Abstract
Objectives
To evaluate the effectiveness of repetitive thoracic paravertebral block (TPVB) under ultrasound (US) guidance for acute pain associated to herpes zoster (HZ) and its prophylactic effects on post-herpetic neuralgia (PHN).
Methods
Patients who suffered from acute pain associated to HZ within 1 week of rash onset were randomized in a ratio of 1:1 to receive a seven-day course antiviral therapy, antiviral therapy with additional US-guided repetitive TPVB using transverse short axial (TSA) approach every 48 h for a week after antiviral therapy. All patients were allowed to receive rescue analgesics. The primary endpoint was HZ burden of illness (HZ-BOI) measured by a severity-by-duration composite pain assessment conducted 1-month post inclusion. Adverse events were also recorded.
Results
A total of 96 patients completed the entire 6-month follow-up. The BOI-30AUC was 112.5 (95%CI: 105.2, 119.9) in control group, and 82.7 (95%CI: 75.4, 90.1) in TPVB group (F = 32.252, p<.001) at D30 after inclusion. Compared with control group, significant reductions of BOI-30–90AUC, and BOI-90–180AUC were observed in TPVB group (F = 11.392, p=.001 at D90; F = 7.467, p=.007 at D180, respectively). At 3 and 6 months after inclusion, the incidence of PHN in TPVB group was significantly lower than control group. Quality of life (QoL) in TPVB group also showed greater improvements at all the time points in all domains of EQ-5D-3L (p<.05). No serious adverse events were observed.
Conclusions
US-guided repetitive TPVB significantly reduced the HZ-BOI and the PHN incidence compared to antiviral therapy alone. It might be considered as an early intervention and preventive strategy to the development of PHN after acute HZ.
This is a prospective randomized comparative study. We made a hypothesis that US-guided repetitive thoracic paravertebral block (TPVB) using a transverse short axial (TSA) approach to treat thoracic herpes zoster (HZ) in acute phase could reduce the burden of illness associated to acute pain. Moreover, this therapy might be a feasible preventive strategy to reduce the incidence of post-herpetic neuralgia.
KEY MESSAGE
Introduction
Herpes zoster (HZ) which is characterized by a unilateral dermatomal vesicular rash accompanied with acute pain usually results from a reactivation of varicella zoster viruses (VZV) after the primary infection referred to as childhood “chickenpox”. It is estimated that the incidence of HZ is from to 3 to 5/1000-person years (PY) in North America, Europe and Asia-Pacific with a sharp increase post 60 years of age to 6–8/1000-PY [Citation1,Citation2]. Thoracic dermatome is reported as the most frequent area affected by HZ [Citation3]. During the prodromal or acute phases of HZ, lots of patients suffered from moderate to severe pain which diminished quality of life and induced heaven burden of illness (BOI). Therefore, a plan that optimizes pain relief should be pursed to improve functional status and health-related quality of life when treating zoster-associated pain (ZAP).
Post-herpetic neuralgia (PHN) is the most common and debilitating complication of HZ which occurs when ZAP persists for more than 90 days after rash onset [Citation4]. Most patients recognized the intensity of neuropathic pain as severe enough to affect quality of daily life and cause the largest HZ-related BOI. Despite the widespread use of antiviral drugs and analgesics, a large percentage of HZ patients with potentially high risk factors progressed to the PHN stage, such as age >50 years, number of lesions >50, moderate-to-severe pain in prodromal or acute phases.
It is believed that a progress of acute pain and inflammation during the acute HZ phase are responsible for the intractable sensation [Citation5]. Therefore, the early-onset of supplemental intervention to control acute ZAP has the benefit of attenuating central sensitization and preventing PHN [Citation6]. Paravertebral nerve block has been proved to be effective in providing relief of ZAP and likely plays a role in reducing the incidence of PHN compared to the standard antiviral treatment standalone [Citation7,Citation8]. Moreover, a comparative study has showed that US-guided nerve block is more accessible than the fluoroscopy-guided nerve block and might be an alternative option for HZ [Citation9]. In this study, we conducted a prospective randomized comparison to test whether antiviral therapy combined with US-guided repetitive thoracic paravertebral block (TPVB) using the transverse short axial (TSA) approach in the treatment of HZ may have dual roles in acute pain reduction and prevention of PHN.
Methods
Study design and setting
This prospective randomized clinical trial with 6-month follow-up compared antiviral therapy to standard antiviral therapy along with US-guided repetitive TPVB using TSA approach for the treatment of thoracic HZ. It was conducted in the anaesthesiology department of the Heilongjiang Red Cross Sengong General Hospital, Harbin, China, between 1 January 2019 and 31 December 2020 (). The protocol of the study was approved by Scientific Research Ethics Committee of Hospital. Written informed consent was obtained in all recruits. The study has been registered in the Chinese Clinical Trial Registry (ChiCTR 2100044335).
A total of 100 eligible patients were randomly assigned to one of the following treatment groups. Groups are control group: (patients received a standard seven-day course antiviral therapy with famciclovir 500 mg three times daily immediately after recruitment at the onset of the viral disease) [Citation10], TPVB group: patients were allocated to receive the same standard antiviral therapy as the control group. Additionally, they received repetitive TPVB injections under US guidance by TSA approach with a mixture of lidocaine 20 mg + triamcinolone 5 mg + normal saline 5 ml in total for each involved nerve root every 48 h for a week (total four injections) after the seven-day course antiviral therapy.
Patients
Inclusion criteria were (1) diagnosed as HZ in the thoracic dermatomal; (2) presented to our pain clinic within 1 week from the initial onset of HZ rash; (3) 50 years or older; (4) complete the whole TPVB injection therapy; (5) follow-up using the routine guideline; (6) complete medical record data. Patients were excluded if they had immunity dysfunction, hepatic or renal dysfunction, coagulation disorders, systemic use of antivirals and pregnancy/lactation.
Randomization and masking
The randomization was performed with a web-based system so that patients were enrolled before the treatment assignment was revealed. Allocation was stratified in permuted blocks of four with a ratio of 1:1 by Statistical Software Stata 10.0 module Ralloc version 3.5.2 (StataCorp, College Station, TX), and masked from any individuals participating in the study. Investigators assessing outcomes and those analysing data were masked in the study.
Procedure
All procedures were performed in outpatient operating room under the ultrasound (US) guidance by the same skilled pain physicians who demonstrate expertise in performing US-guided TPVB. Electrocardiography, blood pressure and oxygen saturation monitoring were applied. Patients were in the lateral position with the affected side facing upward. A low-frequency convex array probe (Philips iU22 DS; Philips Medical Systems, Cleveland, OH) was applied transversely to the targeted lateral aspect of the thoracic spinous process. In the short axis view of the thoracic paravertebral area, paravertebral muscles and the hyper-echoic transverse process were identified clearly. The black acoustic shadow in front of the transverse process completely obscured the thoracic paravertebral area. The hyper-echoic area among parietal pleura, superior costotransverse ligament (SCL) and internal intercostal membrane which represents the top of thoracic paravertebral space (TPVS) or the medial boundary of posterior intercostal space was correspondingly identified by slightly moving the transducer cranially or caudally. Subsequently, colour Doppler mode was used to identify whether a vulnerable blood vessel was abnormally situated around the targeted TPVB area in order to avoid intravascular injection. A 22-gague needle with echogenic (Benlan, Oakville, Canada) was introduced under real-time US-guided from lateral to medial section with an in-plane technique to target the hyper-echoic TPVS top or the posterior intercostal space. After confirmation of the needle tip, 2 ml of 1% lidocaine was injected for test. Each patient was monitored for five minutes for the clinical signs of anaesthesia/HZ associated pain alleviation in the affected thoracic dermatomal. After verification, 5 ml of block liquid mixture was slowly injected to the TPVS for each involved nerve root under the real-time US guidance. Meanwhile, the hyper-echoic pleura were moved forward and the top of TPVS was expanded due to the spread of the injectable suspension in the real-time ultrasonic image (). Each affected nerve root by HZ was identified to be accessed and blocked using the above TSA method under US guidance.
Nonsteroidal anti-inflammatory drug celecoxib (200 mg tablets, up to two times daily, Celebrex, Pfizer Canada, Kirkland, Canada; Celecoxib, Apotex, Toronto, Canada) was given as an analgesic agent as a routine treatment if patients reported their worst pain from 1 to 3, oxycodone–acetaminophen (5 mg/325 mg tablets, up to four times daily, drug named Depalgos©; Molteni Farmaceutici, Inc., Tuscany, Italy) was available as rescue medication if the worst pain >3 measured by Zoster Brief Pain Inventory (ZBPI). Supplementing pain medicine including antidepressant drugs and antiepileptic drugs was prohibited. Moreover, no epidural or intrathecal nerve blocks were permitted during the whole follow-up period.
Follow-ups were performed throughout 180 days. Data were collected by a special trained investigator blinded to the patients’ group assignment at baseline (D0), on days 7 (D7), 14 (D14), 21 (D21), 30 (D30) at our pain clinic, and on days 90 (D90), 180 (D180) by telephone or email interviews.
Outcome measures
An 11-point scale from 0 (no pain) to 10 (pain as bad as you can imagine) which was derived from question 3 of the ZBPI was used to rate the “the worst pain in the last 24 h” associated to HZ [Citation11]. Burden of illness associated to HZ was evaluated as a function of pain duration. Quality of life (QoL) was assessed by the EuroQoL 5-Dimension Questionnaire (EQ-5D-3L) composed of the following five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. There were three levels in each dimension including no problems, some problems and extreme problems [Citation12]. PHN was defined as ZBPI “worst pain” score >3 for more than 90 days after HZ rash onset [Citation13–15]. The use and dosage of concomitant analgesics for each patient was also recorded. Safety was assessed by adverse events.
Power analysis
An estimate cohort of 45 patients was needed per group to be able to achieve 80% power with a two-tailed α of 5% in order to see a 25% decrease in the mean BOI-30AUC in TPVB group compared with control group. The mean BOI-30AUC of control group was 119.718 (SD = 50) in the pre-test consisting of 15 patients. Taking potential dropouts (10%) into consideration, 100 patients per group were included.
Statistical analysis
Statistical analyses were performed by SPSS software, version 19.0 (SPSS Inc., Chicago, IL). Statistical significance was set at the 5% level (two-tailed). Normal quantitative data were reported as mean ± standard deviation (SD) and categorical data as percentage. HZ-BOI scores were analysed by analysis of covariance (ANCOVA) model, using the baseline score as a covariate. Comparison of categorical data was conducted using the chi-square test and Fisher’s exact test. All analyses were according to the per protocol (PP) principle.
HZ-BOI scores were assessed by a severity-by-duration composite measure of pain which was expressed by the area under the curve (AUC) of pain severity over time. The curve of pain severity over time was referred to the dynamic change of ZBPI “worst pain”, taking time as the X-axis and pain severity on a 0–10 scale as the Y-axis. AUC was defined as the area bounded by the curve and coordinate axis, and calculated by GraphPad Prism version 5.0 (GraphPad Software Inc., San Diego, CA) by multiple segment trapezoidal rule. ZBPI and EQ-5D questionnaires were bound in a study booklet to ensure standardization of presentation among all patients. At the initial visit, patients were asked to complete the questionnaires to gather informed consent and eligibility for the study. All patients were provided with additional copies of the validated questionnaires which they were asked to complete at home once per week and return through email and at follow-up visits. Data collection and calculation were performed once at baseline, and further administered at each follow-up assessment date [Citation16].
Results
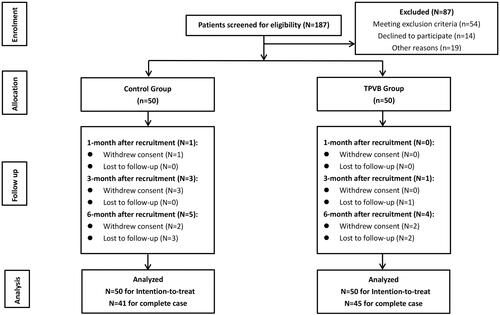
The flow diagram of the recruited patient progress is shown in . A total of 187 patients diagnosed with thoracic HZ were eligible for the study, but 87 patients were excluded because of different reasons. Fifty patients were randomly allocated to each group. In the follow-up period, nine patients from the control group and five patients from the TPVB group withdrew consent or failed to arrive for follow-up. Thus, at the 6-month mark after recruitment, a total of 41 patients were included in control group, and 45 patients in TPVB group for complete case (). No differences were shown on baseline demographic characteristics between two groups ().
Table 1. Baseline characteristics of participants in two groups.
shows that a significant decrease of HZ-BOI scores was revealed in TPVB group, compared to control group. The PP analysis shows that the mean of BOI-30AUC (acute HZ burden of illness (HZ-BOI) over 30 days) was 112.5 (95%CI: 105.2, 119.9) in control group, and 82.7 (95%CI: 75.4, 90.1) in TPVB group after adjusting baseline scores for covariate in the ANCOVA model. Significant difference was revealed between control group and TPVB group, 30 days post zoster rash onset (F = 32.252, p<.001), which indicated that patients in active group receiving TPVB under US-guidance experienced a significantly lower illness burden associated to HZ during the acute phase. The mean of BOI-30–90AUC was 102.3 (95%CI: 85.2, 119.4) in control group, 60.9 (95%CI: 43.9, 78.1) and in TPVB group with F = 11.392 and p=.001. The mean of BOI-90–180AUC was 91.1 (95%CI: 72.3, 109.9) in control group, 54.3 (95%CI: 35.6, 73.1) and in TPVB group with F = 7.467 and p=.007. Both of BOI-30–90AUC and BOI-90–180AUC showed that patients in active group had a lower BOI after receiving TPVB under the guidance of US with p value less than .001. The percentage of patients using rescue analgesics (celecoxib and oxycodone/acetaminophen) (71.9% vs. 45.1%, p<.001 at D30; 42.5% vs. 30.7%, p=.022 at D90; 34.6% vs. 24.2%, p=.030 at D180) decreased significantly in TPVB group, which demonstrated an adequate pain administration in TPVB group ().
Figure 3. Alteration in the consumption of rescue analgesics (celecoxib) in patients with inadequate pain relief in two groups during the follow-up period.
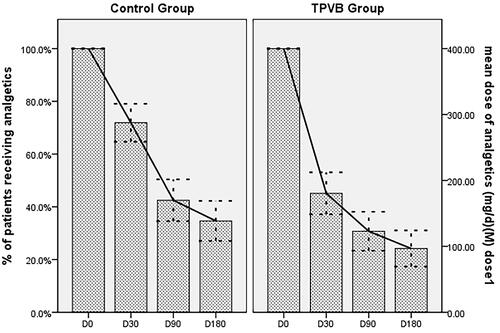
Table 2. HZ-BOI scores of two groups during study days 0–30, 30–90 and 90–180 according to PP analysis.
After 90 days, the incidence of PHN was 16/46 (34.8%) in control group, and 8/49 (16.3%) in TPVB group. Compared with control group, the RR = 2.733 (95%CI: 1.036, 7.215, p=.033) with an incidence difference of 18.5% (95%CI: 1.2%, 35.7%) in TPVB group. After 180 days, PHN incidence was 12/41 (29.3%) in control group, 5/45 (11.1%) in TPVB group (RR = 3.310, 95%CI: 1.051, 10.429, p=.032) with an incidence difference of 18.2% (95%CI: 1.5%, 34.8%) (). Therefore, there was significant difference in the PHN incidence between control group and active group after TPVB therapy using TSA approach.
Table 3. PHN incidence for control group versus TPVB group according to the PP analysis.
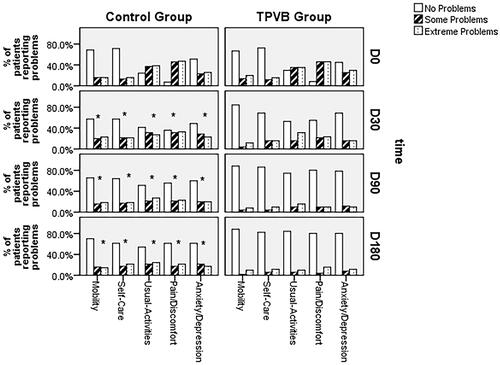
Compared with baseline QoL scores, patients in both groups exhibited a greater improvement of QoL after 30, 90 and 180 days. However, there was significant difference between control group and TPVB group in patients’ quality of life. According to EQ-5D-3L, there were differences in the proportion of patients who reported no discomfort, some degree of discomfort and extreme pain in terms of pain/discomfort (p=.003 at D30, p=.022 at D90, p=.009 at D180), usual activities (p=.016 at D30, p=.007 at D90, p=.028 at D180), mobility (p=.002 at D30, p=.009 at D90, p=.014 at D180), symptom of anxiety/depression (p=.034 at D30, p=.012 at D90, p=.021 at D180) and self-care (p=.048 at D30, p=.003 at D90, p<.001 at D180) between control group and TPVB group respectively at D30, D90 and D180 ().
Figure 4. The proportion of patients reporting problems in the EuroQoL EQ-5D domains at the time of day 0, 30, 90 and 180.
No serious adverse events were observed in the present study. Serious intravascular injection was not noted in TPVB group. Four patients (8.0%) experienced dizziness in TPVB group within 15 min after injection. Nine patients (18.0%) complained of pain at the entry point in TPVB group.
Discussion
In this prospective randomized comparative study, we assessed the effect of US-guided TPVB respectively using TSA approach for the treatment of thoracic HZ acute pain and its preventive effects on PHN. BOI-30AUC, BOI-30–90AUC and BOI-90–180AUC were 112.5, 102.3 and 91.1 in control group, 82.7, 60.9 and 54.3 in TPVB group, which showed that patients in TPVB group had a lower BOI after receiving TPVB injection under the guidance of US. The incidence of PHN was 34.8% in control group, 16.3% in TPVB group with RR = 2.733 at D90, and 29.3% in control group, 11.1% in TPVB group with RR = 3.310 at D180. This meant that PHN incidence in TPBV group was lower than that in control group during follow-up. The percentage of patients using analgesics decreased significantly in TPVB group when compared with the control group at D30, D90 and D180, which demonstrated better adequate pain administration in TPVB group. Compared with baseline QoL scores, patients in both groups exhibited a greater improvement of QoL after 30, 90 and 180 days. However, compared with control group, significant improvement of QoL was shown in TPVB group at all domains of QoL Questionnaire during the whole follow-up period.
The acute phase of HZ is characteristic by severe pain, and long-term pain has the potential for development of PHN [Citation17]. Currently, conventional therapy including antiviral agents and rescue analgesics can accelerate healing of the lesions and reduce the accompanying pain. However, antiviral agents have marginal success in preventing and treating PHN, and analgesics only provide effective temporary pain relief for HZ and PHN, especially for those situations of refractory pain or other relevant risk factors for PHN [Citation5,Citation18]. Recent review and meta-analysis reported that stellate ganglion block, intercostal nerve block, paravertebral block, selective nerve root block and epidural block that administered early in the course of HZ as an interventional and supplemental pain management could offer more long-term pain relief in both acute HZ and PHN [Citation19,Citation20].
Ji et al. reported a randomized controlled trial (RCT) study to assess the effectiveness of repetitive paravertebral injections with local anaesthetics and steroids for the prevention of PHN in 132 patients with acute HZ. At 1 month after four repetitive paravertebral injections, compared with 45% patients in the standard group (oral antivirals and analgesics), 13% in the paravertebral group reported pain related to zoster (p<.001). At 3 and 6 month post-therapy, the incidence of PHN was significantly lower in the paravertebral group than in the standard group (7% vs. 30%, p=.001 at 3 months; 4% vs. 22%, p=.003 at 6 months). They concluded that repetitive paravertebral anaesthetic block combined with steroids plus standard treatment significantly reduced the incidence of PHN than the standard treatment (antiviral medications and analgesics) alone [Citation8]. Consistent with previous results, our study also reported significant reduction of HZ-related illness burden (pain severity over time) after four repetitive TPVBs in TPVB group. The incidence of PHN was 34.8% and 29.3% in control group after 90 days and 180 days, respectively. We speculated that conducting paravertebral block with local anaesthetics and steroids during the early-onset of HZ could reduce root oedema by inhibiting the inflammation of the affected nerves. In turn, this would reduce pain severity, facilitate nerve healing and suppressed developing PHN. Furthermore, viral inflammation of dorsal root ganglion caused by HZ stimulated the sympathetic nervous system inducing neuronal ischaemia and death of the large myelinated nerve fibres. Treatment of HZ with sympathetic block in an early stage might inhibit the irreversible damage to the nerve [Citation21]. Meanwhile, there was sympathetic chain locating on each side of the paravertebral gutter [Citation8]. Thus, high-volume paravertebral injection of liquid drug could expand to block the affected sympathetic chain to stop the irreversible damage. An RCT study found that high-volume injection of local anaesthetics could dilute inflammatory cytokines, remove adhesions, improve blood circulation, inhibit ectopic discharge of affected nerves and reduce central sensitization [Citation22]. Compared with epidural block through transforaminal (TF) or interlaminar (IL) approach, paravertebral block allowed greater amount of local anaesthetic injection, which could lessen HZ related pain. We injected a total of 5 ml liquid mixture of local anaesthetic and steroids to the paravertebral space according to the width of the dermatome affected by HZ. Although the number of transactions was different for each patient in the present study, we thought enough high-volume was guaranteed for each affected nerve to obtain adequate pain relief and reduce the ZBPI pain score. As expected, HZ related BOI-30AUC, BOI-30–90AUC and BOI-90–180AUC were lower in TPVB group, which meant better pain relief was obtained after receiving high-volume paravertebral block under US-guidance.
The effect of a single epidural injection of local anaesthetic and steroid in the acute phase of HZ for 598 patients was conducted in the RCT study. The results showed that at 1 month, 48% patients in the epidural group reported pain compared with 58%in the control group (RR = 0.83, 95%CI: 0.71–0.97, p=.02). After 3 months, these values were 21% and 24% respectively (0.89, 0.65–1.21, p=.47) and, at 6 months, 15% and 17%; (0.85, 0.57–1.13, p=.43). They concluded that a single epidural injection has a modest effect in reducing ZAP in 1 month. Nevertheless, this treatment is not effective for prevention of long-term postherpetic neuralgia [Citation23]. A recent meta-analysis results showed that continuous or repeated epidural blocks could significantly reduce PHN incidence (11% in epidural group vs. 36% in the control group; p=.05). PHN incidence in the groups treated with repetitive nerve blocks was 0–26.7% at 3 months, 5.5–13.9% at 6 months, and 2–5.9% at 12 months [Citation23–25]. In addition, there were rare but serious risks carried by epidural injection under fluoroscopy using IL or TF approach such as epidural haematoma, spinal cord injury, nerve injury and intravascular injection [Citation26]. Therefore, our results also demonstrated that the early suppressive and preventive effect might be more potent if we conducted repetitive paravertebral block under US guidance. Compared with fluoroscopy, US-guided TPVB could avoid exposing the pain physician and patients to radiation, at the same time, the needle could be advanced to get the predetermined targeted and the drug could be continuously injected under real-time imaging. Vessels within 2 mm distance from the targeted area could be identified by Doppler US scan, thus the direction of needle puncture would be adjusted to avoid penetrating the critical vessels to avert from intravascular injection [Citation27,Citation28]. We had to admit that this technique highly depends on experience of the operator. Perforation of pleura inducing pneumothorax was one of the most serious complications of TPVB technique; however, no serious advents were observed in the study. This would be benefitted from the use of US real-time guidance and measurement of pleura depth from entry point before puncture.
In accordance with what was expected, the percentage of patients using rescue analgesics decreased significantly in TPVB group when compared with the control group, which demonstrated better adequate pain administration after TPVB therapy. Moreover, our results showed that compared with baseline QoL scores, patients in both groups exhibited a greater improvement of QoL after 30, 90 and 180 days. However, there were significant differences between control group and TPVB group. Greater improvement of QoL was observed in TPVB group at all domains of EuroQoL EQ-5D Questionnaire during the whole follow-up period. Consistent with our results, several previous studies indicated that health-related quality of life (QoL) was significantly impaired by both severe acute HZ associated pain and PHN-associated pain [Citation29,Citation30].
The study did have some limitations. First, there is no placebo group in which the patients underwent the injections with normal saline under the guidance of US. Second, the long-time efficacy of TPBV therapy for the treatment of acute pain associated to HZ was absent in the present study, which might be more meaningful for the assessment of efficacy. Third, patients in this study were allowed to use rescue analgesics, which would be a confounding factor in the analysis of the efficacy and safety of TPVB therapy under US guidance. Fourth, the cephalo-caudal spread and the occurrence of epidural spread in the TPVB group using TSA approach under the guidance of US were not observed in the present study due to lack of verification of liquid drug spread after thoracic paravertebral injection with contrast agent under CT or C-arm guidance. Therefore, the influence of this spread on the incidence of PHN was not demonstrated in this study. We expected to perform a prospective comparative study under CT guidance to investigate this influence of the incidence of PHN.
Conclusions
Our results indicated that a clinical meaningful reduction was shown in the BOI associated to HZ, and a satisfactory improvement was shown in patients’ quality of life in TPVB group after US-guided TPVB therapy using TSA approach. Therefore, we concluded that besides antiviral therapy, additional TPVB under the US guidance represented an early intervention during acute phase of HZ, which could effectively reduce the illness burden associated to HZ, and might be a feasible preventive strategy to reduce the incidence of PHN.
Authors contributions
Li Niu was involved in the conception and design, analysis and interpretation of the data; the drafting of the paper, revising it critically for intellectual content; and the final approval of the version to be published. Yingchao Ma was involved in the conception and design, analysis and interpretation of the data; the drafting of the paper, revising it critically for intellectual content. Lei Sun was involved in the conception and design, analysis and interpretation of the data; the drafting of the paper. Xin He was involved in the conception and design, analysis and interpretation of the data. Shuang Wu was involved in the conception and design, analysis and interpretation of the data. Fan Shi was involved in the conception and design, analysis and interpretation of the data. All authors agreed to be accountable for all aspects of the work.
| Abbreviations | ||
| TPVB | = | thoracic paravertebral block |
| PHN | = | post-herpetic neuralgia |
| HZ | = | herpes zoster |
| BOI | = | burden of illness |
| 30AUC | = | area under the curve of pain severity over 30 days |
| QoL | = | quality of life |
| VZV | = | varicella zoster viruses |
| DRG | = | dorsal root ganglion |
| ZAP | = | zoster-associated pain |
| ZBPI | = | Zoster Brief Pain Inventory |
| AUC | = | area under the curve |
| LA | = | local anaesthetics |
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, Professor Li Niu, upon reasonable request.
References
- Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6):e004833.
- Ljubojevic HS, Kovacevic M, Skerlev M, et al. Genital herpes zoster as possible indicator of HIV infection. Acta Dermatovenerol Croat. 2018;26(4):337–338.
- Patki A, Vora A, Parikh R, et al. Herpes zoster in outpatient departments of healthcare centers in India: a review of literature. Hum Vaccin Immunother. 2021;17:1–8.
- Gater A, Abetz-Webb L, Carroll S, et al. Burden of herpes zoster in the UK: findings from the zoster quality of life (ZQOL) study. BMC Infect Dis. 2014;14(1):402.
- Forbes HJ, Thomas SL, Smeeth L, et al. A systematic review and meta-analysis of risk factors for postherpetic neuralgia. Pain. 2016;157(1):30–54.
- Makharita MY. Prevention of post-herpetic neuralgia from dream to reality: a ten-step model. Pain Physician. 2017;20(2):E209–E220.
- Makharita MY, Amr YM, El-Bayoumy Y. Single paravertebral injection for acute thoracic herpes zoster: a randomized controlled trial. Pain Pract. 2015;15(3):229–235.
- Ji G, Niu J, Shi Y, et al. The effectiveness of repetitive paravertebral injections with local anesthetics and steroids for the prevention of postherpetic neuralgia in patients with acute herpes zoster. Anesth Analg. 2009;109(5):1651–1655.
- Lee HJ, Park HS, Moon HI, et al. Effect of ultrasound-guided intercostal nerve block versus fluoroscopy-guided epidural nerve block in patients with thoracic herpes zoster: a comparative study. J Ultrasound Med. 2019;38:725–731.
- Chen N, Li Q, Yang J, et al. Antiviral treatment for preventing postherpetic neuralgia. Cochrane Database Syst Rev. 2014;CD006866.
- Coplan PM, Schmader K, Nikas A, et al. Development of a measure of the burden of pain due to herpes zoster and postherpetic neuralgia for prevention trials: adaptation of the brief pain inventory. J Pain. 2004;5(6):344–356.
- Selivanova A, Buskens E, Krabbe P. Head-to-head comparison of EQ-5D-3L and EQ-5D-5L health values. Pharmacoeconomics. 2018;36(6):715–725.
- Song H, Lee J, Lee M, et al. Burden of illness, quality of life, and healthcare utilization among patients with herpes zoster in South Korea: a prospective clinical-epidemiological study. Int J Infect Dis. 2014;20:23–30.
- Poquet N, Lin C. The Brief Pain Inventory (BPI). J Physiother. 2016;62(1):52.
- Alicino C, Trucchi C, Paganino C, et al. Incidence of herpes zoster and post-herpetic neuralgia in Italy: results from a 3-years population-based study. Hum Vaccin Immunother. 2017;13(2):399–404.
- Zheng S, Li X, Yang X, et al. Ultrasound-guided cervical nerve root block for the treatment of acute cervical herpes zoster: a randomized controlled clinical study. Pain Pract. 2019;19(5):500–509.
- Johnson RW, Alvarez-Pasquin MJ, Bijl M, et al. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective. Ther Adv Vaccines. 2015;3(4):109–120.
- Roxas M. Herpes zoster and postherpetic neuralgia: diagnosis and therapeutic considerations. Altern Med Rev. 2006;11(2):102–113.
- Shannon HJ, Anderson J, Damle JS. Evidence for interventional procedures as an adjunct therapy in the treatment of shingles pain. Adv Skin Wound Care. 2012;25(6):276–284; quiz 285–286.
- Xing XF, Zhou ZF, Zhang FJ, et al. The effect of early use of supplemental therapy on preventing postherpetic neuralgia: a systematic review and meta-analysis. Pain Physician. 2017;20(6):471–486.
- Winnie AP, Hartwell PW. Relationship between time of treatment of acute herpes zoster with sympathetic blockade and prevention of post-herpetic neuralgia: clinical support for a new theory of the mechanism by which sympathetic blockade provides therapeutic benefit. Reg Anesth. 1993;18(5):277–282.
- Chun EH, Park HS. Effect of high-volume injectate in lumbar transforaminal epidural steroid injections: a randomized, active control trial. Pain Physician. 2015;18:519–525.
- van Wijck AJ, Opstelten W, Moons KG, et al. The PINE study of epidural steroids and local anaesthetics to prevent postherpetic neuralgia: a randomised controlled trial. Lancet. 2006;367(9506):219–224.
- Kim HJ, Ahn HS, Lee JY, et al. Effects of applying nerve blocks to prevent postherpetic neuralgia in patients with acute herpes zoster: a systematic review and meta-analysis. Korean J Pain. 2017;30(1):3–17.
- Pasqualucci A, Pasqualucci V, Galla F, et al. Prevention of post-herpetic neuralgia: acyclovir and prednisolone versus epidural local anesthetic and methylprednisolone. Acta Anaesthesiol Scand. 2000;44(8):910–918.
- Fujiwara A, Watanabe K, Hashizume K, et al. Transforaminal vs interlaminar epidural steroid injection for acute-phase shingles: a randomized, prospective trial. Pain Physician. 2018;21(4):373–382.
- Lee HH, Park D, Oh Y, et al. Ultrasonography evaluation of vulnerable vessels around cervical nerve roots during selective cervical nerve root block. Ann Rehabil Med. 2017;41(1):66–71.
- Huntoon MA. Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005;117(1–2):104–111.
- Mizukami A, Sato K, Adachi K, et al. Impact of herpes zoster and post-herpetic neuralgia on health-related quality of life in Japanese adults aged 60 years or older: results from a prospective, observational cohort study. Clin Drug Investig. 2018;38(1):29–37.
- Torcel-Pagnon L, Bricout H, Bertrand I, et al. Impact of underlying conditions on zoster-related pain and on quality of life following zoster. J Gerontol A Biol Sci Med Sci. 2017;72(8):1091–1097.