Abstract
Background: Vertebral compression fractures (VCFs) often occur in patients with osteoporosis. These fractures can also lead to postural changes. Several studies have shown that patients with vertebral compression fractures have a restrictive pattern in their pulmonary function. Percutaneous vertebroplasty (PVP) is the standard treatment for vertebral compression fractures, with the benefits of pain relief and enhancement of vertebral stability for partially collapsed vertebral bodies. However, the effects of PVP on short-term recovery of respiratory performance have not been investigated. Therefore, this study aimed to investigate the changes in pulmonary function, respiratory muscle strength, maximal voluntary ventilation (MVV), and chest mobility in patients with vertebral compression fractures after PVP.
Methods: This research was approved by the clinic committee of the E-DA Hospital Institutional Review Board (EMRP07109N) and registered in the Thai Clinical Trials Registry (TCTR20211029005). We recruited 32 VCF patients. Four-time points were measured: before and after PVP and 1 and 3 weeks after PVP. We measured pulmonary function and maximum voluntary ventilation (MVV) by using spirometry. Respiratory muscle strength was assessed by using a respiratory pressure meter. The chest expansion test was used to evaluate chest mobility. A visual analogue scale (VAS) was used to assess resting and aggravated back pain.
Results: Chest expansion and back pain improved at each time point after PVP. MVV showed significant progress at both 1 and 3 weeks after discharge. Forced expiratory volume in 1 second (FEV1) and maximal inspiratory muscle strength significantly improved 1 week after discharge.
Conclusion: Taking all the data together, PVP not only can resolve severe back pain but can also provide excellent improvements in MVV and chest mobility in patients with vertebral compression fractures.
1. Introduction
The World Health Organisation (WHO) defines osteoporosis as a systemic bone disease. Its characteristics include decreased bone mass and deterioration of the microstructure of bone tissue, resulting in weak bones and an increased risk of fracture [Citation1]. Vertebral compression fracture (VCF) is diagnosed by a reduction of more than 20% or 4 mm of the individual vertebral height [Citation2]. There are many causes of VCF, such as traumatic history, cancer, or osteoporosis. It is well established that VCF causes intensive pain in the back and impairment of physical function, which affects the patient’s quality of life and psychosocial status [Citation3,Citation4]. Osteoporotic VCF affects a calculated 1.4 million individuals around the world every year [Citation5].
Aside from severe pain in the back, patients with VCF also tend to have abnormal posture and excessive kyphosis [Citation6]. Numerous reports have revealed that a restrictive pattern in pulmonary function is positively correlated with the severity of vertebral fracture and the extent of kyphosis [Citation7,Citation8]. Patients with osteoporosis-related kyphosis were shown to have significantly decreased vital capacity (VC), lateral rib expansion, and forced expiratory volume in one second (FEV1). A negative correlation between predicted VC and the degree of kyphosis has also been reported [Citation8,Citation9]. Painful osteoporotic VCF is difficult to cure with medical treatment. Percutaneous vertebroplasty (PVP) was initially described by Deramond’s group in 1987 for the treatment of an aggressive vertebral haemangioma [Citation10]. To date, PVP has become a popular intervention for the management of VCF patients. PVP is an image-guided procedure in which radiopaque bone cement is injected into the collapsed vertebral body, providing stability to the vertebral body and relieving back pain [Citation11].
Previous studies confirmed that vertebral compression fracture can cause a restrictive pulmonary function pattern and negatively influence respiratory-related parameters. Percutaneous vertebroplasty is the standard intervention used to resolve severe back pain. However, to date, no studies have explored the progress in respiratory performance after percutaneous vertebroplasty. Based on previous reports, in this study we aimed to investigate the changes in pulmonary function, respiratory muscle strength, and chest mobility after percutaneous vertebroplasty in patients with vertebral compression fracture.
2. Materials and methods
2.1. Study participants
Patients with osteoporotic vertebral compression fractures were recruited from the outpatient clinic of the orthopaedic department of E-DA Hospital, Kaohsiung, Taiwan. Patients were eligible for inclusion if they were 45–90 years of age, diagnosed with osteoporotic vertebral compression fracture, and planning to receive percutaneous vertebroplasty. Patients who had concurrent malignancy or acute infectious disease, a history of thoracic or lumbar fusion surgery, a diagnosis of pulmonary disease (e.g. lung cancer, asthma, chronic obstructive pulmonary disease, or pneumothorax), or limited range of motion in shoulder active flexion and abduction (less than 120°) were excluded from this study. This research was approved by the clinic committee of the E-DA Hospital Institutional Review Board (EDAH IRB: EMRP07109N) and registered in the Thai Clinical Trials Registry (TCTR) (TCTR20211029005). This clinical trial recruited participants from 07 May 2020 to 06 May 2021. All participants provided informed consent and underwent baseline assessment measurements.
2.2. Study protocol
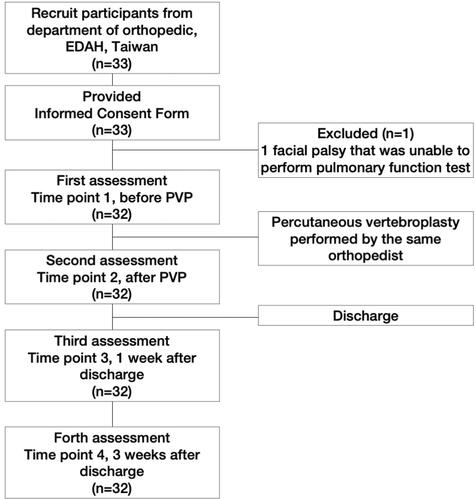
The present study enrolled 32 participants, 5 men and 27 women. There were four study time points for testing: (1) before the operation; (2) after the operation; (3) one week after discharge; and (4) 3 weeks after discharge. All assessments were conducted by the same physical therapist. The participants received conventional treatment during hospitalisation and were discharged for follow-up at the orthopaedic outpatient department as part of the general care protocol. The content of this study protocol is shown in .
2.3. Pulmonary function test and maximal voluntary ventilation
Spirometry (microQuark, COSMED, Italy) was used to measure pulmonary function and maximal voluntary ventilation. The values of forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), and peak expiratory flow rate (PEFR) were used to indicate lung capacity, airway resistance, and gas exchange efficiency. Maximal voluntary ventilation (MVV) was collected by monitoring the maximal volume and effort of ventilation during an interval of 12 s. Each measurement was performed three times and averaged at each study time point to assure the measurement was reproducible and accurate.
2.4. Respiratory muscle strength
A GB60 pressure gauge (JITTO, Taiwan) connected to a one-way valve and a mouthpiece was used to measure respiratory muscle strength. To measure maximal inspiratory pressure (MIP, PImax), the patient was instructed to exhale completely and then inhale forcefully. Maximal expiratory pressure (MEP, PEmax) was measured during forced expiration after a full inhalation. The largest negative pressure of inhalation and positive pressure of exhalation were record. Each measurement was performed three times and averaged at each study time point to assure the measurement was reproducible and accurate.
2.5. Chest mobility
The chest expansion test was selected to test the mobility of the rib cage [Citation12,Citation13]. While in a seated position, the patient was asked to breathe in gradually through the nose, using lung expansion to push the measuring tape as much as possible, then to breathe out through the mouth as completely as possible. The therapist measured the difference in chest circumference between the end of a complete inspiration and expiration cycle with a cloth tape. The anatomical mark was the xiphoid process, and the tenth thoracic spinous process was determined as the posterior landmark [Citation14]. The chest mobility test was performed three times and averaged at each study time point to assure the measurement was reproducible and accurate. This method was proven to be reliable with ICCs of 0.81–0.91 (95% confidence interval, 0.69–0.99) [Citation15].
2.5. Back pain scale
Pain intensity was evaluated by the visual analogue scale (VAS). Operationally, the VAS was a horizontal line 100 mm in length anchored by descriptors at each end: “No pain” and “Very severe pain”. The patient was instructed to mark the point on the line indicating their perception of pain in the resting state (resting pain) and in the worst state in which pain was aggravated by daily activity (aggravated pain). The VAS score was determined by measuring, in millimetres, from the left side of the line to the point the patient marked [Citation16].
2.7. Statistical analysis
The results are presented as mean and standard deviation. Because of the small sample size, Wilcoxon signed-rank test was used to analyse differences among time points. The significance level was considered as p < .05. All statistical analyses were performed by SPSS software version 22.0 (SPSS, Chicago, IL).
3. Results
3.1. Demographic data and clinical characteristics of subjects
In this study, 33 patients with osteoporotic compression fractures who met the inclusion criteria were referred from the orthopaedic outpatient department and signed informed consent. However, 1 patient was excluded because of difficulty using the mouthpiece due to facial palsy. Thus, there were 32 participants in total, 5 men and 27 women. The average age was 75.7 ± 8.6 years (75.4 ± 5.6 years for men, 75.8 ± 9.1 years for women), average height was 150.8 ± 8.1 cm (158.7 ± 3.3 cm for men, 148.9 ± 7.7 cm for women), and average weight was 55.2 ± 12.1 kg (66.9 ± 18.2 kg for men, 53.1 ± 9.7 kg for women). The average admission was 2.1 ± 0.7 days (1.8 ± 0.4 days for men, 2.2 ± 0.8 days for women) ().
Table 1. Baseline characteristics of the VCF patients.
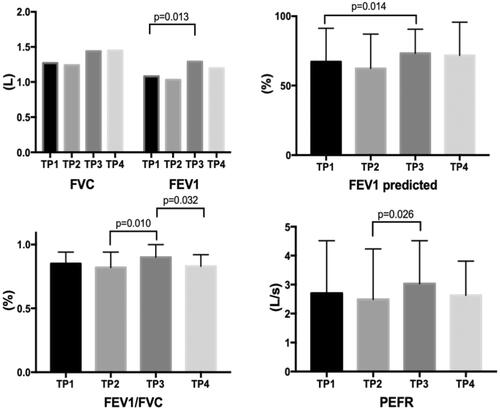
3.2. Effects on pulmonary function in osteoporotic compression fractures with PVP
shows that the performance of forced vital capacity (FVC) was not significantly different between any time points. The parameters FEV1 and FEV1 predicted showed a statistical difference between before operation and 1 week after discharge (time point 1 vs. time point 3). FEV1/FVC showed statistically significant differences between 1 week after discharge and post operation and 3 weeks after discharge (time point 3 vs. time points 2 and 4). Peak expiratory flow rate (PEFR) showed a significant difference between post-operation and one week after discharge (time point 2 vs. time point 3).
Figure 2. Pulmonary function test of each period. Data was presented as mean and standard deviation. Wilcoxon signed-rank test was used to analyse differences among time points. TP1: time point 1, before the operation; TP2: time point 2, after the operation; TP3: time point 3, 1 week after discharge; TP4: time point 4, 3 weeks after discharge; FVC: forced vital capacity; FEV1: forced expiratory volume in one second; PEFR: peak expiratory flow rate.
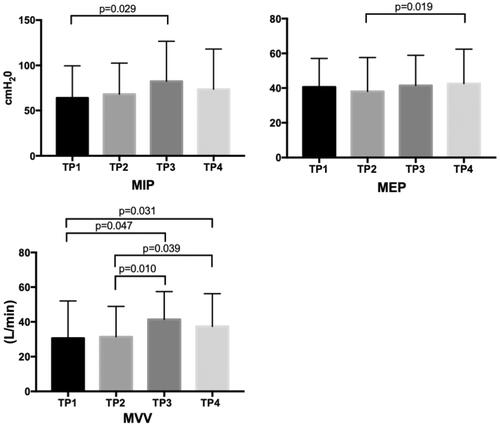
3.3. Effects on respiratory muscle strength and maximal voluntary ventilation in osteoporotic compression fractures with PVP
For respiratory muscle strength, we found no statistical difference in maximal inspiratory pressure (MIP) after PVP. However, there was a statistically significant difference between before PVP and 1 week after discharge (time point 1 vs. time point 3). Maximal expiratory pressure (MEP) showed a statistical difference between post-PVP and 3 weeks after discharge (time point 2 vs. time point 4) (). Moreover, we found no statistically significant difference in maximal voluntary ventilation (MVV) before and after surgery. However, there were statistically significant differences between before PVP and 1 and 3 weeks after discharge (time point 1 vs. time points 3 and 4). There were also statistically significant differences between post-PVP and 1 and 3 weeks after discharge (time point 2 vs. time points 3 and 4). However, there was no significant difference between 1 and 3 weeks after discharge (time point 3 vs. time point 4), as shown in .
Figure 3. Respiratory muscles strength and Maximal voluntary ventilation of each period. Data was presented as mean and standard deviation. Wilcoxon signed-rank test was used to analyse differences among time points. TP1: time point 1, before the operation; TP2: time point 2, after the operation; TP3: time point 3, 1 week after discharge; TP4: time point 4, 3 weeks after discharge; MIP: maximal inspiratory pressure; MEP: maximal expiratory pressure; MVV: maximal voluntary ventilation.
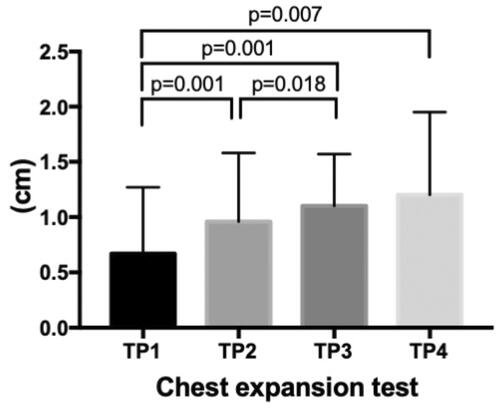
3.4. Effects on chest expansion in osteoporotic compression fractures with PVP
Improved chest wall expansion was immediately apparent after PVP (time point 1 vs. time point 2). Statistical differences were found when comparing PVP 1 and 3 weeks after discharge (time point 1 vs. time points 3 and 4). There was also a significant improvement between after PVP and 1 week after discharge (time point 2 vs. time point 3) ().
Figure 4. Chest mobility of each period. Data was presented as mean and standard deviation. Wilcoxon signed-rank test was used to analyse differences among time points. TP1: time point 1, before the operation; TP2: time point 2, after the operation; TP3: time point 3, 1 week after discharge; TP4: time point 4, 3 weeks after discharge.
3.5. Effects on back pain scale in osteoporotic compression fractures with PVP
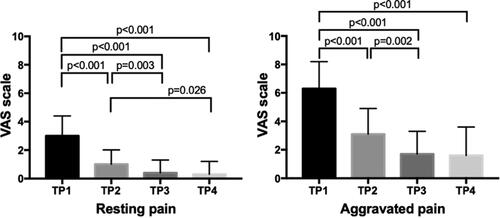
Resting pain showed significant improvement after PVP (time point 1 vs. time point 2), before PVP and 1 week after discharge (time point 1 vs. time point 3), before PVP and 3 weeks after discharge (time point 1 vs. time point 4), and post-PVP and 1 week after discharge (time point 2 vs. time point 3). The tendency of improved aggravated pain was similar to the results of resting pain ().
Figure 5. Back pain state of each period. Data was presented as mean and standard deviation. Wilcoxon signed-rank test was used to analyse differences among time points. TP1: time point 1, before the operation; TP2: time point 2, after the operation; TP3: time point 3, 1 week after discharge; TP4: time point 4, 3 weeks after discharge; VAS: visual analogue scale.
4. Discussion
Vertebral compression fractures are known to occur in the elderly. Transcutaneous vertebroplasty is the most common treatment for vertebral compression fractures. According to the standard procedure, transcutaneous vertebroplasty is performed by injecting radiopaque bone cement into the partially collapsed vertebral body to achieve pain relief, increase spine stability, and even restore the vertebral body height [Citation11]. Over the past few decades, several studies have explored the clinical benefits of transcutaneous vertebroplasty in terms of pain and quality of life, as well as its adverse events [Citation17]. In this study, we investigated the effect of percutaneous vertebroplasty (PVP) on pulmonary function, respiratory muscle strength, chest mobility, and back pain status in patients with vertebral compression fracture (VCF).
Several studies have confirmed that patients with VCF have diminished respiratory performance [Citation18,Citation19]. We found that our study participants only showed short-term improvement in FEV1 in the pulmonary function test after PVP. Abnormal trunk posture can lead to lung compression, reduced rib mobility, and restricted breathing capacity [Citation20]. Our experiment did not include posture training, and the pulmonary function test results were not as expected. On the other hand, a previous study reported that VCF in patients with rib fractures improved continuously over 1 year after open reduction and internal fixation [Citation21]. To achieve the desired pulmonary function, we suggest adding respiratory training and an aerobic exercise program to the treatment plan for patients with VCF after PVP in clinical practice.
Respiratory muscle strength involves inspiratory and expiratory muscle action. To date, there has been no study investigating respiratory muscle strength in VCF patients. According to our experimental results, MEP data showed significant improvement between post-operation and 3 weeks after discharge (time point 2 vs. time point 4). This positive progress may be related to patients returning to their past physical activity due to relief of their aggravated back pain. Maximal voluntary ventilation (MVV) is the maximal air volume an individual can breathe over 12 s [Citation22]. This parameter provides information on respiratory muscle mechanics and endurance, which are involved in the mechanism of dyspnoea and exercise limitation [Citation23]. MVV is also closely correlated with the Cobb angle, which is the most widely used measurement to quantify the magnitude of spinal deformities. It was reported that this is a more practical and sensitive test than FVC for assessing adolescent patients with idiopathic scoliosis [Citation12]. In this study, MVV showed remarkable short-term and long-term improvements. It was found that MVV increased post-operation and 1 week after discharge (time points 2 and 3). It can be predicted that PVP promotes respiratory muscle mechanics and increases exercise capacity in VCF patients.
Several studies observed a relationship between chest wall mobility, sex, age, pulmonary function, and respiratory muscle strength [Citation14,Citation16,Citation24]. Our experiment showed that PVP provides immediate, short-term, and long-term improvements in chest wall expansion. In addition, effective pain management can prevent pulmonary complications such as atelectasis and pneumonia [Citation25]. PVP also provided immediate, short-term, and long-term effects in terms of pain reduction; both resting pain and aggravated pain were mitigated after PVP. A previous study reported that patients with vertebral compression fractures who underwent PVP had a decreased pain scale by 3.5 ± 2.6 points on the third day, 4.2 ± 2.7 points in the second week, 4.6 ± 3.0 points in the first month, 5.4 ± 3.5 points in the third month, and 6.1 ± 3.3 points in the sixth month after the operation [Citation26]. Our results showed a similar tendency to those with regard to aggravated back pain.
This article was the first research to investigate pulmonary function, chest mobility and pain in VCF patients after percutaneous vertebroplasty. Based on ethical considerations, our study was an open-label single-arm study that explored change through time of intervention. There were some limitations in the present study. First, the research was conducted in a single centre. Second, Percutaneous vertebroplasty was performed by the same orthopaedic physician. Further studies that included more physicians and multicenter trials were needed to support the external validity and generalised the results across situations. Third, insufficient sample size and skewed gender demographic in our study may affect the reliability of the results. Large scale randomized-control trials would be suggested to reduce sample bias in future research.
5. Conclusion
Taking all the data together, PVP for patients with VCF was found to not only resolve severe back pain, but also provide excellent improvements in MVV and chest mobility. The effects on pulmonary function and respiratory muscle strength were limited. Thus, further studies should combine respiratory exercise training and respiratory muscle training to optimise the impact of PVP.
Ethics approval
This research was approved by the clinic committee of the E-DA Hospital Institutional Review Board (EDAH IRB: EMRP07109N) and registered in the Thai Clinical Trials Registry (TCTR) (TCTR20211029005).
Author contributions
Conception and design: Ching-Hou Ma, Zhi-Xiang Wu, and Yu-Ting Huang; data curation: Ching-Hou Ma, Zhi-Xiang Wu, and Hsin-Lun Yang; formal analysis: Hui-Ching Cheng and Wan-Ching Chou; investigation: Hui-Ching Cheng, Wan-Ching Chou, Ching-Hsia Hung and Kun-Ling Tsai; writing – original draft: Ching-Hou Ma and Kun-Ling Tsai; writing – review and editing: Ching-Hou Ma, Hsin-Lun Yang, Yu-Ting Huang and Kun-Ling Tsai. All authors agree to be accountable for all aspects of the work.
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data availability statement
The data presented in this study are available in the article.
Additional information
Funding
References
- Sozen T, Ozisik L, Basaran NC. An overview and management of osteoporosis. Eur J Rheumatol. 2017;4(1):46–56.
- Black DM, Palermo L, Nevitt MC, et al. Defining incident vertebral deformity: a prospective comparison of several approaches. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14(1):90–101.
- Phillips FM, Pfeifer BA, Lieberman IH, et al. Minimally invasive treatments of osteoporotic vertebral compression fractures: vertebroplasty and kyphoplasty. Instr Course Lect. 2003;52:559–567.
- Stallmeyer MJ, Zoarski GH, Obuchowski AM. Optimizing patient selection in percutaneous vertebroplasty. J Vasc Interv Radiol. 2003;14(6):683–696.
- Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–1733.
- Leech JA, Dulberg C, Kellie S, et al. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 1990;141(1):68–71.
- Culham EG, Jimenez HA, King CE. Thoracic kyphosis, rib mobility, and lung volumes in normal women and women with osteoporosis. Spine (Phila Pa 1976). 1994;19(11):1250–1255.
- Schlaich C, Minne HW, Bruckner T, et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int. 1998;8(3):261–267.
- Lombardi I Jr, Oliveira LM, Mayer AF, et al. Evaluation of pulmonary function and quality of life in women with osteoporosis. Osteoporos Int. 2005;16(10):1247–1253.
- Galibert P, Deramond H, Rosat P, et al. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie. 1987;33(2):166–168.
- Tsoumakidou G, Too CW, Koch G, et al. CIRSE guidelines on percutaneous vertebral augmentation. Cardiovasc Intervent Radiol. 2017;40(3):331–342.
- Villamor GA, Andras LM, Redding G, et al. A comparison of maximal voluntary ventilation and forced vital capacity in adolescent idiopathic scoliosis patients. Spine Deform. 2019;7(5):729–733.
- Mohammad Rahimi N, Mahdavinejad R, Attarzadeh Hosseini SR, et al. Efficacy of dynamic neuromuscular stabilization breathing exercises on chest mobility, trunk muscles, and thoracic kyphosis: a randomized controlled 6-Week trial. IRJ. 2020;18(3):329–336.
- Adachi D, Yamada M, Nishiguchi S, et al. Age-related decline in chest wall mobility: a cross-sectional study among community-dwelling elderly women. J Am Osteopath Assoc. 2015;115(6):384–389.
- Bockenhauer SE, Chen H, Julliard KN, et al. Measuring thoracic excursion: reliability of the cloth tape measure technique. J Am Osteopath Assoc. 2007;107(5):191–196.
- Şahin G, Ulubaş B, Çalikoğlu M, et al. Is chest expansion a determinant of pulmonary muscle strength in primary fibromyalgia? Joint Bone Spine. 2004;71(2):140–143.
- Buchbinder R, Johnston RV, Rischin KJ, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2018;4(4):Cd006349.
- Gil Obando LM, López López A, Avila CL. Normal values of the maximal respiratory pressures in healthy people older than 20 years old in the City of Manizales - Colombia. Colomb Med (Cali). 2012;43(2):119–125.
- Debouche S, Pitance L, Robert A, et al. Reliability and reproducibility of chest wall expansion measurement in young healthy adults. J Manipulative Physiol Ther. 2016;39(6):443–449.
- Roberts SB, Tsirikos AI. Factors influencing the evaluation and management of neuromuscular scoliosis: a review of the literature. J Back Musculoskelet Rehabil. 2016;29(4):613–623.
- Tanaka H, Yukioka T, Yamaguti Y. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52(4):727–732. discussion 32.
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338.
- Polkey MI, Kyroussis D, Hamnegard CH, et al. Diaphragm performance during maximal voluntary ventilation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997;155(2):642–648.
- Ozgocmen S, Cimen OB, Ardicoglu O. Relationship between chest expansion and respiratory muscle strength in patients with primary fibromyalgia. Clin Rheumatol. 2002;21(1):19–22.
- Hwang EG, Lee Y. When will pulmonary function recover after rib fracture? J Exerc Rehabil. 2020;16(1):108–111.
- Firanescu CE, de Vries J, Lodder P, et al. Vertebroplasty versus sham procedure for painful acute osteoporotic vertebral compression fractures (VERTOS IV): randomised sham controlled clinical trial. BMJ. 2018;361:k1551.