Abstract
Objective
To compare disability changes measured with the Respiratory ICF Maugeri core set on COPD patients, recovering from acute exacerbation with and without hospitalization, submitted to pulmonary rehabilitation (PR).
Materials and methods
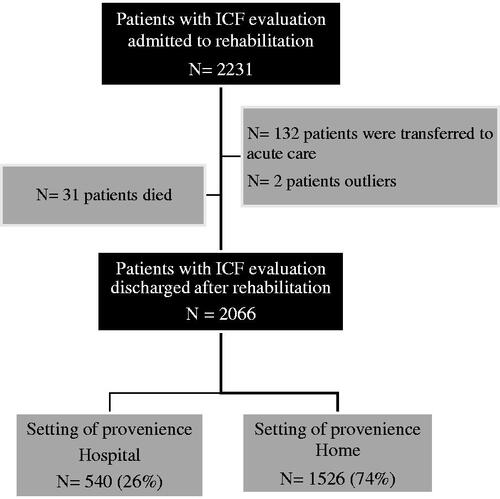
All COPD inpatients admitted for rehabilitation in 9 Respiratory Units (January–August 2019) were considered eligible. 2066 patients were included (540 discharged from an acute Hospital = Hospital group and 1526 coming from their home = Home group). Healthcare professionals filled, in a digitalized chart, the Respiratory ICF Maugeri core set (26 items), assessing ICF categories at admission and discharge.
Results
The baseline distribution of the more severe ICF qualifiers was higher in the Hospital group (p < .001) when compared to the Home group. After rehabilitation, all patients -irrespective of hospitalization need- statistically decreased the rate of the higher ICF qualifiers (p < .0001). Hospital group improved more both the rate of qualifiers ≥2 [Δ: −21.32 (22.41) vs −15.48 (17.32), p < .001] and the rate of qualifiers 0–1 [Δ: + 18.38 (24.67) vs 13.25 (19.13), p < .001] than Home group.
Conclusions
Disability measured with the “Respiratory ICF Maugeri core set” after PR improves in COPD patients recovering from acute exacerbation irrespective of hospitalization need. Its use an additional outcome remains to be further elucidated.
Routine implementation of an ICF set for chronic respiratory diseases can enhance a patient-centered approach in rehabilitation for different severity conditions.
Pulmonary rehabilitation (PR) seems to improve global disability measured with the Respiratory ICF Maugeri core set in COPD patients recovering from acute exacerbation irrespective of hospitalization need, suggesting the use of ICF set as additional PR outcome.
The description, through the ICF language, of rehabilitative needs of patients, coming "from-Home" and "from-Hospital" settings, could help staff and instrument organization.
KEY MESSAGES
Introduction
Rehabilitation has been claimed to be the core health strategy of the twenty first century [Citation1,Citation2].
Pulmonary rehabilitation (PR) is recognized as an evidence-based treatment in improving dyspnoea and quality of life in patients with COPD. PR is very effective with a very low "number needed to treat" (i.e. about 2), irrespective of the severity of COPD [Citation3].
PR has strong evidence of effectiveness in COPD with stable disease [Citation4] or recovering from an exacerbation of COPD (AECOPD) [Citation5], while the reduced risk of mortality at 1 year [Citation6].
Well-established outcomes e.g. 6MWD, MRC score, CAT score, and Barthel index have been proposed to test the efficacy of PR [Citation7].
The International Classification of Functioning, Disability, and Health (ICF) [Citation8] sets represents a new methodological standard for the functioning (organs and diagnosis involved), disability (symptoms and signs), social participation restriction, and environment interaction assessment intending to provide interdisciplinary, holistic and patient-oriented interventions [Citation9]. In practice, at iso-functional impairment, patients present a huge variability of disability and participation needs: ICF classification could be informative about the effect of chronic and acute diseases on individual and help to develop a more comprehensive treatment plan in the rehabilitation setting [Citation8,Citation9] to merge and not to replace well noted specific outcomes.
Our rehabilitative Maugeri network has identified different rehabilitation-based Cardio-Respiratory ICF sets integrating evidence from literature, information gathered from a Clinical Care Pathway (CCP) that implemented routine situations, and input from clinical experts [Citation10,Citation11]. The real-life application of this ICF classification has represented a valid background framework supporting the interdisciplinary nature of functioning itself to improve each step of the rehabilitation cycle [Citation10,Citation11].
Recently we have also shown a large implementation of a PR program based on the Respiratory ICF Maugeri core set discriminating the level of disability in different chronic respiratory diseases to enhance a patient-centered approach in rehabilitation [Citation12]. The Respiratory ICF Maugeri core set administered at admission provided a tailored rehabilitation program according to an interdisciplinary and holistic perspective [Citation13]; re-evaluation at discharge could assess improvements in functions pre to post-rehabilitation.
The present study aimed to test responsivity and to compare disability changes measured with the Respiratory ICF Maugeri core set on COPD patients, recovering from acute exacerbation with and without hospitalization, submitted to pulmonary rehabilitation (PR).
Materials and methods
Population
This study was conducted on the Automated Integrated Health Care Record database of patients with COPD, consecutively admitted for in-hospital PR program after an AECOPD between January the first and 30th August 2019 to the hospitals of ICS Maugeri, Italy (Institutes of Pavia Veruno, Tradate, and Lumezzane), referral institutions for PR program, diagnosis and care of chronic patients (). Diagnosis and severity of COPD were confirmed by spirometry according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines [Citation14].
Patients were divided according to their anamnestic history before rehabilitation admission: Hospital group = patients discharged from an acute hospital and Home group = patients proposed to PR from the territory without acute hospital admission. Patients with less than 6 days and more than 90 days of rehabilitative stay were excluded because of clear outliers.
Patients gave written informed consent to use data for research at the time of hospital admission. The study was approved by the ICS Maugeri Local Review Board (Technical and Scientific Committee).
Intervention
At the time of rehabilitative in-hospital admission, each patient received a multidisciplinary pulmonary rehabilitation program (PRP) according to the Clinical Care Pathway (CCP) [Citation7]. A multidisciplinary team consisting of chest physicians, nurses, physiotherapists, dieticians, and psychologists offered care. Our in-patient multidisciplinary program included the optimization of drug therapy, education, nutritional programs, and psychosocial counselling when appropriate, and at least 22 sessions for 3–4 weeks, of supervised incremental exercise training according to Maltais et al. [Citation15], until performing 30 min of continuous cycling at 50–70% of the maximal load calculated based on the baseline 6MWD according to Luxton et al. [Citation16]. Peripheral limb muscle activities, shoulder, and full arm circling were also performed. Supplemental oxygen for patients under LTOT and interval training for most compromised patients weredelivered. Pulse oximetry and rate, and arterial blood pressure were monitored during exercise. The total daily time duration of activities was 2–3 h.
Measures
At admission and discharge, patients underwent evaluations of routine as a standard haematologic test, blood chemistries and gas analysis, lung function tests, chest X-ray, effort tolerance by 6-minutes walking distance (6MWD) test [Citation17], questionnaire on respiratory symptoms (CAT score) [Citation18], MRC score [Citation19], Barthel dyspnoea score [Citation20–21] and comorbidities with CIRS score [Citation22].
The global impairment of patients was measured through the ICF language, according to the ICF qualifiers and to the linking procedure previously achieved [Citation8,Citation9]. The comprehensive ICF core set can collect more information and it is indicated to guide multidisciplinary assessments in the rehabilitation process [Citation23]. In particular, the Respiratory ICF Maugeri core set used in the study refers to a selection of 26 items defining a respiratory set among the ICF components of body functions (b letter) and activity and participation factors (d letter) (). It has been previously published [Citation10] and here is briefly described.
Table 1. Respiratory ICF Maugeri core set.
The ICF language and the respiratory ICF Maugeri core set
The respiratory ICF Maugeri core set follows the ICF categories which are designated by specific letters, i.e. “b” for Body functions, “s” for Body structures, “d” for Activities and participation, and “e” for Environmental factors. These categories are followed by a numeric code (ICF code) which the first digit represents the ICF chapter number. Further details are given through adding a second (two digits), third and fourth levels (one digit each). The qualifier scale of the ICF factors component (ICF qualifiers) ranged from 0 to 4, according to the increasing severity of the problem (0 no influence, 1 mild, 2 moderate, 3 severe, and 4 complete). Additionally, qualifiers “8 – not specified’’ and “9 – not applicable’’ were used when the available information was not sufficient to quantify the severity of the problem, or when a category did not apply to a specific patient, respectively. Specific ICF categories/codes were previously selected for the Respiratory ICF Maugeri core according to an internal consensus process, either by recoding the established pulmonary rehabilitation outcome measures or, if the first option was not possible, by applying a semi-quantitative methodology [Citation10] (see ).
At the time of admission and discharge, each healthcare professional (pulmonologist, physiotherapist, nurse, psychologist, occupational therapists) had to fill in the ICF, for each inpatient, using a two-step digitalized chart: (a) at admission, to identify the personalized rehabilitation project as well as the critical areas from a clinical point of view; (b) at discharge, to assess changes in functioning according to the ICF qualifiers expressed on the ICF categories. The relative frequency of each ICF qualifier was expressed as the percentage of click “yes” calculated on each patient. The final ICF qualifier was described by the mean of the percentage of clicks “yes” in each level of severity (qualifiers from zero to 4), independently from the ICF category. Moreover, to compare ICF changes observed in a different setting, we defined low ICF severity levels (0 and 1) and higher severity level (≥2), thus cumulative % of click yes for ICF qualifier 0–1 and ≥2 were calculated as well.
Data analysis
Data were analysed by specific software (STATA 13, Stata Corp LP TX, USA). Continuous variables were shown by mean (standard deviation), while binary and categorical variables by percentage. The degree of functioning impairment evaluated by ICF before and after rehabilitation was calculated as percentage of clicks “yes” in each level of severity and pre-to-post difference tested by paired t-test. The analysis was performed on the whole group of patients admitted to rehabilitation, and according to 2 different settings of provenience: patients needing previous hospital admission = Hospital group and patients proposed to PR from the territory = Home group. Comparisons between the 2 different settings of provenience were assessed by unpaired t-test: (1) on the same ICF qualifier (percentage of clicks “yes”) at admission and discharge for each setting; (2) on the pre-to-post difference (Δ) calculated on the cumulative percentage of clicks “yes” for ICF qualifiers ≥2 (high severity) and cumulative percentage of clicks “yes” for ICF qualifiers 0–1 (low severity). For all tests, p was considered significant for value <.05
Results
As shown in , during the study period, 2231 COPD inpatients were admitted to the respiratory units. Thirty-one patients died during the study period, while 132 were transferred to acute care, 2 patients were excluded as outliers. The final analysis was conducted on 2066 survived patients who completed the PR program: 540 of them came from the hospital (due to their need of assistance) and 1526 patients came from their homes. shows the characteristics of the studied patients considering usual evaluations and cumulative ICF qualifiers: as expected, the patients coming from Hospital presented worse values for Barthel dyspnoea, 6MWDT, CAT, MRC, a longer LOS, and a parallel worse global disability according to a higher percentage of click “yes” in ICF qualifiers ≥2.
Table 2. Characteristics of patients at admission.
The whole group improved 6MWD, CAT, MRC, and Barthel Dyspnoea score of 58 ± 94 metres, −7.1 ± 4.6 points, −0.93 ± 0.91, and −11.9 ± 11.4 points respectively. Patients with previous acute hospitalization (Hospital group), when compared to patients without acute hospitalization (Home group), significantly improved 6MWD (83.6 ± 79.9 vs 48.4 ± 97.8, p < .0001), Barthel Dyspnoea score (–14.72 ± 13.20 vs −10.89 ± 10.54, p < .0001), CAT score (–7.72 ± 4.27 vs −6.93 ± 4.75, p = .0255) and MRC score (–1.07 ± 0.99 vs −0.87 ± 0.86, p = .0006).
shows the frequency distribution of the single qualifiers severity rating (from zero to four) chosen by healthcare professionals (HP) on the entire Respiratory ICF set available: Panel “a” shows the percentage of clicks “yes” performed by HP in the whole patients, Panels “b” and “c” represent respectively the percentage of clicks in the Home group and the Hospital group, both at admission (white bars) and discharge (black bars) from rehabilitation.
Figure 2. Frequency distribution of the ICF qualifiers severity ratings (from zero to four) chosen by healthcare professionals (HP) on the entire Respiratory ICF set available, in the whole sample of patients, admitted to rehabilitation (Panel a), coming from Home (Panel b) and Hospital (Panel c). White bars refer to ICF qualifiers at admission (pre) and black bars refer to those at discharge (post). Paired T-test between data at admission and discharge was performed and statistical significance was reported: * indicates p < .0001 and ° p < .05.
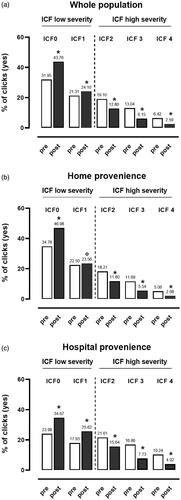
Both at admission and discharge, the distribution of single ICF qualifiers was statistically different between Hospital and Home groups being in the Hospital group lower for the qualifier 0 and 1 and higher for qualifiers ≥ 2 (all p < .001).
After rehabilitation, all patients -irrespective of their hospitalization need- statistically increased the rate of ICF qualifiers 0 and 1 (low severity, p < .0001) and decreased the rate of the higher ICF qualifiers (high severity ≥2; p < .0001). The Hospital group improved more both the rate of cumulative ICF qualifiers ≥2 [Δ: −21.32 (22.41) Hospital vs −15.48 (17.32) Home, p < .001] and the rate of cumulative ICF qualifiers 0 and 1 [Δ: + 18.38 (24.67) Hospital vs 13.25 (19.13) Home, p < .001] than Home group, showing a positive effect of the clinical intervention on patients’ disability.
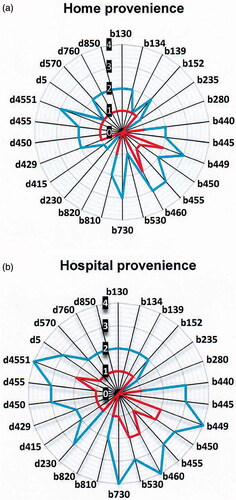
Details on the frequency (shown as mode value) of the 26 ICF codes, as chosen by health staff, at baseline assessment and after rehabilitation have been represented in in the two setting of provenience: Home (panel a) and Hospital group (panel b).
Discussion
An in-patient PRP clinically improved International Classification of global Functioning disability in a huge cohort of patients recovering from AECOPD, independent of their severity as assessed by the need of acute hospitalization. However, acute hospital admission influenced the magnitude of PRP success.
The ICF ontology, differently from the already established outcome measures for pulmonary rehabilitation, is not disease-specific, therefore it allows a more fluid and intelligible exchange of information among pulmonary rehabilitation specialized health care professionals and health care professionals working on the territory [Citation24]. Integrated care is still considered a difficult and complex issue for health care and ICF could smooth the process by sharing a common language, facilitating the comparative evaluation of changes in functioning and standardizing the reports on rehabilitation interventions [Citation25].
The patient’s functioning information, thanks to the joint use of the ICD diseases classification and International Classification of Functioning frameworks, could play a crucial role in rehabilitation medicine, aligning patient care with evidence-based guidelines, optimizing the workflows, and facilitating healthcare benchmarking [Citation26]. The development of an International Classification Functioning core set for COPD involved a series of formal decision-making and consensus processes that incorporate the results of preliminary research, including Delphi expert consultation [Citation10,Citation11].
A brief and comprehensive International Classification Functioning core set for chronic obstructive pulmonary disease (COPD) was established in 2004 and has been proven to be a comprehensive framework covering the symptoms and functions of patients with COPD and a useful tool for measuring their health [Citation27].
The “activity and participation” of brief International Classification Functioning core sets for COPD has been demonstrated to present good reliability and validity to test the daily activities of patients with COPD [Citation28].
Although these important methodological studies, no robust data have been presented on the routine implementation of an International Classification Functioning set for chronic respiratory diseases to enhance a patient-centered approach in rehabilitation. As previously shown [Citation10–13], our respiratory International Classification Functioning set explored different and multidisciplinary disability items as energy, sleep, mental, emotional, muscles, exercise tolerance, straight, ADLs, self-care in adjunction to specific cardio-respiratory disabilities. The COPD population studied was aged, disabled with important symptoms as dyspnoea, with reduced effort tolerance and significant impact on the quality of life as demonstrated by traditionally used tests. Our study shows that this identified International Classification Functioning set in COPD patients – which were recovering from exacerbation, having different severity with or without hospitalization need – is applicable and responsive; in this manner our team assessed with usual items combined to the global functional assessment measured with the International Classification Functioning classification. It is interesting to note that, at admission, in the 38.6% of cases International Classification Functioning qualifiers were ≥ 2 indicating a severe global impairment: as expected, the group of patients with acute hospitalization before rehabilitation presented more frequently qualifiers ≥ 2 in the International Classification Functioning set (48.7% click yes).
The responsiveness of global disability to PR program has been demonstrated by the important reduction of the rate of International Classification Functioning qualifiers ≥ 2 in all sample, in particular in the Hospital group.
Practical implications
The study described how a routine implementation of an International Classification Functioning set for chronic respiratory diseases, based on a comprehensive biopsychosocial function model and standardized descriptions of function and disability, can enhance a patient-centered approach in rehabilitation for different severity conditions. The use at admission and discharge of this International Classification Functioning set to classify patients guided a rehabilitation program according to an interdisciplinary perspective and could be an additive PR outcome measure. The ICF implementation implies in its essence the necessity to be interdisciplinary adopted since it encompasses codes and area of assessment which are covered by different expertise within the rehabilitation team. This holistic view gives separated “silos” but following a clinical care pathway where the patient is at the centre. By describing a patient’s disability through the ICF ontology, clinicians have the unique possibility to share within the team not a fragmented patient but a person with impairments and strengths, limitations, and resources.
Study limitations
Like all retrospective studies, it suffers from missing data. Therefore, we included only International Classification Functioning set data as primary outcomes.
Conclusion
Disability, measured with the “Respiratory International Classification Functioning Maugeri core set” after pulmonary rehabilitation, improves in COPD patients recovering from acute exacerbation irrespective of acute hospitalization need. Its use as an additional PR outcome remains to be further elucidated.
Author contributions
MV and AG contributed to the design of the study; MV, LC, and AO wrote the original draft preparation; GC performed electronic reporting; MP performed statistical analysis; LC performed graphical representation. All authors discussed the results and commented on the manuscript. All authors revised and approved the final draft of the manuscript.
Acknowledgments
The Authors thank Piero Ceriana, Maria Aliani, Bruno Balbi, Claudio Fracchia, Mauro Maniscalco, Francesco Fanfulla, Antonio Spanevello for their clinical support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data available on request from the authors.
Additional information
Funding
References
- Stucki G, Bickenbach J, Gutenbrunner C, et al. Rehabilitation: the health strategy of the 21st century. J Rehabil Med. 2018;50(4):309–316.
- Scrutinio D, Giardini A, Chiovato L, et al. The new frontiers of rehabilitation medicine in people with chronic disabling illnesses. Eur J Intern Med. 2019;61:1–8.
- Riario-Sforza GG, Incorvaia C, Paterniti F, et al. Effects of pulmonary rehabilitation on exercise capacity in patients with COPD: a number needed to treat study. Int J Chron Obstruct Pulmon Dis. 2009;4:315–319.
- Wedzicha JA, Bestall JC, Garrod R, et al. Randomized controlled trial of pulmonary rehabilitation in severe chronic obstructive pulmonary disease patients, stratified with the MRC dyspnoea scale. Eur Respir J. 1998;12(2):363–369.
- Clini EM, Crisafulli E, Costi S, et al. Effects of early inpatient rehabilitation after acute exacerbation of COPD. Respir Med. 2009;103(10):1526–1531.
- Lindenauer PK, Stefan MS, Pekow PS, et al. Association between initiation of pulmonary rehabilitation after hospitalization for COPD and 1-year survival among medicare beneficiaries. JAMA. 2020;323(18):1813–1823.
- Vogiatzis I, Rochester CL, Spruit MA, et al. Increasing implementation and delivery of pulmonary rehabilitation: key messages from the new ATS/ERS policy statement. Eur Respir J. 2016;47(5):1336–1341.
- Organization. WH. The international classification of functioning, disability & health. 2001.
- Stucki G, Ewert T, Cieza A. Value and application of the ICF in rehabilitation medicine. Disabil Rehabil. 2002;24(17):932–938.
- Giardini A, Vitacca M, Pedretti R, et al. [Linking the ICF codes to clinical real-life assessments: the challenge of the transition from theory to practice]. Giornale italiano di medicina del lavoro ed ergonomia. 2019;41(2):78–104.
- Giardini A, Traversi E, Paneroni M, et al. Cardio-respiratory International Classification of Functioning, Disability and Health sets for inpatient rehabilitation: from theory to practice. Eur J Phys Rehabil Med. 2020;56(2):252–254.
- Vitacca M, Giardini A, Corica G, et al. Implementation of a real-world based ICF set for the rehabilitation of respiratory diseases: a pilot study. Minerva Med. 2020;111(3):239–244.
- Lastoria C, Bido S, Ceriana P, et al. [Implementation of the ICD-ICF model in rehabilitation medicine: report of a clinical case in respiratory rehabilitation]. Giornale italiano di medicina del lavoro ed ergonomia. 2019;41(2):150–155.
- 2018 Global strategy for prevention, diagnosis, and management of COPD; [cited 2019 Jan 1]. Available from: http://goldcopd.org/gold-reports/.
- Maltais F, LeBlanc P, Jobin J, et al. Intensity of training and physiologic adaptation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997;155(2):555–561.
- Luxton N, Alison JA, Wu J, et al. Relationship between field walking tests and incremental cycle ergometry in COPD. Respirology. 2008;13(6):856–862.
- Rasekaba T, Lee AL, Naughton MT, et al. The six-minute walk test: a useful metric for the cardiopulmonary patient. Intern Med J. 2009;39(8):495–501.
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654.
- Fletcher CM. Standardized questionnaire on respiratory symptoms: a statement prepared and approved by the MRC Committee on the Aetiology of Chronic Bronchitis (MRC breathlessness score). Br Med J. 1960;2(5213):1665–1666.
- Vitacca M, Paneroni M, Baiardi P, et al. Development of a Barthel Index based on dyspnea for patients with respiratory diseases. Int J Chron Obstruct Pulmon Dis. 2016;11:1199–1206.
- Vitacca M, Malovini A, Balbi B, et al. Minimal clinically important difference in Barthel index dyspnea in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2020;15:2591–2599.
- Parmelee PA, Thuras PD, Katz IR, et al. Validation of the cumulative illness rating scale in a geriatric residential population. J Am Geriatr Soc. 1995;43(2):130–137.
- Cieza A, Ewert T, Ustün TB, et al. Development of ICF Core Sets for patients with chronic conditions. J Rehabil Med. 2004;36(0):9–11.
- Spoorenberg SL, Reijneveld SA, Uittenbroek RJ, et al. Health-related problems and changes after 1 year as assessed with the geriatric ICF core set (GeriatrICS) in community-living older adults who are frail receiving person-centered and integrated care from embrace. Arch Phys Med Rehabil. 2019;100(12):2334–2345.
- Stucki G, Pollock A, Engkasan JP, et al. How to use the international classification of functioning, disability and health as a reference system for comparative evaluation and standardized reporting of rehabilitation interventions. Eur J Phys Rehabil Med. 2019;55(3):384–394.
- Stucki G, Bickenbach J. Functioning information in the learning health system. Eur J Phys Rehabil Med. 2017;53(1):139–143.
- Stucki A, Stoll T, Cieza A, et al. ICF Core Sets for obstructive pulmonary diseases. J Rehabil Med. 2004; 36(0):114–120.
- Guo C, Liu Y, Hao S, et al. The reliability and validity of the “activity and participation” component in the brief ICF core set for chronic obstructive pulmonary diseases based on rasch analysis. COPD. 2020;15:1191–1119.