’s t-tests or one-way analysis of variance were used for continuous variables. All continuous data were expressed as mean ± standard deviation. The annual event rate was evaluated by the number of events occurring during the follow-up period divided by the number of individuals and the average duration of follow-up. Survival curves were plotted by the Kaplan–Meier method, and the log-rank test was used for the comparison of the difference in mortality between individuals with and without BrP. A two-tailed p-value < .05 was considered statistically significant.
Results
Demographic data of the study individuals
After excluding 13 individuals with pacing rhythm, 2 with atrioventricular block, and 1 with poor ECG image quality, 5214 apparently healthy individuals were enrolled (2530 men, 2684 women), with a mean age of 69.3 ± 8 years (men, 69.5 years; women, 69.1 years). Comparisons of demographic data between individuals with or without BrP are shown in . Interestingly, we found that the percentage of patients with hypertension or dyslipidemia was significantly lower among individuals with BrP than those without (all p < .05), irrespective of which criteria were used.
Table 1. Demographic data and clinical outcomes of the study individuals.
Comparisons of BrP defined by HRS/EHRA/APHRS criteria and ISHNE criteria
Four individuals had spontaneous type 1 BrP (0.077%; 3 men, 1 woman) regardless of which criteria were applied. According to the 2013 HRS/EHRA/APHRS criteria, 68 individuals had a type 2 BrP (1.30%; 53 men, 15 women) and 101 individuals had a type 3 pattern (1.94%; 56 men, 45 women), whereas 46 individuals had a type 2 BrP according to the 2012 ISHNE criteria (0.88%, 36 men, 10 women). After applying the 2012 ISHNE criteria, 22 individuals with a previous type 2 BrP and all of the 101 individuals with a type 3 BrP were excluded. As a result, the number of individuals with BrP decreased 71% (). On the other hand, we found that there was a male predominance in the incidence of BrP independent of which criteria were applied (p < .001 for both).
Comparisons of ECG parameters using different diagnostic criteria
Among ECG parameters, the mean QRS duration was significantly longer in the individuals with a BrP as defined by the 2013 HRS/EHRA/APHRS criteria, whereas no difference in mean QRS was noted according to the 2012 ISHNE criteria (p = .003 vs. 0.24, respectively) (). The degree of the P-wave axis was significantly larger in the individuals with a BrP than those without, regardless of which criteria were applied (p < .003 for both).
Table 2. Comparisons of electrocardiographic parameters in the individuals with or without Brugada ECG pattern.
Comparisons of prognoses of individuals with BrP defined by HRS/EHRA/APHRS and ISHNE criteria
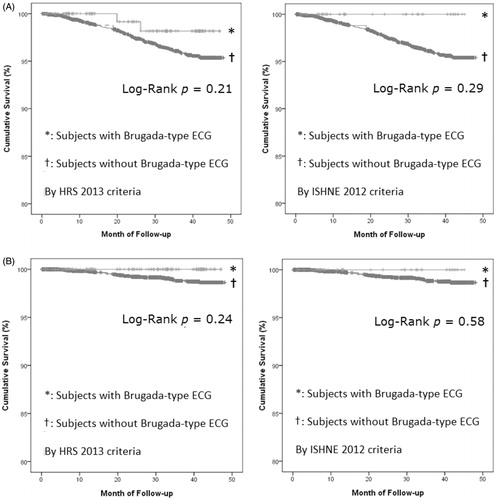
During the 4-year follow-up (median, 40 months), 141 individuals died. Both all-cause and cardiovascular mortalities were not significantly different between individuals with or without BrP regardless of the HRS/EHRA/APHRS or ISHNE criteria were applied ().
Figure 3. Kaplan–Meier survival analysis between individuals with and without Brugada-type ECG patterns according to the criteria proposed by 2013 HRS/EHRA/APHRS and 2012 ISHNE. (A). All-cause mortality. (B). Cardiovascular mortality. ECG = electrocardiogram; HRS/EHRA/APHRS = Heart Rhythm Society/European Heart Rhythm Association/Asia-Pacific Heart Rhythm Society; ISHNE = International Society for Holter and Noninvasive Electrocardiography.
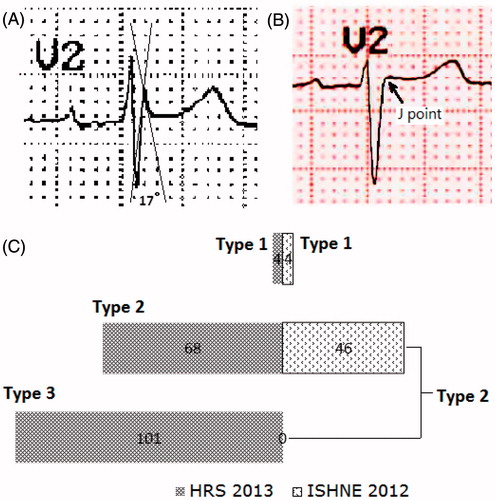
To investigate the prognosis of the individuals who had BrP defined by the 2013 HRS/EHRA/APHRS criteria, but did not fit the 2012 ISHNE criteria, we analysed their clinical outcomes and found that there was no difference between all-cause mortality of the individuals with type 2 BrP by 2012 ISHNE criteria and those excluded (p = .45) (). There was no individual in the two groups dying of cardiovascular reasons.
Discussion
The ECG pattern of BrS is known to be dynamic over time. Using the consensus of BrP proposed by the HRS/EHRA/APHRS, it is difficult to distinguish type 2 and type 3 BrP from ICRBBB. Chevallier et al. [Citation39] enrolled 38 patients with type 2 or type 3 BrP and ICRBBB, and compared the electrocardiographic characteristics between the patients showing type 1 BrP after ajmaline infusion and those who did not. They concluded that the β angle with a cut-off value of >58° had a sensitivity and specificity of 92% and 87%, respectively, and had a positive predictive value of 79% and negative predictive value of 95%. Serra et al. [Citation41] compared 50 BrS patients with type 2 BrP in baseline and 58 healthy athletes with r' wave in V1/V2 and discovered that the β angle at 36.8° cut-off had better diagnostic yield, with a positive predictive value of 93.5% and a negative predictive value of 88.5%. However, it may be inconvenient to measure the β angle in clinical practice. To solve this problem, they also investigated the duration of base of the r’ wave and found that the duration of base of the r’ wave at 5 mm from the high take-off of the QRS ≥160 ms (4 mm) had a sensitivity of 85%, specificity 95.6%, positive predictive value 94.4% and negative predictive value 87.9%, which outperformed the criterion of β angle at 58° cut-off. Although these studies were small-scale and the results needed to be confirmed by a large-scale study, they indeed provided us a useful method to differentiate between non-diagnostic BrP that will turn into a diagnostic type 1 BrP and those that will not [Citation42]. Therefore, the 2012 ISHNE criteria emphasized the importance of using wide β angle and duration of the base of the triangle at 5 mm from r’ wave, which were more strict than the other criteria.
There were explanations for why the number of BrP decreased by 71% after applying the 2012 ISHNE criteria in this study. First, most of the excluded individuals with BrP had a small β angle, with 18 ICRBBBs and 11 CRBBBs, which could be related to comorbidities in elders and high mean age of the HALST cohort. Second, as the prevalence of type 2 BrP (saddle-back pattern) defined by the 2012 ISHNE criteria in this study was comparable to that of other countries [Citation11,Citation15,Citation18,Citation38], this criteria may reduce the confounding effect of age- and/or comorbidities-related RBBB pattern. Therefore, applying the 2012 ISHNE criteria may increase the accuracy of prevalence assessment of BrS in the world.
There were some limitations of this study. The all-cause and cardiovascular mortality were not significantly different between individuals with or without BrP, irrespective of 2013 HRS/EHRA/APHRS or 2012 ISHNE criteria were applied. This result may be influenced by the relatively small number of individuals with BrP, especially type 1 BrP, and the relatively short follow-up time in this study. In addition, the individuals with BrP that remained asymptomatic for more than 55 years might have a relatively lower risk of arrhythmic death, given that the mean age of BrS onset was 41 years [Citation2]. Therefore, these individuals had a similar survival rate as those without BrP.
Conclusions
The prevalence of spontaneous type 1 BrP in a community-based Han Chinese population with a mean age of 69.3 years is 0.077%, higher than that in the western world. After applying the 2012 ISHNE criteria, the number of individuals with BrP was decreased by 71%. However, there was no significant difference in all-cause mortality and cardiovascular mortality between individuals with type 2 BrP defined by the 2012 ISHNE criteria and those with non-type 1 BrP defined by the 2013 HRS/EHRA/APHRS criteria but not meeting the 2012 ISHNE criteria in this study. In both consensuses, type 1 BrP is diagnosed with the same criteria. ISHNE criteria are useful for its simplicity to merge type 2 BrP and type 3 BrP into one new type 2 BrP. We concluded that the two different criteria may impact on the diagnostic yield of individuals with BrP, but did not affect the prognosis of individuals with BrP.
Supplementary_figure_1.tif
Download TIFF Image (549.6 KB)Supplementary_Materials.doc
Download MS Word (767.5 KB)Acknowledgements
We are sincerely grateful to the staff of the Sixth Core Lab, Department of Medical Research, National Taiwan University Hospital for technical support. We also thank the Healthy Aging Longitudinal Study in Taiwan (HALST) individuals who participated in the study and all members of the HALST study group.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. Journal of the American College of Cardiology. 1992;20:1391–1396.
- Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 2005;111:659–670.
- Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013;10:1932–1963.
- Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998;97:457–460.
- Priori SG, Gasparini M, Napolitano C, et al. Risk stratification in Brugada syndrome: results of the PRELUDE (PRogrammed ELectrical stimUlation preDictive valuE) registry. Journal of the American College of Cardiology. 2012;59:37–45.
- Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635–643.
- Delise P, Allocca G, Marras E, et al. Risk stratification in individuals with the Brugada type 1 ECG pattern without previous cardiac arrest: usefulness of a combined clinical and electrophysiologic approach. Eur Heart J. 2011;32:169–176.
- Matsuo K, Akahoshi M, Nakashima E, et al. The prevalence, incidence and prognostic value of the Brugada-type electrocardiogram: a population-based study of four decades. Journal of the American College of Cardiology. 2001;38:765–770.
- Tohyou Y, Nakazawa K, Takenobu H, et al. A survey in the incidence of right bundle branch block with ST elevation among normal population. Jpn J Electrocardiol. 1995;15:223–226.
- Atarashi H, Ogawa S, Harumi K, et al. Three-year follow-up of patients with right bundle branch block and ST segment elevation in the right precordial leads: Japanese Registry of Brugada Syndrome. Idiopathic Ventricular Fibrillation Investigators. J Am Coll Cardiol. 2001;37:1916–1920.
- Miyasaka Y, Tsuji H, Yamada K, et al. Prevalence and mortality of the Brugada-type electrocardiogram in one city in Japan. J Am Coll Cardiol. 2001;38:771–774.
- Furuhashi M, Uno K, Tsuchihashi K, et al. Prevalence of asymptomatic ST segment elevation in right precordial leads with right bundle branch block (Brugada-type ST shift) among the general Japanese population. Heart. 2001;86:161–166.
- Sakabe M, Fujiki A, Tani M, et al. Proportion and prognosis of healthy people with coved or saddle-back type ST segment elevation in the right precordial leads during 10 years follow-up. European Heart Journal. 2003;24:1488–1493.
- Oe H, Takagi M, Tanaka A, et al. Prevalence and clinical course of the juveniles with Brugada-type ECG in Japanese population. Pacing and Clinical Electrophysiology. 2005;28:549–554.
- Tsuji H, Sato T, Morisaki K, et al. Prognosis of subjects with Brugada-type electrocardiogram in a population of middle-aged Japanese diagnosed during a health examination. The American Journal of Cardiology. 2008;102:584–587.
- Ito H, Yano K, Chen R, et al. The prevalence and prognosis of a Brugada-type electrocardiogram in a population of middle-aged Japanese-American men with follow-up of three decades. Am J Med Sci. 2006;331:25–29.
- Shin SC, Ryu HM, Lee JH, et al. Prevalence of the Brugada-type ECG recorded from higher intercostal spaces in healthy Korean males. Circ J. 2005;69:1064–1067.
- Uhm JS, Hwang IU, Oh YS, et al. Prevalence of electrocardiographic findings suggestive of sudden cardiac death risk in 10,867 apparently healthy young Korean men. Pacing and Clinical Electrophysiology. 2011;34:717–723.
- Gervacio-Domingo G, Isidro J, Tirona J, et al. The Brugada type 1 electrocardiographic pattern is common among Filipinos. J Clin Epidemiol. 2008;61:1067–1072.
- Wajed A, Aslam Z, Abbas SF, et al. Frequency of Brugada-type ECG pattern (Brugada sign) in an apparently healthy young population. J Ayub Med Coll Abbottabad. 2008;20:121–124.
- Juang JM, Phan WL, Chen PC, et al. Brugada-type electrocardiogram in the Taiwanese population-is it a risk factor for sudden death? J Formos Med Assoc. 2011;110:230–238.
- Viskin S, Fish R, Eldar M, et al. Prevalence of the Brugada sign in idiopathic ventricular fibrillation and healthy controls. Heart. 2000;84:31–36.
- Letsas KP, Gavrielatos G, Efremidis M, et al. Prevalence of Brugada sign in a Greek tertiary hospital population. Europace. 2007;9:1077–1080.
- Schukro C, Berger T, Stix G, et al. Regional prevalence and clinical benefit of implantable cardioverter defibrillators in Brugada syndrome. International Journal of Cardiology. 2010;144:191–194.
- Sinner MF, Pfeufer A, Perz S, et al. Spontaneous Brugada electrocardiogram patterns are rare in the German general population: results from the KORA study. Europace 2009;11:1338–1344.
- Gallagher MM, Forleo GB, Behr ER, et al. Prevalence and significance of Brugada-type ECG in 12,012 apparently healthy European subjects. International Journal of Cardiology. 2008;130:44–48.
- Pecini R, Cedergreen P, Theilade S, et al. The prevalence and relevance of the Brugada-type electrocardiogram in the Danish general population: data from the Copenhagen City Heart Study. Europace. 2010;12:982–986.
- Bozkurt A, Yas D, Seydaoglu G, et al. Frequency of Brugada-type ECG pattern (Brugada sign) in Southern Turkey. Int Heart J. 2006;47:541–547.
- Blangy H, Sadoul N, Coutelour JM, et al. Prevalence du syndrome de Brugada dans une population de medecine preventive en Lorraine a propos de 35,309 cas. [Prevalence of Brugada syndrome among 35,309 inhabitants of Lorraine screened at a preventive medicine centre]. Archives Des Maladies Du Coeur Et Des Vaisseaux. 2005;98:175–180.
- Hermida JS, Lemoine JL, Aoun FB, et al. Prevalence of the brugada syndrome in an apparently healthy population. Am J Cardiol. 2000;86:91–94.
- Junttila MJ, Raatikainen MJ, Karjalainen J, et al. Prevalence and prognosis of subjects with Brugada-type ECG pattern in a young and middle-aged Finnish population. Eur Heart J. 2004;25:874–878.
- Lee C, Soni A, Tate RB, et al. The incidence and prognosis of Brugada electrocardiographic pattern in the Manitoba Follow-Up Study. The Canadian Journal of Cardiology. 2005;21:1286–1290.
- Monroe MH, Littmann L. Two-year case collection of the Brugada syndrome electrocardiogram pattern at a large teaching hospital. Clin Cardiol. 2000;23:849–851.
- Greer RW, Glancy DL. Prevalence of the Brugada electrocardiographic pattern at the Medical Center of Louisiana in New Orleans. J La State Med Soc. 2003;155:242–246.
- Donohue D, Tehrani F, Jamehdor R, et al. The prevalence of Brugada ECG in adult patients in a large university hospital in the western United States. Amer Heart Hosp J. 2008;6:48–50.
- Patel SS, Anees S, Ferrick KJ. Prevalence of a Brugada pattern electrocardiogram in an urban population in the United States. Pacing and Clinical Electrophysiology. 2009;32:704–708.
- Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference. Heart Rhythm. 2005;2:42940.
- Juang JM, Chen CY, Chen YH, et al. Prevalence and prognosis of Brugada electrocardiogram patterns in an elderly Han Chinese population: a nation-wide community-based study (HALST cohort)dagger. Europace. 2015;17(Suppl 2):ii54–ii62.
- Chevallier S, Forclaz A, Tenkorang J, et al. New electrocardiographic criteria for discriminating between Brugada types 2 and 3 patterns and incomplete right bundle branch block. Journal of the American College of Cardiology. 2011;58:2290–2298.
- Bayes de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. Journal of Electrocardiology. 2012;45:433–442.
- Serra G, Baranchuk A, Bayes-De-Luna A, et al. New electrocardiographic criteria to differentiate the Type-2 Brugada pattern from electrocardiogram of healthy athletes with r'-wave in leads V1/V2. Europace. 2014;16:1639–1645.
- Postema PG. Are we able to predict the diagnosis of Brugada syndrome? Europace. 2014;16:1543–1545.