Abstract
Background
Patients with type 2 diabetes usually start treatment with oral hypoglycaemic medications once they have been diagnosed. They eventually require insulin injections. We looked into the experiences of such patients with allopathic treatment alternatives over the course of their journey.
Methods
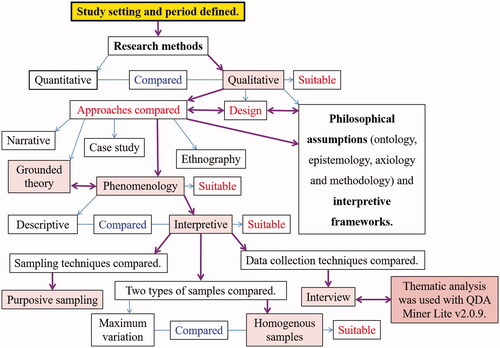
The study was conducted using a qualitative inquiry (phenomenological approach triangulated with modified grounded theory) from July 2019 to January 2020. A total of 24 participants (11 men and 13 women) were recruited purposively and interviewed face-to-face until theoretical saturation was reached. QDA Miner Lite v2.0.9 was used to categorise the data.
Results
The majority of patients had no previous notions regarding their illness. They did not have an emotional reaction to being diagnosed. They were uncomfortable on oral hypoglycaemic agents because of uncontrolled blood glucose and gastrointestinal disturbances, which were thought to be the main causes for medication changes. Initial insulin treatment experiences included fear of injection pain, difficulty self-injecting, and a sense of last resort. Insulin’s effectiveness, ease of injection with a little needle, and lack of gastrointestinal discomfort were all key reasons in changing the patients’ minds about it. Patients have rigorously adhered to insulin since it was found to improve health and bring life.
Conclusion
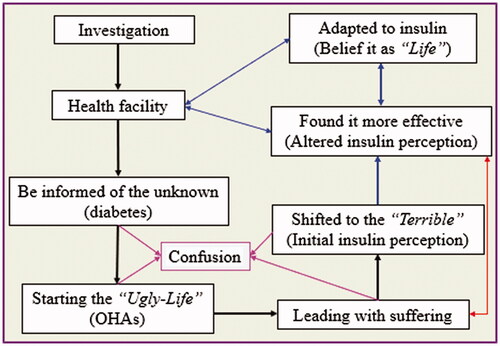
The “life-world” journey of patients with type 2 diabetes with allopathic treatment options was started to be informed of the “unknown” (diabetes), which leads to the “ugly life” (with oral agents), and bridge to and living with the “terrible” (insulin), which was later found to be effective and perceived as “life.”
Patients with type 2 diabetes believed that life with oral hypoglycaemic medications was “boring.”
The major reasons for switching to insulin were “uncontrolled blood sugar levels” and “gastrointestinal disturbances” brought on by oral medications.
Insulin first terrified type 2 diabetes patients, but they eventually referred to it as “life.”
KEY MESSAGES
1. Introduction
Type 2 diabetes mellitus (T2DM) is due to insufficient synthesis of insulin [Citation1–5]. The core pathophysiological features for the development of T2DM are impaired insulin secretion and increased insulin resistance [Citation6,Citation7]. T2DM is mainly caused by insulin resistance [Citation8]. The gradual decline of beta-cell function leads to inadequate insulin production (insulin deficiency) [Citation8–11]. Therefore, eventually, insulin injection becomes mandatory for people with T2DM [Citation7,Citation9,Citation10]. Insulin is among the most effective agents to treat T2DM [Citation12,Citation13]. It is more known about the physiological effects of insulin, but very less on what is going on patients who are using it [Citation10]. Despite its most effectiveness, patients using it were failing to achieve normoglycemia [Citation14].
Diabetes is diagnosed using signs, symptoms, and laboratory tests. Impaired fasting glucose (IFG), fasting plasma glucose (FBS), casual plasma glucose (CPG) or random plasma glucose (RBS), impaired glucose tolerance (IGT), oral glucose tolerance test (OGTT), and glycosylated haemoglobin (HbA1c) are some of the laboratory procedures available [Citation15]. The FBG is favoured because of its ease of use, repeatability, and less link to microvascular problems [Citation16].
The preferred first-line pharmacologic treatment for T2DM is metformin. It should be continued for as long as it is tolerated and not contraindicated once started. It should be supplemented with other medications. However, metformin use for a long time has been linked to biochemical vitamin B12 insufficiency. Therefore, if there is evidence of continuous weight loss, hyperglycaemia, or if HbA1C >10% or blood glucose levels ≥300 mg/dL, early insulin introduction should be considered [Citation17]. In fact, indogeneous insulin secretion eventually becomes insufficient to meet the body’s need [Citation18]. When oral hypoglycaemic agents (OHAs) are no longer effective, insulin treatment is frequently required [Citation4,Citation12]. Insulin therapy, rather than a third oral antidiabetic medicine, should be considered as a third anti-hyperglycemic agent for patients who have had T2DM for 7–10 years, have failed two oral antidiabetic drugs, and have HbA1c levels that are over the tolerable limit [Citation19]. When dietary restrictions and lifestyle changes combined with OHAs have failed to achieve adequate metabolic control, insulin therapy is eventually required [Citation20].
Though other insulin formulations are available, the most basic regimen includes “split mixed” insulin, which consists of twice-daily premixed doses of intermediate-acting and regular insulin. The most frequent concentration is 100 units per millilitre (U-100), with higher concentrations (U-200, U-300, and U-500) reserved for patients who require higher doses [Citation21].
The majority of T2DM patients are initially prescribed oral antidiabetic medication [Citation22]. Immediately after being diagnosed, patients commonly took the prescribed medications for some time [Citation22,Citation23]. The effectiveness of the prescribed medications was then examined by them. Patients either maintained taking the medications or made a range of alterations in response to the self-evaluation [Citation23]. The patients’ negative perceptions of “medication dangers” coexist with a strong belief that “drugs are beneficial,” leading to the idea that diabetic medications are a necessary evil [Citation24].
Patients’ medication taking behaviour, however, differed depending on each lay evaluation method [Citation23]. Accordingly, it is crucial to comprehend patients’ everyday views and experiences in order to create individualised diabetes management plans that could affect how they react to the disease and its treatment [Citation25]. As a result, this study looked into T2DM patients’ reactions to being diagnosed as well as their “life-world” journey as they have pursued allopathic therapy options.
2. Methods
2.1. Ethics approval statement
The study was approved by Wollo University’s College of Medicine and Health Sciences’ “Research, Community Service, and Graduate Coordinating Office” with the reference number CMHS: 443/13/11. All literate participants gave written informed consent prior to the interviews. Participants who were illiterate affixed their fingerprints. The names of those who took part were kept secret. At the time of data collection, no one else was present except the participants. The collected data were kept confidential.
2.2. Design and setting
As illustrated in , a phenomenological study was undertaken in conjunction with modified grounded theory from July 2019 to January 2020 at Dessie Comprehensive Specialised Hospital (DCSH) in Dessie City Administration (DCA), North-East Ethiopia. Grounded theory and phenomenology are the most popular qualitative research approaches [Citation26]. The two most widely used methods were triangulated in this study, which is a crucial aspect of qualitative research [Citation27]. While grounded theory derives from the notion that interactions between people lead to new insights and knowledge, phenomenology emphasises an inner perspective in the form of consciousness and subjectively lived experiences. Lifeworld, consciousness, phenomenological reduction, and essence are key facets of phenomenology. Since they help to create a theory, coding, categories, and core categories are noteworthy components in grounded theory [Citation28]. Instead of finely fragmenting data (e.g. coding data line by line), modified grounded theory creates concepts directly from interpretations of data on an analysis worksheet [Citation29]. Hence, in this study, in order to deeply explore the patients’ life-world and develop a conceptual model of their experiences, phenomenological and modified grounded theory approaches were triangulated [Citation29].
The DCA was established in 1882. It is a multi-ethnic city in Ethiopia’s north-east. The two main religions practiced by the majority of its residents are Orthodox Christianity and Islam [Citation30]. In the city, 85% of the population lives in urban areas. The rest lives in the city’s rural Kebeles [Citation31]. The first language spoken is Amharic, followed by Tigrigna [Citation32]. Dessie is the largest city in North-East Ethiopias region [Citation33], and it is here that the region’s largest and highest tertiary hospital (DCSH) is located, with the largest catchment area. It provides services to almost 8 million people. DCSH offers 13 different types of special services in addition to its usual activities. It had a capacity of more than 500 beds. The hospital employs a total of 925 people, including 616 medical professionals and 309 administrative personnel [Citation34].
2.3. Participants and sample
The participants were T2DM patients who came to DCSH for their treatment follow-up. In order to obtain homogeneous samples () [Citation35], we only included those who had T2DM and were taking insulin. In addition, people with T2DM are advised to use insulin if their condition has advanced and after trying alternative pharmacological treatments. The best way to design evidence-based interventions for such patients is to investigate their life-world views and learn from their experiences. So, they were purposively chosen [Citation36]; i.e. on the basis of being on insulin treatment, having no known or overt psychological disorders, and being able to converse successfully. Aside from these criteria, patients were chosen to represent a wide range of socio-demographics (sex, age, marital status, educational level, religious affiliations). As a preliminary screening, the participants were identified by the lead investigator (EMB) from the diabetes patients’ registration books, which were available at DCSH’s diabetic clinic. However, the participants in the study were adults over 35 years old who were identified by clinicians who worked in DCSH and were familiar with T2DM. EMB then organised his programs according to the patients’ scheduled visits in advance, encountered with them at their appointment time, and informed them sufficiently about the purpose of the study. After providing sufficient information and consent, only those T2DM patients receiving insulin treatment, and who were interested to participate in the study were interviewed. The interviewees were not offered any incentives to participate in the study. There were no repeated interviews conducted. Fortunately, none of the patients who were recruited declined or dropped out.
2.4. Instrument and data collection
The data were collected by the lead investigator (EMB) using an Amharic-language semi-structured interview guide (), through face-to-face in-depth interviews [Citation37], which were recorded using an audio device. Field notes and memos were taken at the same time as the interview. The interviews were conducted during the patients’ scheduled appointments in a variety of peaceful, distraction-free locales (separated locations of the hospital, isolated spots of cafes, work areas of participants and their homes). The interviews were carried out until the data were saturated (with no new idea to be obtained) [Citation38–40]. The interview lasted from 23 to 71 min (average of 46 min).
Table 1. Semi-structured interview guide.
2.5. Data processing and analysis
The lead investigator (EMB) transcribed the interviews verbatim into MS Word and had them double-checked by additional research teams (MHK and BDW). Three analysts (EMB and other Amharic-speaking team members, MHK, and BDW) immersed themselves in the data by separately reading and open-coding transcripts and producing preliminary codes. These three people met on a regular basis to discuss developing themes and revise code definitions, with periodic input from the whole research team, until all of the codes and definitions were agreed upon. For better conceptualisation, the analysis was carried out by reading the transcripts several times. The coding was begun and completed in Amharic, then translated into English and repeated for accuracy. Beginning with the first interview, the coding process was carried out by reading the transcripts line by line. Data collecting and coding processes were carried out concurrently with the analysis. The important quotes from the participants were used to illustrate the study’s findings. The study team held regular discussions on each code and emerging themes in order to deliver accurate results. Finally, the emergent categories were grouped together to form higher-level conceptual themes [Citation41,Citation42]. QDA Miner Lite v2.0.9 was utilised for data analysis.
2.6. Rigour
To ensure data trustworthiness, the researchers used a variety of tactics [Citation43–45]. The interview guide was pre-tested on two patients who were similar but were not deemed research participants. Before being translated into English, the transcripts were returned to the participants. The participants were also informed of the findings, which were validated by the fact that the explanations were based on their own perceptions and experiences. During the research procedure, more than two investigators and methods were involved. “Consolidated criteria for reporting qualitative studies (COREQ)” [Citation46] directed the writing of the study report.
2.7. Reflexivity
The lead investigator (EMB) recognises that the interaction between him and the participants is the study’s outcome [Citation47]. He has been a part of the community since childhood and is quite familiar with the local slang, which may help him better analyse the participants’ experiences from a lay perspective. EMB holds a bachelor’s degree in nursing, a bachelor’s degree in pharmacy, and a master’s degree in social and administrative pharmacy (SAP). Due to his status as a member of the elite as well as a senior pharmacist and nurse, he was an ideal investigator for this study, but the participants saw him as a powerful person. EMB, on the other hand, was cautious about how his personal perceptions influenced the data collection procedure, as well as how the participants responded [Citation48].
3. Results
3.1. Socio-demographic description
A total of 24 patients were interviewed (11 men and 13 women). The average, median, and interquartile range (IQR) of ages were 55, 57, and 58 years, respectively. With diabetes and insulin, respectively, their average longevity was 12 and 5 years ().
Table 2. Description of study participants (n = 24).
Coming to the main findings, five important and interconnected themes were emerged: Labelling, Reactions to being diagnosed, Initilal treatment with OHAs, Justifications for switching to insulin, Insulin therapy (Initial perceptions, Altered perceptions and Outcomes) ().
3.2. Labelling
Diabetes mellitus is known in Amharic as “Ye-Siquar Beshita,” which translates to “Sugar Disease,” while diabetes is known as “Siquar,” which literally means “Sugar.” The term “Siquar” was also used to describe both blood sugar and table sugar. As a result, it must be interpreted in context. Patients have merely indicated their body weight, loss, or rise in numbers without any units, such as 92. For blood glucose level, the same expression was used. Insulin doses were also expressed in a similar fashion. The doses of OHAs were also stated as such. “At the number,” or simply “the number,” was used to describe each syringe’s calibration point. The OHAs are denoted by their dosage form (tablet, or “Knin” or “Kenina” in Amharic), physical size (glibenclamide-small, and metformin-large or big), manner of administration (“Ye-Miwatew” for the oral agent, which literally means to be swallowed), size of dose (5 for glibenclamide, 500, 850, and 1000 for metformin), and well-known brands. Some patients refer to well-known brand names, such as Daonil (glibenclamide). Insulin was referred to simply as “injection.” In Amharic, the medicine insulin and the term injection were both referred to as “Merfe.” The syringe and needle are denoted to as “Mewogia” or “Mewugia,” which literally means “the apparatus for piercing the skin and delivering medicine into the body.” “Merfe” was also sometimes used to express the syringe with its needle. As a result, the term “Merfe” could be understood in a variety of ways.
3.3. Reactions to being diagnosed
The majority of participants said they did not feel anything after being identified as diabetes. They stated that they were not affected in any way. Patients who felt nothing were those who were unaware of their illness. Some patients, however, had emotional reactions such as denial (disbelief), anxiety, confusion, shock, and fear. For individuals who had previously been unaware of their illness, the instant reaction was shocking. Thus, anxiety and shocking were the most common reactions.
When I was initially told I had diabetes, I was terrified, afraid, puzzled, and disoriented. I couldn’t believe what I was hearing. I was hesitant to accept the new, because I was unsure. (Male, 48 years, Bachelor’s degree holder)
It’s a shock. For a little while, I was unsteady due to shock. You can see how difficult it is to live with it (diabetes). It was preferable to be blown away by that shock than to accept the fact that I had diabetes. (Female, 35 years, Illiterate)
Patients who were hesitant to react at first felt anxious about “what could happen next” after learning that diabetes is a chronic condition that cannot be cured and requires lifelong treatment. As a result, they were worried about what might happen next.
I didn’t feel anything at first. Later, when I was told that the drug should not be halted, how could I explain the situation to you? I'm having a hard time deciding what I want to be. (Female, 71 years, Illiterate)
… However, I felt terrible when “Allah” brought me something I didn’t recognise. I felt, but I kept getting more and more and nothing. I’m extremely inconvenient. You’ll never know what will happen to you as a result of it (diabetes). (Male, 58 years, Illiterate)
3.4. Oral therapy and justifications for switching to insulin
The majority of patients began their treatment with OHAs. At first encounter, OHAs were the most commonly prescribed hypoglycaemic medicines (glibenclamide followed by metformin). Uncontrolled blood sugar by OHAs (oral treatment failure) was the most common reason for switching to insulin injection. Side effects of OHAs such as gastrointestinal upset, distress, and irritation, unpleasant taste, and arthritis or joint difficulties were the second most common reasons.
My "Siquar" (blood sugar) was 400, as I told you. That is why he (the doctor) decided to transfer me to injection (insulin). "It (the OHA) did not treat it (diabetes)," the doctor said when it was 400. And replaced it with an injection. (Male, 65 years, illiterate)
I have been unable to eat due to the "Knin" (OHA). My stomach can’t take it anymore. "It switched to the injection (insulin)," he (the doctor) responded after I told him that the "Knin" made me not to eat and tasted unpleasant for my mouth. (Male, 46 years, illiterate)
I started with the big "knin" (metformin). My stomach was suffering. I carry it and appeal when it has bothered me with bad taste too. “It will be changed to an injection (insulin),” they (doctors) said. After that, it was changed to that. (Male, 46 years, illiterate)
Another cause for switching to insulin was weight loss as a result of uncontrolled blood sugar. Doctors’ advice was also a reason in the decision to switch from oral to insulin therapy. The least likely was itching in the pelvic regions, which was thought to be caused by the OHAs’ side effect.
Do I refuse to follow a doctor’s orders? Doctors are professionals who know what they’re doing. They must have told me to modify that (OHA) to this (insulin) for my benefit. And it is at the doctor’s discretion, not mine, that I utilise it. (Male, 66 years, Basic literacy)
My pubis is itchy as well, but there are no weird has evident. It’s perplexing that no line comes out no matter how I lift it up like this (demonstrating the strength of pitching with nails). He (the doctor) told me it was the "Siquar’s" (diabetes) medicine (OHA) issue while I was being evaluated in a hospital. I didn’t say anything about what this is or how it ties to "Siquar." I went to a different hospital to see if it was a skin problem. I'm told I'm not having any problems. My pelvic floor had collapsed, making it impossible for me to move. However, it is devoid of fluid. I couldn’t move, because I was exhausted. Then I returned to the hospital (DCSH), where I was checked and given it (insulin). (Female, 60 years, Basic literacy)
3.5. Insulin treatment
3.5.1. Initial perceptions
The majority of the participants stated that they had no prior knowledge of insulin before starting to use it. Fear of injection pain and perceived problems in self-injecting were the most common reasons for patients to refuse insulin treatment at first, followed by anxiety and perception of last resort.
I was apprehensive about injecting myself. While the doctor switched it (OHA) to "Merfe" (insulin), I refused it for almost three months due to fear of injection. I was hardily wasted. (Female, 42 years, Secondary school completed)
It should be changed to insulin, according to them (doctors). Then, because I was afraid of the injection, I tried to persuade them that adding another oral drug would be preferable to having insulin. (Male, 59 years, Master’s degree holder)
I cried when I saw that an injection (insulin) had been prescribed for me, due to the fact that I dislike injections. (Female, 50 years, Basic literacy)
Patients believe that if insulin is prescribed, they are nearing the end of their lives. They mentioned that because it was the last medicine, if it failed, there would be no other options. According to their explanation, the only thing that will happen following insulin failure is death. So it was felt that trying others first would be preferable to starting an insulin regimen too early.
Fear is the cause for refusing to take "Merfe" (insulin). They (patients) are terrified of "Merfe," because it is the last medicine. "Would you be okay if you were us?" If you’re on "Merfe," you are nearing the conclusion of your life, that your life is coming to a close. (Male, 73 years, Diploma holder)
However, there were circumstances in which patients did not initially refuse insulin.
Most patients use the injection (insulin). They shifted from the "kenina" (OHA) to the injection. To begin with, there are no objections. (Male, 65 years, Illiterate)
3.5.2. Altered perceptions
The relative effectiveness of insulin compared to OHAs was identified to be the primary reason for the participants to change their initial perception. This was thought to be the most important reason for adhering to an insulin regimen.
The "Knin" (OHA) made me feel uneasy. It made my stomach hurt and upset. It also made me lose my appetite, so I didn’t eat anything. But today I consume a well-balanced diet. I'm in good health. My life, I believe, is the "Merfe" (insulin). Because my current physique is vastly different from the one I had when I took the "Knin." There is no longer any increased thirst, frequent urination, or pain. (Female, 42 years, Secondary school completed)
It was previously supposed that it would be uncomfortable in anticipation of a large needle. Patients who found the needle was small, on the other hand, felt at ease and found it easier to inject insulin.
The doctor informed me that the pill was no longer effective. Then I was told that I needed to start taking insulin right away. The insulin injection, on the other hand, was a source of anxiety for me. I was concerned about how I would survive if I had to inject myself. But the needle was small when I started, so it wasn’t a big deal. (Male, 59 years, Master’s degree holder)
The problem was that the previous needle was large and uncomfortable. The needle has now become small in size, making it more comfortable and painless to use. (Male, 73 years, Diploma holder)
I'm frightened about getting an injection. I had no idea how small the needle was. But when I started, I realised it was small and simple. (Female, 42 years, Grade 12 completed)
Participants also believed that life would be impossible without insulin. As a result, since they have considered it to be their life, they were able to adhere to insulin.
Insulin is vital to life. It’s preferable to the "Knin" (OHA) that touches the stomach. (Male, 58 years, illiterate)
Insulin was also found to be suitable for the participants’ bodies. Patients were likewise confident in the prescriptions that their doctors had given them. They trust doctors to know what’s best for them. As a result, adopting their decision was regarded as obligatory.
They (other patients) said it (insulin) was fine. However, I had previously been scared of the injection. However, he (the doctor) advised me to take insulin if my blood sugar level was rising. And I took it because of that (doctor’s advise). The injection does not hurt when I take it. And I'm allowed to eat as much as I want. (Male, 65 years, illiterate)
In rare cases, however, insulin treatment has been reported to be ineffective.
What could I say to you? Insulin will not be able to reduce it (blood glucose). It’s a bit inconsistent, going up and down. It’s pointless. I've just been traumatising with needles. (Female, 70 years, illiterate)
3.5.3. Outcomes
The majority of patients had favourable insulin outcomes. It provided them with numerous advantages, including the avoidance of gastro intestinal disturbances caused by OHAs (improved appetite), improved body image (avoids excessive weight loss), avoided complications, suppressed symptoms (minimized sufferings), improved productivity and psychological tensions and sleep, enhanced treatment adherence (in being effective) and comfort and health, and overall confidence in their ability to survive. The participants stated that they adhered to their insulin therapy. This was due to the fact that it was found to be effective. They stated their thoughts with hope and assurance, as if life would cease to exist without insulin.
Oh, many…many things have altered since I started on insulin. I'm sleeping great, and my body is growing (improved in weight). I am filled with joy and serenity of mind. My body, I believed, craved insulin treatment. (Male. 48 years, Bachelor’s degree holder)
What makes you think I'm a human being? Diabetes ate me alive. I was fat before. Even if it fluctuates, the "Siquar" (blood sugar) level is now normal. (Female, 60 years, Basic literacy)
There was a considerable improvement in the patients’ overall health status after they started insulin treatment.
My physique was quickly deteriorating. They (doctors) tested me with several "Knins" (OHAs), but there was no improvement. As a result, they switched me to "Merfe" (insulin). This is where I started it (DCSH). "Alhamdulillah," I'm alright after that. (Female, 38 years, Illiterate)
I knew that (insulin) was beneficial. When I was taking the "Kenina," I wasn’t living my life. I was 42 in weight, which was pretty low. I thought I was going to pass away. But you must survive if you have "Merfe" (insulin) now. And I reasoned that if there is life, why shouldn’t I take it? And I'm going to take it. (Female, 42 years, Secondary school completed)
4. Discussion
This study revealed that patients had their own expression styles of diabetes. Diabetes mellitus is called “Ye siquar Beshita” in Amharic, which means “Sugar Disease,” while diabetes is called “Siquar,” which literally means “Sugar” [Citation49]. A study conducted in Butajira and Addis Ababa, Ethiopia found similar expressions [Citation50]. This could be owing to the populations’ linguistic and sociocultural similarities. Most participants first reacted to being diagnosed with diabetes with little emotion because they had no prior knowledge of the disease [Citation51]. Another study conducted in Sweden also found that most individuals did not have intense sensations when they were diagnosed with diabetes [Citation52]. After learning of the disease, however, the most common reaction described in this study was concern about “what could happen next?” followed by shock, denial, and confusion. Similarly, many T2DM patients responded with shock when they received their first diagnosis [Citation53]. Given the normal nature of emotional reactivity to undesirable events, the patients’ reluctance to be emotionally reactive to their diagnosis plainly suggests a lack of knowledge of their disease [Citation51], necessitating the need for community-based diabetes awareness intervention.
Rather than the conventional advice of monotherapy with metformin as the first pharmacologic agent for the treatment of T2DM [Citation17,Citation54], glibenclamide was the most commonly prescribed OHA for the initial treatment in this investigation, followed by metformin. The discrepancy in this study could be due to the fact that metformin is a newer medicine than glibenclamide, or it could be due to the patients’ characteristics. This finding contrasts with the findings of another quantitative study conducted in Shanan Gibe Hospital in Southwest Ethiopia, which revealed metformin to be the most commonly prescribed OHA [Citation55]. This could be owing to the difference in sample sizes between the two study designs. However, when compared to the findings of the current study, this quantitative research indicated that the majority of patients had uncontrolled blood glucose while on therapy, which is the same to what was found with OHAs, but the opposite of what was found with insulin [Citation55]. This could be related to patients’ strictest adherence to insulin treatment after being frustrated by the ineffectiveness and adverse effects of OHAs, as well as the fact that they felt insulin to be rather successful and convenient in the belief that it would give them life.
The most common reasons for patients to switch their treatment regimen to insulin were uncontrolled blood glucose by OHAs and gastrointestinal disturbances caused by them, whether at the discretion of their doctors or for personal reasons. Insulin is actually indicated for T2DM individuals who have poor glycemic control [Citation56]; insulin therapy becomes necessary if lifestyle changes and OHAs are ineffective to control blood sugar levels [Citation57].
Patients initially had intense fear of injection pain and difficulty self-injecting when insulin was prescribed (switching from OHAs to insulin) [Citation58]. They also experienced unexplainable fear (apprehension) in the impression of last resort (in believing that insulin is the last drug for diabetes which shows the severity of the disease). Since they believe they are unable to handle the demands of insulin therapy, patients actually experience emotional reactions when first advised to use insulin, which include severe apprehension, discomfort, dejection, or denial [Citation59]. The early poor perceptions of insulin therapy could be related to a lack of knowledge regarding the diease and insulin treatment [Citation51]; because the initiation and adherence to insulin therapy are influenced by patients’ beliefs and knowledge about diabetes and insulin treatment [Citation59].
Although insulin was first thought to be awful for patients, most of them changed their minds after using it. This might be due to the fact that T2DM patients regularly used trial and error in their treatment strategies and help-seeking processes, which are experiential, with continuous evaluation, information seeking, and decision-making [Citation60]. The most common reasons for altered insulin perceptions were its effectiveness, being confident in survival as a result of its effectiveness (perceiving it as life), comfort-ability of insulin needle (easiness to use in being small), feeling of suitability of insulin with body (feeling of internal convenience or absence of gastro-intestinal disturbances), and believing in doctor’s order after being counselled, respectively. Another study conducted in Manchester, UK, reported a similar experience [Citation10].
The majority of the participants in this study strictly adhered to their insulin treatment. They adhered because they found it to be beneficial. Patients in Butajiara and Addis Ababa (Ethiopia) have also been diligent in taking their diabetes medications [Citation50]. When it came to the consequences of their disease (diabetes) [Citation61], the patients mentioned that when they completely adhered to their insulin treatment, complications were eliminated. As a result, practically, all patients indicated that insulin was effective, resulting in excellent outcomes (impacts). The significant positive effect of insulin was that it improved their health. It was also emphasised that the outcome of insulin was the basis for the strictest adherence. They believed that their adherence was a result of its effectiveness, and that their improved health was a result of their adherence [Citation49]. The participants also stated that it improved a wide range of body systems, including improved appetite due to the absence of gastric problems, improved body image (avoid wastage), improved sleep and comfort, and threw suffering symptoms, and most importantly, it increased their confidence in their ability to survive. They believed that, although diabetes took everything they owned, insulin brought everything they did not [Citation49]. A cross-sectional study in Kuwait also indicated that using an insulin pump improved patients’ glycemic control and quality of life (QOL) as a result of better satisfaction and dose adherence [Citation62].
Using insulin, on the other hand, appears to be linked to a 38% increased risk of fracture in people with T2DM in the early stages of the condition. Insulin users were shown to have a 1.35 times higher risk of fracture than non-users [Citation63]. Diabetic retinopathy (DR), particularly proliferative diabetic retinopathy (PDR), was also nearly twice as common in T2DM patients on an insulin regimen compared to those on an OHA regimen. Insulin users had a considerably increased rate of diabetic macular edoema (DME) regardless of staging [Citation64].
4.1. Practical implications
Diabetes treatment aims to maintain overall health, symptom-free living, and QOL by preventing complications [Citation8]. It is necessary for the patient and the health professional to make a joint choice before starting insulin [Citation11]. As a result, therapists must study and comprehend not just the overt behaviour of their patients, but also the covert and underlying attitudes which govern that behaviour [Citation65].
4.2. Limitations
Only those who were undergoing treatment at DCSH were interviewed. Patients with gestational and type 1 diabetes were excluded. It did not take into account T2DM patients who were receiving treatment at other public and private facilities.
5. Conclusion
The majority of patients stated that they were not emotionally affected when they were diagnosed. OHAs were used to begin treatment for almost all of the patients. Suboptimal blood glucose (uncontrolled by OHAs) and OHAs side effects were the main reasons for switching to insulin. When they were first prescribed insulin, they had unfavourable feelings about the pain of injections, the difficulty of self-injecting, and the need to use it as a last resort. However, when they found that insulin was effective and better, they changed their minds. They adhered to it, and their health improved as a result. So, they saw it as “life.”
Author contribution
Ewunetie Mekashaw Bayked: Conceived and designed the research; Performed the research; Analysed and interpreted the data; Contributed inputs, materials, analysis tools or data; Wrote the paper. Mesfin Haile Kahissay and Birhanu Demeke Workneh: Conceived and designed the research; Performed the research; Analysed and interpreted the data.
Acknowledgments
First and foremost, we would want to express our gratitude to all of the study participants for their time, voluntary participation, and information sharing. Second, we would like to thank all of the nurses, general practitioners, and physicians who work at DCSH’s diabetes clinic. Finally, we are grateful to DCSH’s planning and programming, as well as its human resource departments, for supplying us with appropriate information regarding the hospital.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available within the article.
References
- ASFAW AA. Appropriateness of Type 2 diabetes mellitus drug therapy: a case of Tikur Anbessa Specialized Hospital Diabetes Clinic Thesis. Addis Ababa University; 2014.
- Novy TR. 2011. The Lived experience of Native Americans diagnosed with type 2 diabetes mellitus. University of Wisconsin Oshkosh, Oshkosh, Wisconsin (USA):3.
- Parry O, Peel E, Douglas M, et al. Issues of cause and control in patient accounts of type 2 diabetes. Health Educ Res. 2006;21(1):97–107.
- Petznick A. Insulin management of type 2 diabetes mellitus. Am Fam Phys. 2011;84(2):183–190.
- Tesfamariam A. 2016. Comparative study between dpp-4 inhibitors based therapies and other Non-Insulin based therapies among type 2 diabetes patients in Addis Ababa Ethiopia [thesis]. Addis Ababa University.
- Kaku K. Pathophysiology of type 2 diabetes and its treatment policy. Jpn Med Assoc J. 2010;53:41–46.
- Wong J, Tabet E. The introduction of insulin in type 2 diabetes mellitus. Aust Fam Phys. 2015;44(5):278–283.
- Ayubah NL, Peltonen J. 2018. Experiences of type 2 diabetes patients with nursing care: a literature review. JAMK University of Applied Sciences, Jyväskylä, Finland:4.
- Hamaty M. Insulin treatment for type 2 diabetes: when to start, which to use. Cleve Clin J Med. 2011;78(5):332–342.
- Morris JE, Povey RC, Street CG. Experiences of people with type 2 diabetes who have changed from oral medication to self-administered insulin injections: a qualitative study. Pract Diab Int. 2005;22(7):239–243.
- Tan AM, Muthusamy L, Ng CC, et al. Initiation of insulin for type 2 diabetes mellitus patients: what are the issues? A qualitative study. Singapore Med J. 2011;52(11):801–809.
- Chen KW, Tseng H-M. The barriers to initiating insulin therapy among people with type 2 diabetes in Taiwan - a qualitative study. J Diabet Metabol. 2012;3:5.
- Lee YK, Ng CJ, Lee PY, et al. What are the barriers faced by patients using insulin? A qualitative study of Malaysian health care professionals’ views. Patient Prefer Adherence. 2013;7:103–109.
- Tong WT, Vethakkan SR, Ng CJ. Why do some people with type 2 diabetes who are using insulin have poor glycaemic control? A qualitative study. BMJ Open. 2015;5(1):e006407.
- Hopper PD. 2007. Nursing care of patients with disorders of the endocrine pancreas. In: Understanding medical surgical nursing. 3rd ed. Philadelphia (PA): F. A. Davis Company; p. 851–875.
- Mahler RJ, Adler ML. Type 2 diabetes mellitus: update on diagnosis, pathophysiology, and treatment. J Clin Endocrinol Metab. 1999;84(4):1165–1171.
- American Diabetic Association. Standards of medical care in diabetes—2019 abridged for primary care providers. Clin Diabet. 2019;37(1):11–34.
- Home P, Riddle M, Cefalu WT, et al. Insulin therapy in people with type 2 diabetes: opportunities and challenges? Diab Care. 2014;37(6):1499–1508.
- LaSalle JR, Berria R. Insulin therapy in type 2 diabetes mellitus: a practical approach for primary care physicians and other health care professionals. J Am Osteopath Assoc. 2013;113(2):152–162.
- Bretzel RG, Eckhard M, Landgraf W, et al. Initiating insulin therapy in type 2 diabetic patients failing on oral hypoglycemic agents: basal or prandial insulin? The APOLLO trial and beyond. Diabetes Care. 2009;32 Suppl 2(2):S260–S265.
- Wells BG, DiPiro JT, Schwinghammer TL, et al. 2017. Diabetes mellitus. In: Pharmacotherapy handbook. 10th ed. New York (NY): McGraw-Hill Education.
- Ahmad A, Khan MU, Aslani P. A qualitative study on medication taking behaviour among people with diabetes in Australia. Front Pharmacol. 2021;12:693748.
- Widayanti AW, Norris P, Heydon S, et al. Medicine taking behaviours of people with type 2 diabetes in Indonesia: a qualitative study. Int J Clin Pharm. 2020;42(1):31–39.
- McSharry J, McGowan L, Farmer AJ, et al. Perceptions and experiences of taking oral medications for the treatment of type 2 diabetes mellitus: a systematic review and meta-synthesis of qualitative studies. Diabet Med. 2016;33(10):1330–1338.
- Widayanti AW, Heydon S, Norris P, et al. Lay perceptions and illness experiences of people with type 2 diabetes in Indonesia: a qualitative study. Health Psychol Behav Med. 2019;8(1):1–15.
- Urcia IA. Comparisons of adaptations in grounded theory and phenomenology: Selecting the specific qualitative research methodology. Int J Qual Methods. 2021;20:160940692110454.
- Zeegers M, Barron D. Method. In: Zeegers M, Barron D, editors. Milestone moments in getting your PhD in qualitative research. Walthan (MA): Chandos Publishing; 2015. p. 75–85.
- Strandmark M. Method development at nordic school of public health NHV: phenomenology and grounded theory. Scand J Public Health. 2015;43(16 Suppl):61–65.
- Akiko K. 2018. Qualitative research and a modified grounded theory approach: the Tsuru University review. Tsuru, Japan: Tsuru University; p. 47–58.
- Balcha A. 2019. Charting the history of Dessie. [cited 2019 Dec 24]. Available from: https://wollo.org/local-history-dessie
- Central Statistical Agency 2013. Population projection of Ethiopia for all regions at wereda level from. 2014–2017. Addis Ababa, Ethiopia: Central Statistical Agency of Ethiopia.
- Central Statistical Agency 2007. Ethiopian population and housing census report. Addis Ababa, Ethiopia: Central Statistical Agency of Ethiopia.
- Dimon M. 2018. The largest cities in Ethiopia. In: Ethiopian Gazette. Available from: https://ethiopiangazette.com/the-largest-cities-in-ethiopia.
- Getachew D. 2020. Annual report. Dessie, Ethiopia: Dessie Comprehensive Specialized Hospital (DCSH).
- Al-Busaidi ZQ. Qualitative research and its uses in health care. Sultan Qaboos Univ Med J. 2008;8(1):11–19.
- Palinkas LA, Horwitz SM, Green CA, et al. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–544.
- Moser A, Korstjens I. Series: Practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract. 2018;24(1):9–18.
- Dworkin SL. Sample size policy for qualitative studies using in-depth interviews. Arch Sex Behav. 2012;41(6):1319–1320.
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–1760.
- Vasileiou K, Barnett J, Thorpe S, et al. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol. 2018;18(1):148.
- Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE guide no. 131. Med Teach. 2020;42(8):846–854.
- Nowell LS, Norris JM, White DE, et al. Thematic analysis: Striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):160940691773384.
- Korstjens I, Moser A. Series: practical guidance to qualitative research. Part 4: trustworthiness and publishing. Eur J Gen Pract. 2018;24(1):120–124.
- Shenton A. Strategies for ensuring trustworthiness in qualitative research projects. EFI. 2004;22(2):63–75.
- Stahl N, King J. Expanding approaches for research: understanding and using trustworthiness in qualitative research. J Dev Educ. 2020;44:26–28.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357.
- Dodgson JE. Reflexivity in qualitative research. J Hum Lact. 2019;35(2):220–222.
- Olmos-Vega FM, Stalmeijer RE, Varpio L, et al. A practical guide to reflexivity in qualitative research: AMEE guide no. 149. Med Teach. 2022;44(4):1–11.
- Mekashaw E, Demeke B, Haile M. Recognition of symptoms, mitigating mechanisms and self-care experiences of type 2 diabetes patients receiving insulin treatment in North-East Ethiopia. Emerald Open Res. 2022;3:14.
- Habte BM, Kebede T, Fenta TG, et al. Explanatory models of adult patients with type 2 diabetes mellitus from urban centers of Central Ethiopia. BMC Res Notes. 2016;9(1):441–451.
- Bayked EM, Workneh BD, Kahissay MH. Thirst for information and needs reflections of type 2 diabetes patients receiving insulin treatment in North-East Ethiopia: a qualitative exploration. J Prev Med Public Health. 2021;54(2):119–128.
- Pikkemaat M, Boström KB, Strandberg EL. “I have got diabetes!” – interviews of patients newly diagnosed with type 2 diabetes. BMC Endocr Disord. 2019;19(1):53.
- Zimmermann M, Bunn C, Namadingo H, et al. Experiences of type 2 diabetes in Sub-Saharan Africa: a scoping review. Glob Health Res Policy. 2018;3(1):25–37.
- Wexler DJ. 2020. Management of persistent hyperglycemia in type 2 diabetes mellitus. Available from: https://www.uptodate.com/contents/management-of-persistent-hyperglycemia-in-type-2-diabetes-mellitus
- Yigazu DM, Desse TA. Glycemic control and associated factors among type 2 diabetic patients at shanan gibe hospital, southwest Ethiopia. BMC Res Notes. 2017;10(1):597.
- Ishii H, Iwamoto Y, Tajima N. An exploration of barriers to insulin initiation for physicians in Japan: Findings from the diabetes attitudes, wishes and needs (DAWN) Japan study. PLoS One. 2012;7(6):e36361.
- Zhang Y, Xie Y-j, Meng D-D, et al. Clinical study of treatment switching from premixed insulin to basal insulin combined with oral hypoglycemic drugs in patients with type 2 diabetes. Diabetol Metab Syndr. 2014;6(1):37.
- Liu C, De Roza J, Ooi CW, et al. Impact of patients’ beliefs about insulin on acceptance and adherence to insulin therapy: a qualitative study in primary care. BMC Prim Care. 2022;23(1):15.
- Kalra S, Bajaj S, Sharma SK, et al. A practitioner’s toolkit for insulin motivation in adults with type 1 and type 2 diabetes mellitus: evidence-based recommendations from an international expert panel. Diabetes Ther. 2020;11(3):585–606.
- Low LL, Tong SF, Low WY. Selection of treatment strategies among patients with type 2 diabetes mellitus in Malaysia: a grounded theory approach. PLoS One. 2016;11(1):e0147127.
- Bayked EM, Workneh BD, Kahissay MH. Sufferings of its consequences; patients with type 2 diabetes mellitus in North-East Ethiopia, a qualitative investigation. Heliyon. 2022;8(2):e08871.
- Alsairafi ZK, Smith FJ, Taylor KMG, et al. A qualitative study exploring patients’ experiences regarding insulin pump use. Saudi Pharm J. 2018;26(4):487–495.
- Losada-Grande E, Hawley S, Soldevila B, et al. Insulin use and excess fracture risk in patients with type 2 diabetes: a propensity-matched cohort analysis. Sci Rep. 2017;7(1):1–9.
- Jingi AM, Noubiap JJN, Essouma M, et al. Association of insulin treatment versus oral hypoglycaemic agents with diabetic retinopathy and its severity in type 2 diabetes patients in Cameroon, Sub-Saharan africa. Ann Transl Med. 2016;4(20):395–395.
- Abolghasemi R, Sedaghat M. The patient’s attitude toward type 2 diabetes mellitus, a qualitative study. J Relig Health. 2015;54(4):1191–1205.