Abstract
Introduction
Adverse healthcare-related events (AE) entail reduced patient safety. Estimating their frequency, characteristics, avoidability and impact is a means to identify targets for improvement in the quality of care.
Methods
This was a descriptive observational study conducted within the Patient Safety Incident Study in Hospitals in the Community of Madrid (ESHMAD). The study was conducted in a high-complexity hospital in May 2019 through a two-phase electronic medical record review: (1) AE screening and epidemiological and clinical data collection and (2) AE review and classification and analysis of their impact, avoidability, and associated costs.
Results
A total of 636 patients were studied. The prevalence of AE was 12.4%. Death during the stay was associated with the presence of AE (OR [CI95%]: 2.15 [1.07 to 4.52]) versus absence and emergency admission (OR [CI95%]: 17.11[6.63 to 46.26]) versus scheduled. A total of 70.2% of the AEs were avoidable. Avoidable AEs were associated with the presence of pressure ulcers (OR [CI95%]: 2.77 [1.39 to 5.51]), central venous catheter (OR [CI95%]: 2.58 [1.33 to 5.00]) and impaired mobility (OR [CI95%]: 2.24[1.35 to 3.71]), versus absences. They were associated too with the stays in the intensive care unit (OR [CI95%]: 2.75 [1.07 to 7.06]) versus medical service. AEs were responsible for additional costs of €909,716.8 for extra days of stay and €12,461.9 per patient with AE.
Conclusions
The prevalence of AEs was similar to that found in other studies. AEs led to worse patient outcomes and were associated with the patient’s death. Although avoidable AEs were less severe, their higher frequency produced a greater impact on the patient and healthcare system.
Adverse events are one of the main problems in healthcare delivery and patients who suffer from at least one AE are double as likely to die during hospitalization.
Avoidable adverse events are the most frequent in health care and they are a good target where achieve improvement areas that allow getting optimal patient safety and quality of care levels.
Patients hospitalized in the ICU, with the previous presence of pressure ulcers, central venous catheter, or impaired mobility were associated with the development of avoidable AE, so optimal management of these patients would reduce the impact of AE.
Key messages
Introduction
The Conceptual Framework for the International Classification for Patient Safety, published in 2009 by the World Health Organization (WHO), defines adverse healthcare-related events (AE) as incidents that occur during medical care and harm a patient, producing an injury, suffering, disability, or death [Citation1]. They are among the main hospital care problems [Citation2], compromising the optimal quality of care and causing an unnecessary increase in mortality and healthcare costs [Citation3]. AEs may be the third leading cause of death in the United States [Citation4]. AEs are one of the areas for improvement within the field of Patient Safety. Due to their importance, the realization of policies aimed at combating AEs and promoting the culture of safety are strategies that allow mitigation of their impact [Citation5].
The first step to achieving it is to measure the frequency of AEs to know the magnitude of the problem. To this end, Brennan et al.’s (Harvard Medical Practical Study [HMPS], 1991) methodology [Citation6] is the most widely used, replicated, and validated, allowing high comparability [Citation7] and generating a body of scientific evidence. According to the studies conducted with this methodology, the incidence of AEs ranges from 3.7 to 37%, half of them avoidable [Citation8–13]. Subsequent works have estimated a prevalence of 11% [Citation13]. The high frequency and the impact of AEs prompted the publication of the To Err is Human [Citation14] report in 2000 and the development of numerous medical error prevention programmes [Citation15,Citation16].
Avoidable AEs are particularly significant, as they are associated with the patient’s death at the end of the hospitalization [Citation17]. Avoidability ranges from 30 to 84% [Citation18] of AE, meaning there is intrinsic potential for developing measures for improvement [Citation19,Citation20], and studying these AEs is an efficient means to improve the quality of care.
Although numerous studies have been made focused on AEs, there’s a lack of evidence of the risk factors related to avoidable AEs. Also, very few works have analysed the relationship between AEs and the patient’s death. Under this premise, this study, which was included in the Patient Safety Incident Study in Hospitals in the Community of Madrid (ESHMAD) [Citation21,Citation22], arises intending to analyze in a pioneering way the factors related to avoidable AEs. Other objectives were to measure the prevalence of AEs, their association with patients’ death during hospitalization, and the economic cost of AEs in a high-complexity hospital. With this, it is intended to improve knowledge of AEs and find potential areas for improvement in Patient Safety.
Materials and methods
Design and sample selection
This was a cross-sectional, descriptive, observational study. All patients hospitalized in a high-complexity hospital and identified in a cross-section drawn at the beginning of a day of care in the second week of May 2019 were included. According to the methodology, patients needed to be hospitalized during the first phase of the study. Each hospitalization ward was assigned to a reviewer, in such a way that they had to perform the cross-sectional cut on one of those days of the week. Patients admitted within the previous 24 h or in the Emergency Department were excluded. The study was conducted according to the Brennan et al. methodology in the Harvard Medical Practice Study (HMPS) [Citation6], in two phases:
AE Screening with the AE Screening Guide, based on the Screening Review Form by Brennan et al. [Citation6,Citation23], modified after the ENEAS [Citation12,Citation24], IBEAS [Citation13], and EPIDEA [Citation25] studies, and adapted for the simultaneous conducting of the Prevalence of nosocomial infections in Spain study (EPINE) [Citation26]. The Screening Review Form is validated too with high sensitivity for the screening of AE, with a negative predictive value of 99.5% [Citation23]. Epidemiological variables were gathered from all patients included in the sample. This phase was performed by healthcare workers.
AE checking, classification, and characterization phase applying the Spanish version of the Modular Review Form 2 (MRF2) [Citation12,Citation13,Citation24,Citation27]. This is a validated form that was applied solely to those screened as positive in the previous phase and classified as AE (calibrated events) or as false positives (if no potential or active AEs were detected at the study time). Furthermore, MRF2 allowed AE to be classified and their impact and avoidability assessed. Healthcare professionals with specific training performed a peer review of all patients included in this phase. The grade of reliability of this tool estimated in previous studies was good (kappa = 0.61) [Citation6].
The study was conducted based on a partial sample of the Patient Safety Incident Study in Hospitals in the Community of Madrid (ESHMAD) database. The ESHMAD study wanted to estimate the prevalence of AEs in 34 public hospitals in the Community of Madrid [Citation21,Citation22]. ESHMAD database was used also in another work, which focused on how surgical interventions could increase the risk of developing an AE in the surgical patients of the whole sample [Citation28].
Study variables
All variables were gathered based on previous studies conducted [Citation29], such as age, patient sex, type of hospitalization service (classified as medical speciality, surgical, intensive care unit [ICU], paediatric, and psychiatry), presence or absence of intrinsic risk factors (IRF) (renal failure, cardiovascular disease, neoplasm, chronic obstructive pulmonary disease, immunodeficiency, neutropenia, cirrhosis of the liver, hypoalbuminaemia, pressure ulcers, impaired mobility, sensory deficits, obesity, and active smoking), presence or absence of extrinsic risk factors (ERF) (previous surgery, peripheral vascular catheter, central vascular catheter, urinary intubation), the reason for discharge, pre-screening stay, and total stay. The Charlson Comorbidity Index was also calculated to estimate the degree of comorbidity prior to admission [Citation30].
The type of AE was recorded, and the impact on the patient was studied by recording the number of days of stay and the additional treatments administered as a result. The severity of AE was classified by applying the Conceptual Framework for the International Classification for Patient Safety, published by WHO in 2009 [Citation1]: 'mild’ for AE that did not affect management or length of hospitalization; 'moderate’, leading to readmission or additional days in hospital and; 'severe’ if the patient required further surgery or it contributed to permanent disability or death.
The following were also analysed: (1) relationship between potential AE and health care and (2) degree of avoidability of the AE. A validated and specific scale of the MRF2 was applied to both [Citation5,Citation23], (a scale of 1 to 6; being '1′ 'minimal relationship/evidence’, and '6′ an 'almost-certain relationship/evidence’; values ≥4 were considered positive).
The cost associated with additional days of hospitalization derived from AE was estimated, both overall and broken down according to whether or not AE were avoidable. For these purposes, the costs attributable to the additional days of stay for each Care Unit were calculated using monetary equivalents provided by the hospital’s accounting department for 2019. A specific monetary equivalence was used for each Care Unit.
Statistical analysis
First, a descriptive and bivariate analysis per patient was carried out. For this, central (mean and median) and dispersion measures (standard deviation [s] and interquartile range [IR]) were used in quantitative variables, and proportions were estimated for qualitative variables. For bivariate analysis with hypothesis contrast test: in quantitative variables, the Student t or Mann–Whitney U were used after evaluating their normal distribution; in qualitative variables, the chi-square or Fisher test was used according to whether it was parametric or non-parametric. Values of p < 0.050 were considered statistically significant.
In the second place, variables associated with a patient’s death were explored through a predictive multivariate logistic regression analysis. After exploring association in a bivariate analysis, a backward modelling strategy was used with an output p-value of 0.100. To correct the overoptimism of the model, resampling techniques (Bootstrap) were used, and goodness of fit was measured with the Hosmer-Lemeshow test. Charlson index was kept in the model because it was related to a bad prognosis [Citation30].
After that, records with AE were analysed. A descriptive and bivariate analysis was carried out, stratifying by the avoidance of the AE. The type of AE, time of appearance of the AE, severity, direct health care derived from the AE, and modification of stay were analysed. The total cost of the AEs was estimated from the days of stay added per care unit. For bivariate analysis with hypothesis contrast test: in quantitative variables, the Student’s t or Mann–Whitney U tests were used after evaluating their normal distribution; in qualitative variables, the chi-square or Fisher test was used according to whether it was parametric or non-parametric. Again, values of p < 0.050 were considered statistically significant.
Finally, variables associated with avoidable AE records were explored through a predictive multivariate logistic regression analysis. In this model, non-avoidable AE records were excluded to avoid possible bias. A backward modelling strategy was used with an output p-value of 0.100. To correct the overoptimism of the models, resampling techniques (Bootstrap) were used, and goodness of fit was measured with the Hosmer-Lemeshow test.
STATA version 16 software was used for statistical analysis [Citation31].
Ethics committee
ESHMAD study was approved on 19 March 2019 by the Ethics Committee of the Hospital Universitario Ramón y Cajal (reference 057/19), guaranteeing the anonymity and custody of the data gathered, which were transcribed to an anonymized online database, with security mechanisms and safeguarding of personal data.
The economical cost of AE was a secondary objective and the cost of each hospitalization day was only requested in this sample.
Results
Sample characteristics
A total of 636 patients met the inclusion criteria. The mean age was 66.5 years, and the median age was 70 years. No relevant differences were found concerning sex. A 66.3% of the admissions were urgent, and the medical area had the largest number of patients (46.4%). The mean and median pre-screening stay was 12.5 and 5.0 days, respectively. A 6.3% of patients died during admission ().
Table 1. Prevalence of adverse events according to patient and hospital admission characteristics.
A 93.1% of the sample presented ≥1 IRF, the most frequent of which being cardiovascular disease (in 54.4% of the sample), impaired mobility (37.6%), and neoplasm (32.7%). A 75.8% of the sample had ≥1 ERF, the most frequent being a peripheral venous catheter (65.3%), followed by the urinary catheter (21.1%) and the central venous catheter (17.1%) (Table S1 in Supplementary Material).
Prevalence of AE by study phase
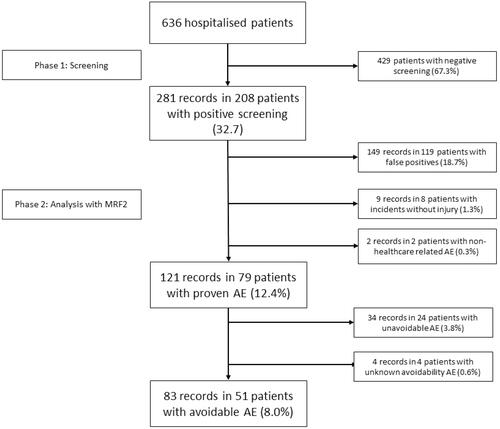
Of the 636 patients included, a positive screening item was detected in 208 (32.7%). After applying MRF-2 (second phase), 121 AE were identified in 79 patients (prevalence of AEs patients of 12.4%). Of the rest of the patients with positive screening, 119 were false-positive (18.7%), eight had no-harm incidents (1.3%), and two had AE concerning unproven health care (0.3%). Of the 121 AEs, 83 were classified as avoidable in 51 patients (8.0% prevalence). Of the remainder, 34 AEs found in 24 patients had non-avoidable AEs (3.5%), and 4 had non-assessable avoidable AEs ().
Factors associated with AEs
The highest prevalence of AEs was in the ICU (36.1%), followed by surgical services (11.6%), medical (11.5%), paediatrics (5.6%), and psychiatry (0.0%; p < 0.001). When comparing patients with ≥1 AE versus those without AE, a greater mean age (71.9 years, compared with 65.7; p = 0.021) and previous stay (28.0 days, compared with 10.3; p < 0.001) were observed. In addition, a higher prevalence of AE was detected in patients undergoing surgery (16.2% versus 10.1%; p = 0.025).
The prevalence of AEs increased with the number of IRF (2.3% for patients without IRF; 10.2% for 1 IRF; 8.1% for 2 IRF; and 15.6% for ≥3 IRF; p = 0.014), with significant differences for pressure ulcers (39.4% versus 11.0%; p < 0.001), hypoalbuminaemia (18.9% versus 9.5%; p < 0.001), impaired mobility (18.4% versus 8.8%; p < 0.001), CVA (16.5% prevalence versus 7.5%; p < 0.001), and sensory deficit (17.5% versus 11.0%; p = 0.040).
The gradual increase in ERF meant an increase in the prevalence of AEs (6.5% for patients without ERF; 10.9% for 1 ERF; 21.1% for 2 ERF; and 26.3% for ≥3 ERF; p < 0.001), with significant differences for the presence of urinary catheter (20.9%, versus 12.2%; p < 0.001), central venous catheter (20.2% versus 10.9%; p = 0.008), and peripheral venous catheter (14.5% versus 8.7%; p = 0.039). Additional information on all the IRF and ERF analysed are provided in Table S1 in Supplementary Material.
Association between death and AE
Of the 636 patients, 40 died during admission. As a result, there was a higher prevalence of AEs (30.0% among deceased patients versus 11.2 in the non-deceased; p < 0.001) ().
Table 2. Association between death and detection of AEs.
When adjusted for age, sex, Charlson Index, admission type, and type of service, urgent admission entailed a 17.1 increase in the risk of death (OR[CI95%]: 17.11[6.33 to 46.26] versus scheduled admission), as well as ICU stay (OR[CI95%]: 5.77[1.74 to 19.15], versus stay in medical speciality), being a man (OR[CI95%]: 2.16[1.01 to 4.64 versus a woman], the presence of AE (OR[CI95%]: 2.15[1.07 to 4.52], versus absence) and age (OR[CI95%]: 1.04[1.01 to 1.07] for each year of increase) ().
The goodness of fit of the model was evaluated with the Hosmer-Lemeshow test, obtaining a value p = 0.109, and no differences were observed between the findings and what was expected.
Impact and avoidability of AEs
A total of 121 AEs were detected in the 79 patients. The most frequent type of AE were healthcare-associated infections (HCAI; 44.6%), complications of a procedure (24.8%) and complications of care (19.8%). 55.4% of AEs occurred during care on the ward, 61.1% were moderate or severe, and 99.2% affected subsequent health care. In addition, 59.5% of AEs lengthened the hospital stay or led to readmission, adding a total of 2,001 days of hospitalization and 206 days of ICU stay (17.3 and 1.7 days on average, respectively). The total direct economic cost of extending stays because of AEs was €909,716.8 and €12,461.9 per patient with AE.
Avoidability was evaluated in 117 AEs; 83 were avoidable (70.9%). The most frequent types of avoidable AEs were HCAI (42.2% of the total preventable AE), followed by complications of care (28.9%) and complications of a procedure (16.9%). The 24 AE (100.0%) produced by care complications were considered avoidable. 49.4% of avoidable AEs had a moderate-severe impact (compared with 85.3% in non-avoidable; p < 0.001) and 47.0% extended hospital stay or readmission (compared with 85.3% of non-avoidable; p < 0.001). The total number of days of hospitalization and ICU stay caused by avoidable AEs were 1,183 and 151 days, respectively. The direct economic costs of avoidable and non-avoidable AEs were €581,643.0 and €328,083.8, respectively ().
Table 3. Types of AE and their impact by avoidability.
Adjusting risk factors associated with records with avoidable AEs in a multivariate model revealed an association for their development with the previous presence of pressure ulcers (OR[CI95%]: 2.77 [1.39 to 5.51]), with ICU admission (OR[CI95%]: 2.75 [1.07 to 7.06]), compared with admission to medical speciality, the central venous catheter (OR[CI95%]: 2.58 [1.33 to 5.00]) and impaired mobility (OR[CI95%]: 2.24 [1.35 to 3.71]), as opposed to their absence. In addition, the model showed optimal goodness of fit (Hosmer-Lemeshow Test: p = 0.434) ().
Table 4. Risk factors associated with avoidable AE records.
Discussion
A prevalence of AE of 12.4% was detected, the most frequent of which were HCAI (44.6%). About half had moderate-severe consequences for patients, and 59.5% led to an extended hospital stay, with an additional 2,093 days of hospitalization and an associated cost of €909,716.8. In addition, 99.2% of AEs required additional health care. The gradual increase in IRF and ERF resulted in a dose-response increase in the prevalence of AEs, associated with cardiovascular disease, hypoalbuminaemia, impaired mobility, and pressure ulcers in IRF and urinary catheter, peripheral venous catheter, and central venous catheter in ERF. 30% of deceased patients had AEs, and overall avoidability was 70.9%.
First of all, the methodological design is of interest to give context. As part of the measurement of AEs, the Brennan et al. study in New York, United States, in 1991 marked the beginning of the development of studies using the HMPS methodology, allowing comparability of results [Citation6]. This study and those performed subsequently by Thomas et al. in Utah and Colorado in 1992 [Citation8], Wilson et al. in Australia in 1995 [Citation9] and Vincent et al. in the UK in 2001 [Citation10] assessed the impact of medical errors and AEs from longitudinal designs. Although it establishes causality relationships and identifies a greater number of AEs, this methodology consumes more resources and makes it difficult to assess trends in time. Adapting the HMPS methodology [Citation6] to a cross-sectional design allows efficient hospital AEs surveillance. Identifying longer AEs from a briefer review of the EMR and making it possible to compare the results of the Hospital in cross-sectional sections performed at different times [Citation32,Citation33].
The estimated frequency of AEs in other studies ranges from 3% of Brennan et al. [Citation6] and Thomas et al. [Citation8] – who only analysed episodes to find one AE per patient – to 34.0% of Larsen et al. in paediatric ICUs in 2007 [Citation34]. Later, in Spain, in 2005, the ENEAS study detected an incidence of AEs of 9.3% and was the first to analyse the total AEs per episode [Citation12]. In a meta-analysis by Schwendimann et al. in 2018 [Citation35], the frequency of AEs was 10.0%, and the most frequent type of AE was complications of a procedure, followed by adverse drug effects and HCAI. This difference in the most frequent types of AEs detected in our study is explained for two reasons. On the one hand, there is a lack of consensus in the classification of the types of AE. In this study, we have used the criterion established by the EPINE study, which sets out to be sensitive in detecting them [Citation26]. The second reason is the cross-sectional methodology. HCAI tends to prolong hospital stay compared to other AEs, so its proportion in a cross-sectional area is possibly overestimated. However, this has no impact on the study.
In our study, a prevalence of AEs of 12.4% is an intermediate value for high-complexity hospitals. It should be contextualized with other cross-sectional design studies, such as the IBEAS, conducted in 2009 in 58 medium and high-complexity hospitals in Argentina, Colombia, Costa Rica, Mexico, and Peru [Citation13]. This study showed a prevalence of 10.5% and almost 12.0% in high-complexity hospitals. HCAI was also the most frequent type of AE (37.1%), and more than 60.0% had a moderate-severe impact on the patient. A lower frequency of AEs was observed among paediatric patients, consistent with the findings of Requena et al. in 2011 [Citation36]. Patients who had been in hospital for longer when screened had a higher prevalence of AEs, which could be caused by the AEs prolonging the hospital stay in 50% of cases. This proportion of AEs that prolonged the hospital stay is consistent with the findings of Sousa et al. in 2018 [Citation37].
A 15.2% of patients with AE died during their hospital stay. This relationship was originally studied by Brennan et al. descriptively, with 13.6% of AEs associated with patient death [Citation6]. In 2004, Baker et al. in Canada found 15.9% [Citation11]. More recent studies, such as that of Tartaglia et al. in Italy in 2012 [Citation38], and Sousa et al. in Portugal, in 2014 [Citation39], found 10.6% and 10.8%, respectively. These figures are slightly lower than in our study, although longitudinal.
On the other hand, the transversal design tends to over-represent AEs with more serious consequences for the patient, thus overestimating the proportion of AEs associated with death [Citation33]. In the IBEAS study, 5.7% of AEs were associated with death, but the sample is of limited comparability, this being a younger population (median age 45 years versus 70 years in this study) [Citation13]. This study estimated an adjusted measure of association as to how much the risk of dying from AE increases. This value was more than twice as high (OR[CI95%]: 2.15[1.07 to 4.52]) adjusted by age, sex, type of admission, Charlson Index, and type of service, the association being congruent with what was found in the study of Martins et al. in Brazil, in 2011, which estimated an OR of more than 9 [Citation17].
A total of 70.9% of the AEs identified were avoidable. The avoidability value was higher than that observed by Lessing et al. and Panigioti et al. in their meta-analyses of 2010 and 2019, respectively (50.0%, regardless of the type of care area), with a similar impact on the patient (half of AE with moderate-severe impact) [Citation18,Citation40]. Also, it has been found that 100% of AEs related to care complications were classified as avoidable. This data is variable in scientific literature, but the trend is consistent with this result. The meta-analysis by Panigioti et al. found that adverse drug effects (25%) and complications in care (24%) were the most avoidable [Citation18]. and a study by D'amour et al. in Canada in 2014 estimated that inadequate care was responsible for 76.8% of AE, which were, therefore, the most avoidable [Citation41]. HCAI were classified as avoidable in 66%, slightly more than the 60% found by Corrales-Fernandez et al. in 2011 [Citation42].
Regarding hospitalization days, in this study, avoidable AEs caused more days of additional stay than unavoidable AEs (1,203 additional days of stay, compared with 819 days of unavoidable AEs), resulting in higher associated direct economic costs (€581,643.0, compared with €328,083.8, respectively). If this estimate is extrapolated to the 70 hospitals in Spain with more than 500 beds [Citation43], the avoidable AEs suffered by hospitalized patients derived from a cross-section would mean extra costs of €40.7 million.
Limitations
The main limitation of this study lies in its cross-sectional design, which over-represents the AEs that prolong hospital stays and underestimate shorter ones, as well as not allowing the establishment of causation relationships. However, this is a common limitation of all cross-sectional studies, which are far more operational and efficient as surveillance systems for potential AEs.
The influence of the reliability and accuracy of clinical records should also be considered, and the collection and interpretation of data have an inherent component of subjectivity that may affect results. A standardized, widely used, and recognized methodology was used to control these limitations [Citation44], to which a peer review of all positive screening was added.
Strengths
The standardization of the methodology is the study’s main strength since it ensures its reproducibility and comparability over time, this being a key element for periodic surveillance of possible incidents related to patient safety. However, another strength of our study was the analysis of factors associated with avoidable AEs. In this regard, it was observed that the records of patients in the ICU and the previous presence of pressure ulcers, central venous catheter, and impaired mobility were associated with the development of avoidable AEs, guiding us for the optimal management of immobilized patients, which is an area of improvement to reduce their impact.
In addition, this is one of the few studies that have collected information from negative screening, which has allowed us to explore the association between the presence of AEs and the patient’s death, enabling efficient identification of areas of improvement where a better impact on patient safety can be achieved. Finally, this work manages to identify areas for improvement in patient safety and its dissemination helps to promote the culture of safety, identified in previous works as a fundamental factor to achieve improvements [Citation45].
Future research direction
Future studies, with a longitudinal design, should delve into the contributing factors of avoidable AEs specifically in ICUs, something that would allow mitigating its direct impact on the patient and the health system.
Once the previous knowledge of the causes that produce avoidable AEs has increased, there will be necessary studies that propose and investigate targeted interventions in order to reduce their frequency. It would be interesting to consider whether strategies aimed at ICU patients could be beneficial for them.
Conclusions
The prevalence of AEs was consistent with that obtained in other hospitals of the same complexity in studies that applied a similar methodology. Patients with more serious comorbidities were most likely to suffer AEs, practically all of them requiring additional health care.
The AEs had a major impact on health care, showing an association with patient death during hospitalization; therefore, raising awareness of its importance is critical to achieving optimal quality of care.
Avoidable AEs are less severe. However, their high frequency has greater repercussions on the patient and healthcare system. For example, patients hospitalized in the ICU who have pressure ulcers, impaired mobility, or cardiovascular disease, or who require a central venous catheter are those most frequently affected by avoidable AEs; therefore, optimizing their management would be beneficial by reducing their impact on the patient and would represent savings for the healthcare system.
Author contributions
JMA-A, JLV-M, JV-G, DSJ-S and AP-H: Conception and design. DSJ-S, PM-N, JV-G, ESHMAD Director Group and external advisers: Acquisition of data. DSJ-S, JLV-M and JV-G: Analysis and interpretation of data. DSJ-S and JV-G: Drafting the manuscript. JLV-M, JMA-A, PM-N and AP-H: Critical revision of the manuscript for important intellectual content. JMA-A, JLV-M and AP-H: Supervision.
Supplemental Material
Download MS Word (15.9 KB)Acknowledgements
To ESHMAD Director Group and external advisers** for their participation in the acquisition of data.
**Asunción Colomer Rosas, Inmaculada Mediavilla Herrera, Ma José Esteban Niveiro, Nieves López Fresneña, Cristina Díaz-Agero Pérez, Pedro Ruiz Lopez, Isabel Carrasco Gonzalez, Cristina Navarro Royo, Carmen Albéniz Lizarraga, Yuri Fabiola Villan Villan, Ana Isabel Alguacil Pau, Alicia Díaz Redondo, Rosa Plá Mestre, Dolores Martín Ríos, Angels Figuerola Tejerina, Carlos Aibar Remón, José Joaquín Mira Solves, Juana Requena Puche, Idelfonso González Solana, Montserrat Salcero Guijarro, Delia Fernández Redondo, Esteban del Pozo García, Cornelia Bischofberger Valdés, Libertad Martín Prieto, Marta Grande Arnesto, Beatriz Nieto Pereda, Ana Herranz Alonso, Alicia Díaz Redondo, Laura Rubio Cirilo, Rafael Martos Martínez, María Teresa Ledo Varela, María Vicenta García Rosado, Jesús Minaya Saíz, María Jesús Labrador Domínguez, María José Pita López, Elia Mayoral Peccis, Marco Antonio Espinel Ruíz, Ana Polo Parada, Emely García Carrasco, Carlos Aranda Cosgaya, Carmen Gutiérrez Bezón, María de Sebastián Rueda, Miguel Ruíz Álvarez, Mercedes Vinuesa Sebastián, María Dolors Montserrat Capella, Carolina Ruíz Entrecanales, Sonia de Miguel Fernández, María Pilar González Sánchez, Felisa Jaén Herreros, María José Durá Jiménez, Carmen de Burgos Lunar, Anabel Alguacil Pau, María Ángel Valcárcel de la Iglesia, Laura Moratilla Monzó, Mercedes Ortiz Otero, Margarita Mosquera González, Susana Lorenzo Martínez, María Dolores Martín Ríos, Carolina Lucas Molina, María Teresa Sayalero Martín, María Dolores Calles Gato, Juan José Granizo Martínez, Juan Vega Barea, Eva Jiménez González de Buitrago, Inés Fernández Jiménez, Cristina García Fernández, Inmaculada López Carrillo, Ana Robustillo Rodela, Elena Ramírez García, Romina Sánchez Gómez, Nieves Franco Garrobo, Nieves Plana Farrá, Marta Macías Maroto, Marta Soler Vigil, Gonzalo de las Casas Cámara, Nuria Gálvez Carranza, Ana Belén Jiménez Muñoz, Belén Martínez Mondéjar, Beatriz Isidoro Fernández, Lourdes Sainz de los Terreros Soler, Carolina del Valle Giráldez García, Ruth González Ferrer, Guillermo Ordóñez León, Miguel Miró Murillo, Rosalía Hernández Holgado, Pilar Paloma Blanco Hernández, José Manuel Carrascosa Bernaldez, Sonia Fraile Gil, Beatriz Fidalgo Hermida, Francisco López Rodríguez Arias, Verónica Aranaz Ostáriz, María Pardo Ortiz, Raquel Arguedas Sanz. This work is inspired by the End of Master’s Work entitled "Frequency and Impact of Adverse Events in a Third-Level Hospital. ESHMAD Study", defended by Diego San José Saras on 28 October 2020. It can be found at: https://repisalud.isciii.es/bitstream/handle/20.500.12105/13467/FrecuenciaImpactoEventosAdversos_2020.pdf?sequence=1&isAllowed=y
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The data that support the findings of this study are available from the corresponding author, JVG, upon reasonable request.
References
- World Health Organization. Conceptual framework for the International Classification for Patient Safety. 2009. http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf.
- WHO. 10 Facts on Patient Safety Geneva [Internet]. 2017. http://www.who.int/features/factfiles/patient_safety/en/.
- Kruk ME, Gage AD, Joseph NT, et al. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. Lancet. 2018;392(10160):2203–2212.
- Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. 2016;353:i2139.
- Al-Mugheed K, Bayraktar N, Al-Bsheish M, et al. Patient safety attitudes among doctors and nurses: Associations with workload, adverse events, experience. Healthcare (Basel). 2022;10(4):631.
- Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the harvard medical practice study I. N Engl J Med. 1991;324(6):370–376.
- Walshe K. The reliability and validity of adverse-event measures of the quality of health care. 1998. 1–417.
- Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38(3):261–271.
- Wilson RM, Runciman WB, Gibberd RW, et al. The quality in Australian health care study. Med J Aust. 1995;163(9):458–471.
- Vincent C, Neale G, Woloshynowych M. Adverse events in british hospitals: preliminary retrospective record review. BMJ. 2001;322(7285):517–519.
- Baker GR, Norton PG, Flintoft V, et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678–1686.
- Aranaz-Andrés JM, Aibar-Remón C, Vitaller-Burillo J, ENEAS work group, et al. Impact and preventability of adverse events in spanish public hospitals: results of the spanish national study of adverse events (ENEAS). Int J Qual Health Care. 2009;21(6):408–414.
- Aranaz-Andrés JM, Aibar-Remón C, Limón-Ramírez R, IBEAS team, et al. Prevalence of adverse events in the hospitals of five latin American countries: results of the ‘iberoamerican study of adverse events’ (IBEAS). BMJ Qual Saf. 2011;20(12):1043–1051.
- Institute of Medicine (US) Committee on Quality of Health Care in America. To err is human: Building a safer health system. [Internet]. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US); 2000. [cited 2021 Mar 27]. http://www.ncbi.nlm.nih.gov/books/NBK225182/
- Donaldson L. An organisation with a memory. Clin Med (Lond). 2002;2(5):452–457.
- Building a safer NHS for patients: implementing an organisation with a memory. London: Great Britain Department of Health ; 2001. [cited 2022 February 16]. https://www.palliativedrugs.com/download/BuildingaSaferNHSforPatients.pdf.
- Martins M, Travassos C, Mendes W, et al. Hospital deaths and adverse events in Brazil. BMC Health Serv Res. 2011;11:223.
- Panagioti M, Khan K, Keers RN, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ. 2019;366:l4185.
- Chuang YT, Ginsburg L, Berta WB. Learning from preventable adverse events in health care organizations: development of a multilevel model of learning and propositions. Health Care Manage Rev. 2007;32(4):330–340.
- Rafter N, Hickey A, Condell S, et al. Adverse events in healthcare: learning from mistakes. QJM. 2015;108(4):273–277.
- Valencia-Martín JL, Martin-Delgado J, Pardo-Hernández A, et al. The study on safety in hospitals in the region of Madrid (ESHMAD) design: Screening and analysis of incidents and adverse events. J Healthc Qual Res. 2021;36(4):231–239.
- Valencia-Martín JL, Vicente-Guijarro J, San JoseSaras D, et al. Prevalence, characteristics, and impact of adverse events in 34 Madrid hospitals. The ESHMAD study. Eur J Clin Invest. 2022;e13851. doi: 10.1111/eci.13851
- Hiatt HH, Barnes BA, Brennan TA, et al. A study of medical injury and medical malpractice. N Engl J Med. 1989;321(7):480–484.
- Aranaz-Andrés JM, Aibar-Remón C, Vitaller-Murillo J, ENEAS work group, et al. Incidence of adverse events related to health care in Spain: results of the spanish national study of adverse events. J Epidemiol Community Health. 2008;62(12):1022–1029.
- Requena J, Aranaz JM, Gea MT, Grupo de Trabajo del Proyecto Estudio de Prevalencia de Identificación de Eventos Adversos, et al. [Evolution of the adverse effects prevalence related to healthcare in hospitals of the Valencia community]. Rev Calid Asist. 2010;25(5):244–249.
- Estudio de Prevalencia de Infecciones Nosocomiales. Informe España. 2019. Sociedad Española de Medicina Preventiva, Salud Pública e Higiene. [cited 2022 February 16]. https://epine.es/api/documento-publico/2019%20EPINE%20Informe%20Espa%C3%B1a%2027112019.pdf/reports-esp.
- Aranaz-Andrés JM, Aibar-Remón C, Vitaller-Murillo J, et al. Estudio nacional sobre los efectos adversos ligados a la hospitalización: ENEAS 2005. Madrid: Ministerio de Sanidad y Consumo; 2006.
- Aranaz-Ostáriz V, Gea-Velázquez De Castro MT, López-Rodríguez-Arias F, on behalf of the ESHMAD Director Group and External Advisers, et al. Surgery is in itself a risk factor for the patient. IJERPH. 2022;19(8):4761.
- Aranaz-Andrés JM, Limón R, Mira JJ, ENEAS Working Group, et al. What makes hospitalized patients more vulnerable and increases their risk of experiencing an adverse event? Int J Qual Health Care. 2011;23(6):705–712.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- StataCorp. 2019. Stata statistical software: Release 16. College Station (TX): StataCorp LLC.
- Michel P, Quenon JL, de Sarasqueta AM, et al. Comparison of three methods for estimating rates of adverse events and rates of preventable adverse events in acute care hospitals. BMJ. 2004;328(7433):199.
- Aranaz Andrés JM, Limón Ramírez R, Aibar Remón C, IBEAS Teamwork, et al. Comparison of two methods to estimate adverse events in the IBEAS study (Ibero-American study of adverse events): cross-sectional versus retrospective cohort design. BMJ Open. 2017;7(10):e016546.
- Larsen GY, Donaldson AE, Parker HB, et al. Preventable harm occurring to critically ill children. Pediatr Crit Care Med. 2007;8(4):331–336.
- Schwendimann R, Blatter C, Dhaini S, et al. The occurrence, types, consequences and preventability of in-hospital adverse events - a scoping review. BMC Health Serv Res. 2018;18(1):521.
- Requena J, Miralles JJ, Mollar J, et al. [Clinical safety paediatric patients]. Rev Calid Asist. 2011;26(6):353–358.
- Sousa P, Uva AS, Serranheira F, et al. Patient and hospital characteristics that influence incidence of adverse events in acute public hospitals in Portugal: a retrospective cohort study. Int J Qual Health Care. 2018;30(2):132–137.
- Tartaglia R, Albolino S, Bellandi T, et al. [Adverse events and preventable consequences: retrospective study in five large italian hospitals]. Epidemiol Prev. 2012;36(3-4):151–161.
- Sousa P, Uva AS, Serranheira F, et al. Estimating the incidence of adverse events in portuguese hospitals: a contribution to improving quality and patient safety. BMC Health Serv Res. 2014;14:311.
- Lessing C, Schmitz A, Albers B, et al. Impact of sample size on variation of adverse events and preventable adverse events: systematic review on epidemiology and contributing factors. Qual Saf Health Care. 2010;19(6):e24–e24.
- D'Amour D, Dubois C-A, Tchouaket E, et al. The occurrence of adverse events potentially attributable to nursing care in medical units: cross sectional record review. Int J Nurs Stud. 2014;51(6):882–891.
- Corrales-Fernández MJ, Gea-Velázquez de Castro MT, Limón-Ramírez R, et al. [Factors that contribute to health care associated infections: how to prevent them]. Rev Calid Asist. 2011;26(6):367–375.
- Ministerio de Sanidad. Portal Estadístico del SNS - Información estadística de hospitales: Estadística de Establecimientos Sanitarios con Régimen de Internado [Internet]. [cited 2022. February 16]. https://www.sanidad.gob.es/estadEstudios/estadisticas/estHospiInternado/inforAnual/homeESCRI.htm.
- Woloshynowych M, Neale G, Vincent C. Case record review of adverse events: a new approach. Qual Saf Health Care. 2003;12(6):411–415.
- Al-Mugheed K, Bayraktar N. Patient safety attitudes among critical care nurses: a case study in North Cyprus. Int J Health Plann Manage. 2020;35(4):910–921.