Abstract
Objective
This study examines the impact of the COVID-19 pandemic on cochlear implantation (CI) recipients in Saudi Arabia. The impact was measured using the results of an online survey that investigated challenges related to access to re/habilitation and programming services, increased dependence on virtual interaction, and emotional impact.
Methods
The cross-sectional online survey reached 353 pediatric and adult CI recipients between April 21st and May 3rd 2020, during the first weeks of implementing the lockdown strategy and the transitioning to virtual settings.
Results
It was revealed that overall access to aural re/habilitation was considerably affected during the pandemic, and that the impact of this disruption was significantly greater for pediatric recipients than for adults. On the other hand, overall access to programming services was not affected. Results also revealed that CI recipients' performance at school or work was negatively impacted by the transition to a virtual communication. In addition, participants noticed a decline in their auditory performance, language skills, and speech understanding. They also registered feelings of anxiety, social isolation, and fear related to sudden changes in their CI function. Finally, the study revealed a gap between CI clinical/non-clinical support provided during the pandemic and the expectations of CI recipients.
Conclusion
Collectively, outcomes from this study highlight the importance of shifting towards a more patient -centered model that offers empowerment and self-advocacy. In addition, the outcomes also emphasize the importance of developing and adapting emergency protocols. This will ensure continuation of services provided to CI recipients during scenario disasters like a pandemic.
Pediatric aural re/habilitation was subjected to a significantly greater interruption, compared to adult aural re/habilitation, duringthe COVID-19 shutdown.
Cochlear Implant (CI) recipients expressed feelings of anxiety, social isolation, and fear. These feelings were related to sudden changes in their CI functioning, caused by interruption of support services during the pandemic.
Patient -centered model can offer emergency protocols that ensure a smooth continuation of cochlear implant-related re/habilitation and services during disaster scenarios such as the COVID-19 pandemic.
Key messages
Introduction
Over 1.5 billion people experience some form of hearing impairment worldwide [Citation1]. For those whose hearing loss cannot be adequately addressed through acoustic amplification alone, cochlear implantat (CI) is a viable option [Citation2]. In Saudi Arabia, the numbers of CI programmes have surged nationwide thanks to their high efficiency and effectiveness [Citation3]. Now, there are about 25 government-supported CI programmes: eight in the Central region, five in the Eastern region, four in the Western region, five in the Southern region, and three in the Northern region. Collectively, these public health sector programmes performed approximately 1000 CI surgical operations in 2018/2019Footnote1, with an estimated annual growth rate of 15% and success rate of around 97.5% [Citation3,Citation4], which is consistence with CI manufacturers’ reliability reports [Citation5,Citation6]. Alongside CI surgeries, these CI programmes also provide essential services for CI recipients, that are delivered by multi-disciplinary teams including, but not limited to: audiologists, otolaryngologists, speech-language pathologists (SLP), psychologists, social workers, and programme coordinators. In addition, CI devices, consumables, and costs of repair to external items are all covered under the national public health plan. Furthermore, the CI programme teams work closely with CI local distributors to maintain appropriate access to all external items needed by CI recipients.
The majority of CI recipients in Saudi Arabia are pediatrics (over 65%, 18 years and younger), whereas adults (around 30%, over 18 years) constitute a smaller fraction of the total number of people with CI implantsFootnote2. Following successful implantation, CI recipients will requireaural re/habilitation and support services for the rest of their lives, with age-appropriate re/habilitation being a major factor in successful CI outcomes [Citation7]. While the level of re/habilitation and support needed by a CI recipient is dependent on several factors, the most critical and demanding stage for all recipients is the period immediately after implantation. Therefore, during the first two post-implantation years, all CI recipients receive an intensive re/habilitation programme. This involves attending at least two or three aural rehabilitation sessions a week with an SLP. Additionally, the recipient is expected to have regular visits with the audiologist for device programming, these visits are then reduced over time as applicable. Any interruption to the programme will limit the benefits of the CI, particularly for those within the critical age of language acquisition, i.e., ages birth to 5 years.
Immediately after COVID-19 was declared a pandemic on the 11th of March 2020 [Citation8], regulatory bodies in Saudi Arabia took several precautionary measures to contain the spread of the disease. These measures commenced on the 9th and 15th of March, when schools and workplaces closed and were replaced by, where possible, online learning and working from home. For the former, all children and pupils from pre-school age to college level were directed to attend classes through virtual learning hubs. For the latter, workplace attendance was severely restricted in both public and private sectors, with remote-working enforced where possible and with face-to-face meetings replaced with meetings via virtual communication platforms. On the 23rd of March a night-time curfew was imposed, followed by travelling restrictions between cities, which in turn was followed by a total lockdown during the Eid holydays in July [Citation9].
Besides the inconvenience of having to adjust to this new isolation lifestyle, the majority of the population quickly adapted to these measures with no significant issues. However, those with special needs, including those with hearing impairments, were faced with considerable obstacles. Certainly, the transition from in-person to virtual communication with others at school, work, or at social events introduced new challenges to the hearing-impaired community. Specifically, people with a CI had to actively adapt to this new method of communication. One major challenge stemmed from the fact that sound transmitters such as headphones used in virtual communication could alter/omit some of the speech signals. Therefore, individuals who use a CI understand less when listening to recorded speech than when hearing live speech [Citation10]. This is all in addition to the loss of visual cues that are crucial for speech understanding, especially when listening without real-time captioning [Citation11]. Individuals with hearing loss, even those with CI, still need visual cues and non-verbal information to fully understand speech, but these are often absent when communicating virtually [Citation12].
Aside from issues surrounding virtual communication platforms, face-to-face meetings during the pandemic also proved very difficult for the hearing impaired and CI recipients – mainly because of face masks. Face masks not only create a visual barrier by obscuring parts of the face that would have provided visual cues, but they are known to alter sound characteristics. Depending on the type of material, face masks can attenuate the sound pressure level (SPL) of the speech signal by up to 29.2 dB, specifically at frequencies of 3000 Hz and higher [Citation13,Citation14]. These visual and acoustic challenges are also exacerbated when social distancing rules require people to stand two metres or more apart. Trecca et al. [Citation15] has investigated this issue and preliminary data revealed that over 85% of individuals with hearing loss faced difficulties with acoustic transmission when facemasks are used during the pandemic.
All these pandemic-related communication barriers can render everyday tasks prohibitively challenging for the hard of hearing [Citation16,Citation17] and can cause profound psychological and emotional stress to CI recipients and their families [Citation18].
In addition to these obstacles, CI recipients also faced disruption to their re/habilitative and programming services, as well as disruption in their communications with their healthcare providers, which often projected to cause adverse clinical side effects [Citation19]. A survey study where children with CI had difficulties attending aural rehabilitations, hardwear services, and intermittency in sound access reported that that this interruption have led to behavioral changes [Citation20]. The same outcome was also reported by Sahoo et al. [Citation21], were parents reported that the pandemic impacted their children’s psychological status and caused behavioral changes.
Therefore, the aim of this study was to investigate the impact of COVID-19 pandemic-related implications on both pediatric and adult CI recipients in Saudi Arabia. The parameters evaluated availability and access to aural rehabilitative and programming services, ease of communication with CI programme staff, and overall provision of support. In addition, this study examines CI recipients’ experience with virtual school/work settings, and how these changes affect their auditory and language performance abilities as well as their mental/emotional wellbeing.
Study design
Survey construction
A cross-sectional online survey was created in the Arabic language using Google Doc forms. Prior to distribution, the survey underwent revision and proofreading. It was then completed by three independent test respondents in order to obtain important feedback regarding the level of difficulty and time it takes for the target population (guardians for pediatrics and self-completion for adults) to complete. The survey was divided into 11 sections: the first nine featured multiple-choice questions (in some more than one answer could be selected), and the last two sections contained scale-rating questions. The respondents were able to return to previous sections and change answers prior to submission.
Survey sections covered the following: demographic information (1), CI background information (2), healthcare accessibility and health communication before and after the pandemic (3), aural rehabilitation and programming services prior to the pandemic (4), aural rehabilitation and programming services during the pandemic (5), challenges during the pandemic (6), adaptation of CI recipients during the pandemic (7), clinical and non-clinical organization support during COVID-19 pandemic (8), virtual school/workplace communication (9), CI management and intervention in emergencies (10), digital solutions to improve healthcare services and quality of care (11).
Distribution and study sample
The survey was distributed between the 21st of April and the 3rd of May 2020, during the first weeks of lockdown and the transition to virtual school and work platforms in Saudi Arabia. Convenience sampling was used to recruit survey participants from all regions of Saudi Arabia. To reach as many targeted individuals as possible, CI associations and support groups were recruited to distribute the link. The Survey link was then sent to participants via digital platforms including Twitter and instant messaging applications.
Of the 424 responses to the online survey, 353 (n = 326 pediatrics and n = 27 adults) were used in this study. Individuals who answered the control question wrong were excluded (71 in total: 51 pediatrics and 20 adults). For the pediatric survey, 197 were completed by fathers, 140 by mothers, and 5 by other family members. All adult participants completed the survey themselves.
Statistical analysis
Statistical analyses were carried out using (SAS Institute Inc. Cary, 2013) [Citation22]. Descriptive analyses were initially performed to provide information of sample data and visual/practical relevance. To assess the test of independence and correlation, a chi-square correlation test of independence was completed. Where the chi-square test could not be used due to the sample size or distribution concerns, Fisher’s exact test was carried out instead. Statistical significance used in this study was 5%, which was determined as P value. Also, missing values in the data were treated as missing completely at random (MCAR). Rating scales were converted from a scale of five to three in all sections for an easier analysis and view of the results.
Results
Availability and access to aural rehabilitation, programming, hardware and support services during the COVID-19 pandemic
Two major external factors were considered in the analysis: transportation challenges related to pandemic travel restrictions and economical implications of the lockdown. 50% of pediatric and 30% of adult participants reside in the same city where the speech and language rehabilitation services are located. Moreover, a higher number (around 60%) of pediatric and adult participants reside in the same city where the programming services are located (further socioeconomic and CI background information for all participants is shown in the appendix, and ). Over 60% of participants reported easy physical access to both rehabilitation and programming services prior to pandemic-related travel restrictions. During the pandemic, travel difficulties and the distance between services and the recipients’ homes were not reported as a major issue.
Table 1. Demographic information of pediatric and adult participants; N = 353.
Table 2. Cochlear implant history and background information for pediatric and adult recipients; N = 353.
Furthermore, around 90% of participants in this study are receiving services for CI surgery and aural rehabilitation (i.e., speech and language therapy and device programming services) in government-run hospitals and government-affiliated centres. The majority of participants are Saudi nationals who are eligible for CI surgery and subsequent rehabilitation care under the free-of-charge national health services. Therefore, any economic implications brought on by the pandemic are not likely to affect how CI recipients access rehabilitation or support services during the pandemic. As a result, questions related to healthcare insurance or changes to the income of participants were not significant to this study.
Access to aural rehabilitation services
Regarding SLP-led aural re/habilitation services, both pediatric and adult participants were asked about the number of scheduled sessions and the number of attended sessions before and during the pandemic (). The results showed that pediatrics were the most affected in this area (for detailed subgroup analysis, refer to ). For them, there was a significant drop in the number of scheduled rehabilitation sessions during the pandemic compared with pre-pandemic (). There was also an overall decline in the number of scheduled sessions for adults during the pandemic, but statistical analyses did not reveal the decrease to be significant (), (for detailed subgroup analysis, refer to ).
Figure 1. (a) Scheduled/attended aural re/habilitation sessions before and during COVID-19 pandemic in paediatrics. *p < 0.001, a correlation test was completed for each subgroup separately for scheduled and attended sessions. Subcategories were categorized as follows: intensive aural re/habilitation (i.e., 1–3 ≥ sessions per week), moderately intensive aural re/habilitation (i.e., 1–2 sessions per month), non-intensive aural re/habilitation (i.e., 1 session per 3–6 months). (b) Scheduled/attended aural re/habilitation sessions before and during COVID-19 pandemic in adults. A correlation test was completed for each subgroup separately for scheduled and attended sessions. Subcategories were categorized as follows: intensive aural re/habilitation (i.e., 1–3 ≥ sessions per week), moderately intensive aural re/habilitation (i.e., 1–2 sessions per month), and non-intensive aural re/habilitation (i.e., 1 session per 3–6 months).
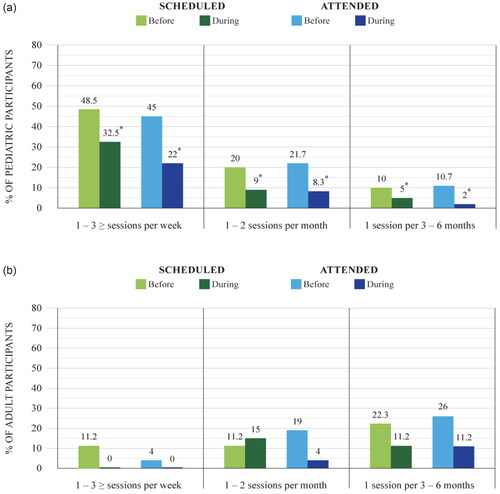
Table 3. Correlation test P value results for tested parameters for N = 353 (Pediatrics: n = 326 and Adults: n = 27).
As for the number of attended sessions, in general, participants who were more committed to attending their scheduled sessions pre-pandemic recorded a better attendance record during the pandemic. Again, pediatrics were more affected than the adults as they significantly missed more sessions during the pandemic compared with the number of missed sessions pre-pandemic (for detailed subgroup analysis, refer to ). Parent survey respondents expressed that the main reason behind missing sessions during the pandemic was the fear of COVID-19 exposure. For adults, statistics comparing pre-pandemic and pandemic attendance patterns showed no significant change, despite an observed overall decrease (for detailed subgroup analysis, refer to ). However, those adults who did miss their aural re/habilitation sessions also reported the fear of COVID-19 exposure as the main reason. In both groups, the rate of attendance for aural re/habilitation sessions and area of residency did not show a significant correlation.
During the period in which the study survey was distributed, a 24-hour lockdown was imposed for the Eid national holidays. During which, Participants attempted to contact the CI Programme via different methods (). When they were asked if they had emergency access to members of their rehabilitation team during the six days of total lockdown, the survey indicated that pediatrics were overall more affected by restricted communication with their CI team than the adults. Parents of pediatric recipients also reported difficulties reaching out to all members of the team. In terms of which member was reached out to, pediatric survey participants reported that the most reachable CI team members during lockdown were the audiologist and the CI Programme coordinator; the adult group cited audiologists as the easiest to reach.
Figure 2. Methods of contacting CI program members in emergencies during COVID-19 pandemic. *Includes scheduled, walk-in, emergency room visits. ** Includes audiologists, and CI program coordinator.
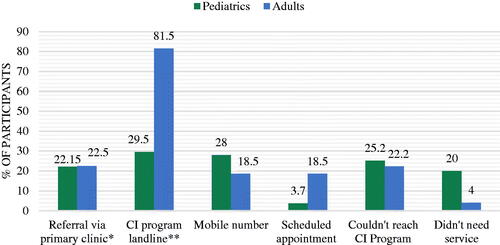
Finally, participants were asked to rate the overall support received by the CI team during the pandemic. The majority of the pediatric group reported a low satisfaction rate, while most of the adults reported that they were moderately satisfied. When asked which member of the rehabilitation team they felt was most needed during the pandemic, the pediatric group selected their SLP, while the adult group selected their audiologist.
Access to programming and hardware services
For on-site programming services, there was no significant change in availability and access before and during the pandemic, according to the pediatric and adult survey results (). During the survey period, 7% of CI pediatric recipients received remote programming services through a local CI distributer office visit in their residential area, mostly outside the city where the programming office is located. Participants who received remote programming were able to do so successfully via conferencing software at their local CI distributor office. There, a facilitator connected their device to a pod so that the primary audiologist could gain full access to the implant.
For CI internal device emergency services, only 18% in each group required an immediate intervention for issues related to their implanted device. Participants reported swelling, redness, and infection in the implant area as the major issues. Both groups reported that they received adequate urgent care by the CI team regardless of their residential location ().
On the other hand, of pediatric and adult participants, 32.21%; 40.74% reported that they experienced malfunctioning or loss of external CI hardware. For pediatric CI recipients, the hours of device usage significantly influenced the rate of malfunction of external items (). The external items susceptible to damage, starting with the most prone, were: microphone filters, drying kits, connecting cables, and the rechargeable battery. However, most of the participants reported that they had spare parts at home, while the rest were able to source replacements for the damaged items from elsewhere.
It is worth mentioning that there was no significant correlation in service accessibility at CI local distributer offices before and during the pandemic (). When participants were asked to rate the support provided by local CI distributors during the pandemic, the majority of both groups reported a low level of support. Furthermore, a low satisfaction rating was seen across all local distributer offices of all the brands of CI, with no particular brand scoring significantly higher or lower compared with the others ().
Home, school and work performance during the COVID-19 pandemic
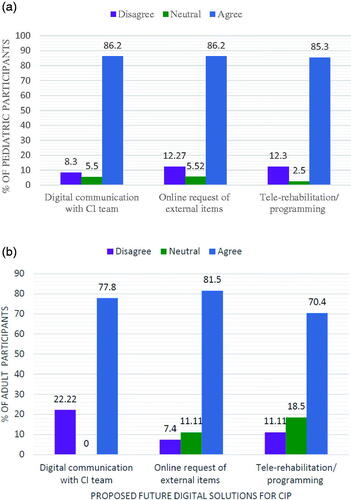
The survey’s results show that during the pandemic, only 20% of pediatric and 7% of adult CI recipients received a home-based aural re/habilitation training kit from their SLP. Most of the recipients who did not receive the training kit, self-initiated home training by utilizing internet-based platforms and social media (). For both groups, there was a significant correlation between parental and self-qualifications and the utilization of digital platforms for training materials (). Regarding rehabilitation results, parents reported no noticeable improvement in the language skills of their children with home-based training (). Nevertheless, CI participants and their families exhibited readiness to integrate digital solutions into their health care services ().
Figure 3. Sources of aural re/habilitation material during COVID-19 pandemic. *By primary SLP. **Includes Google search, social media, aural rehabilitation mobile applications.
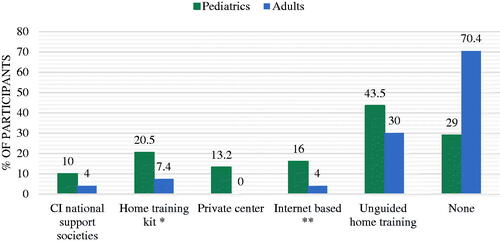
Figure 4. (a) Agreement to proposed future digital solutions for CI program in pediatrics. (b) Agreement to proposed future digital solutions for CI program in adults.
Attending school and work prior and during the pandemic was investigated. Fifty three% of participants (Pediatric and adults) attended educational facilities prior to the pandemic. This number dropped to 35% during the pandemic, when virtual attendance was required. Whereas 60% of adult participants were employed and attended work. This number dropped to 48%, when virtual attendance was enforced during the pandemic (refer to for details).
Most participants, around 80%, reported hearing difficulties while using a virtual setting, which consequently affected their performance at school/work. Yet, disclosure of hearing difficulties to teacher/employer, utilization of assistive listening devices (ALDs), and implementation of communication strategies while using the virtual platforms were rated very low in both groups. Regarding ALD utilization, even though 45% and 70% of pediatrics and adults, respectively, owned at least one ALD (refer to for details), only one third received training on how to use them.
Similarly, participants in both groups rated school/employer support to be either non-existent or low. In addition, results show a significant correlation between reporting low school/work support and self-assessed hearing difficulties (). The national CI associations were rated slightly higher in support compared with other sectors.
Subjective changes in CI recipients’ daily living during the pandemic
Participants were asked to self-assess the challenges they faced. In terms of auditory performance, the majority of participants from both groups reported severe deterioration. There was a significant correlation between the length of time since a participant underwent CI surgery and the magnitude of the deterioration (). Those who were implanted just before the pandemic faced more hearing difficulties compared with participants who were implanted earlier and passed the critical stage. As for self-assessed deterioration in language skills, only a few of the pediatric recipients’ parents and almost none of the adults reported any deterioration. Self-assessed deterioration in speech understanding – reported by adults only – was described as either moderate or severe by 45% of participants.
Participants were also asked if they felt that face masks affected their face-to-face communication and understanding of verbal communication. Most parents did not think that face masks had an effect on their children’s communication, while most of the adult participants reported face masks did impact their communication abilities.
When answering questions regarding feeling anxious and socially isolated, one quarter of the pediatrics group and one third of the adults group reported having experienced severe anxiety and fear of sudden changes in the function of their CI during the pandemic. These feelings were not influenced by the length of the time passed since the device was implanted (). Extreme feelings of social isolation were also experienced by around 20% of participants in both groups. While data analysis for both groups showed no obvious link between feeling socially isolated and noticing changes in auditory performance (), there was a significant correlation in the pediatrics group between feeling socially isolated and having other health comorbidities (). Finally, when asked if they believed the emotional impact of the pandemic was greater for a person with hearing loss compared with someone with normal hearing, 30% of pediatrics and over 50% of adults strongly agreed to this statement.
Discussion
The aim of this study was to examine the impact of the COVID-19 pandemic on CI recipients in Saudi Arabia. More than 350 CI pediatric and adult recipients participated in an online survey. Survey questions addressed aural rehabilitation progression, programming services offered, and availability of hardware maintenance. In addition, participants were surveyed on their experience with changes in communication patterns and support offered to them by their clinical and non-clinical institutions. The study was conducted shortly after COVID-19 was declared as a global pandemic by the World Health Organization.
Participants completed the survey during the two months where the preventive measures were at their highest. Therefore, the impact of the pandemic on participants, including restricted travel and emotional stress, was expected to have been captured at its most severe. Also, the disturbance to the workflow of CI rehabilitation and support teams—was also expected to have been captured at its highest. Physical visits to CI re/habilitation locations (mostly hospitals) were limited to high-risk cases only; for others, care was provided through phone-based medical screenings to address concerns, function, and performance evaluation. In addition, local distributors of CI and other affiliated entities/offices also closed and relied on phone customer service.
Analysis of survey answers revealed that pediatric CI re/habilitation progression was more vulnerable to pandemic-related implications. This has been shown by the drop in scheduled and attended re/habilitation sessions in the pediatric group. Regarding the scheduling of appointments, a possible cause of the sharp drop could be due to prioritization requirements. The majority of CI recipients are prelingual children, of which around 10% are in an intensive stage of an aural rehabilitation programme. For this group, it is crucial to undergo a minimum of two to three sessions per week as they are in a time-sensitive stage of their rehabilitation. Therefore, it was expected that the aural re/habilitation team prioritize CI pediatric recipients undergoing intensive therapy during pandemic restrictions, thus significantly affecting the appointments available for CI pediatric recipients with non-urgent needs. Therefore, limited clinical capacity mandated that only high-risk patients, or those with urgent medical priorities, are seen in person.
Regarding the adults, the overall number of adult recipients is small in comparison. This resulted in no appointment disturbance or shifting of prioritization, and subsequently there were no significant changes to their scheduling pattern. As for appointment attendance, again pediatric were more likely to miss their appointments during the pandemic mainly due to fair of COVID-19 exposure, which is consistent with a previous study from Germany [Citation23]. On the other hand, programming services were not affected, according to the responses given by the participants in both groups. This could be attributed to 90% of participants being implanted for more than a year and had thus reached a stable programming that, in turn, lessened the frequency of required visits [Citation2,Citation24]. It could also be attributed to that fact that a small portion of participants received remote programming services via a remote programming system. In remote programming, participants still had to travel to a local CI distributor office to receive the service, but remote programming outside a hospital setting was expected to at least minimize the fear of disease exposure. This reaffirms that, a wider implementation of tele-practice in aural rehabilitation and programming is critical to prevent any future interruption of CI services during challenging circumstances [Citation25,Citation26]. In general, it is projected that the digitalization of health services will prove to be a practical future approach for an efficient and cost-effective healthcare system [Citation27].
As for language skills in pediatrics, home-based aural re/habilitation training kits were only received by a small number of CI recipients. The majority relied on digital platforms to obtain aural re/habilitation training material with no reported improvement in speech and language skills. This could be a result of not knowing where to get/how to perform effective home-training without directions from their SLP. Therefore, not only it is crucial to provide all CI recipients with home-training kits, but it is also vital to create digital training materials that meet the needs of the targeted population – i.e., platforms in the Arabic language – and educate CI recipients on how to choose the ones that best fit their needs.
Participants also reported feelings of anxiety and fear of sudden changes in the function of their CI. Introducing a patient-centred care model in CI programmes – by empowering CI recipients by teaching them to take control of their CI journey – will lead to better performance outcomes [Citation28]. It will also eliminate feelings of fear, anxiety, and frustration that can result from not knowing what to do in case of interrupted contact with the CI team [Citation29]. The decentralization of care and resources offered to patients is thought to improve clinical outcomes, assuming that it will not diminish communication with health care providers [Citation19].
Another important aspect of a patient-centred care model is self-advocacy. Participants reported having hearing difficulties during virtual school/work meetings with no real-time captioning, yet they did not inform their teacher/employer that this was the case. Furthermore, despite the fact that a large number of participants owned ALDs, only a small number have been trained in how to use them and thus only a few can utilize them in virtual communications. Therefore, self-advocacy in addition to the proper utilization of ALDs, and the implementation of communication strategies must be enhanced amongst CI recipients.
In addition, health care professionals and CI recipients should receive training on the different forms of emergency support that might be available, and how to provide/receive them. Again, the digitalization of health care services is expected to allow for a higher level of support during disaster scenarios, compared with traditional provision [Citation30].
Finally, further research should be conducted to break down the classification of CI recipients even further. This will aid in understanding the diverse needs and consequently help to build a better, all-inclusive support system. Moreover, since the national CI societies and support groups were rated the highest in support provision during the pandemic, future investigative studies to examine benefits and initiate collaborative support approaches are recommended.
Clinical implications
Build a proper infrastructure for the successful integration of tele-rehabilitative approaches.
Digitize re/habilitation programmes and create tele-applications in Arabic language to implement a patient-centred care model in Saudi CI programmes.
Implement communication strategies and special programming protocols for hearing aids/implantable devices in order to enhance affected frequency ranges in virtual platforms.
Invest in educational audiologists in all school systems in Saudi Arabia to ensure that the environment, and assistive technology equipment in virtual platforms are properly used for students with hearing impairment.
Adapt a patient-centred care model in CI programmes by empowering CI recipients to manage and troubleshoot their devices.
Limitations
This study provides a large sample size and a high number of examined variables. Yet, findings of this study could not be compared with other findings in Saudi Arabia due to the lack of existing national research in this area. It could be seen as a limitation that the adult sample is much smaller than the pediatric sample; however, this reflects the ratio of adult to pediatric CI recipients in Saudi Arabia.
Conclusion
Collective findings of this study emphasize the benefits of integrating tele-practice and digital platforms in cochlear implant services. Further studies to assess models of digitalization in health care for CI recipients in their native language are still required prior to implementation. In addition, integrating a patient-centered care model in CI services will prove to be extremely beneficial for CI recipients. Such an approach will not only achieve better performance outcomes but help to reduce negative feelings regarding personal wellbeing. Similarly, incorporating empowerment and self-advocacy into the rehabilitation of CI recipients will reduce fear and anxiety by making recipients feel more in control as they become independent and less reliant on professional support in their daily lives.
Ethical approval
This study was approved by the Institutional Review Board at King Abdullah International Medical Research Center (KAIMRC), King Saud Bin Abdulaziz University for Health Sciences. Prior to the commencement of the survey, an electronic informed consent was obtained for all participants (a guardian for minors and self for adults), as it is mandatory to click on consent button in order to access the survey questions.
Author contributions
Conception and design: R. Alkhalil. Development of methodology: R. Alkhalil. Data collection: R. Alkahlil. Data analysis and interpretation: R. Alkhalil, B. Al-Sowayan, B. Albdah. Manuscript writing: R. Alkhalil, B. Al-Sowayan. All Authors reviewed and approved the final draft.
Acknowledgments
We would like to express our gratitude to all CI recipients and their families for their participation in this survey. We would also like to acknowledge CI local distributer offices for their role in distributing the survey. Finally, we thank Sharaf studio for revising and proof-reading the survey.
Disclosure statement
No potential competing interest was reported by the authors.
Data availability statement
The data that support the findings of this study are available from the corresponding author, RA, upon reasonable request.
Additional information
Funding
Notes
1 These are estimated numbers based on combined information from25 large national CI programs, CI local suppliers, and CI companies annual reports. National database is not available yet.
2 These are estimated numbers based on combined information from 25large national CI programs and CI local suppliers. National database is not available yet.
References
- World Health Organization. 2021. World report on hearing.
- Messersmith JJ, Entwisle L, Warren S, et al. Clinical practice guidelines: cochlear implants. J Am Acad Audiol. 2019;30(10):827–844.
- Alzahrani MA, Aldajani NF, Alghamdi SA. Guidelines for cochlear implantation in Saudi Arabia. Saudi Med J. 2021;42(12):1265–1271.
- Garrada M, Alsulami MK, Almutairi SN, et al. Cochlear implant complications in children and adults: retrospective analysis of 148 cases. Cureus. 2021;13(12):e20750.
- Cochlear Ltd. Cochlear TM Nucleus ® System Reliability Report Solidea, Cochlear Nucleus System recipient Cochlear Ltd. Cochlear Nucleus System Reliability Report, Volume 20. 2021.
- Medel, EL, MED-EL Cochlear Implant Systems. https://www.medel.com/hearing-solutions/cochlear-implants/reliability, 2022.
- Moran M, Vandali A, Briggs R, et al. Speech perception outcomes for adult cochlear implant recipients using a lateral wall or perimodiolar array. Otol Neurotol. 2019;40(5):608–616.
- World Health Organization. 2020. Public health emergency of international concern declared. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
- The Official Saudi Press Agency. 2020. COVID-19. https://www.spa.gov.sa/listnews.php?lang=en&cat=9#page=25
- Uhler K, Biever Y, Gifford H. 2016. Method of speech stimulus presentation impacts pediatric speech recognition monitored live voice versus recorded speech. Otol Neurotol. 37(2):e70–e74. http://journals.lww.com/otology-neurotology
- Krijger S, Coene M, Govaerts PJ, et al. Listening difficulties of children with cochlear implants in mainstream secondary education. Ear and Hearing. 2020;41(5):1172–1186.
- Most T, Aviner C. Auditory, visual, and Auditory-Visual perception of emotions by individuals with cochlear implants, hearing aids, and normal hearing. J Deaf Stud Deaf Educ. 2009;14(4):449–464.
- Magee M, Lewis C, Noffs G, et al. Effects of face masks on acoustic analysis and speech perception: implications for peri-pandemic protocols. J Acoust Soc Am. 2020;148(6):3562–3568.
- Atcherson SR. I can hear and see what you’re saying. Hearing Health Magaz. 2020;36(1):24–25.
- Trecca EMC, Gelardi M, Cassano M. COVID-19 AND hearing difficulties. Am J Otolaryngol. 2020;41(4):102496.10.1016/j.amjoto.2020.102496. PMC: 32327217
- Chodosh J, Weinstein BE, Blustein J. 2020. Face masks can be devastating for people with hearing loss. BMJ. 370:m2683. BMJ Publishing Group.
- Wolfe J, Morais M, Schafer E. Improving hearing performance for cochlear implant recipients with use of a digital, wireless, Remote-Microphone, Audio-Streaming accessory. J Am Acad Audiol. 2015;26(06):532–539.
- Ornell F, Schuch JB, Sordi AO, et al. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020;42(3):232–235.
- Ruben BD. Communication theory and health communication practice: the more things change, the more they stay the Same1. Health Commun. 2016;31(1):1–11.
- Ayas M, Ali Al Amadi AMH, Khaled D, et al. Impact of COVID-19 on the access to hearing health care services for children with cochlear implants: a survey of parents. F1000Research. 2020;9:690.
- Sahoo L, Kumar A, Patnaik U, et al. 2020. Cochlear implant rehabilitation during covid-19 pandemic: a parents’ perspective.
- SAS Institute Inc. Cary, N. S. I. I. (2013). SAS, S. (2013). 9.4 SAS Institute Inc. Cary, NC: SAS Institute Inc. (9.4).
- Aschendorff A, Arndt S, Kröger S, et al. Quality of cochlear implant rehabilitation under COVID-19 conditions. HNO. 2021;69(Suppl 1):1–6.
- Hemmingson C, Messersmith JJ. Cochlear implant practice patterns: the U.S. Trends with pediatric patients. J Am Acad Audiol. 2018;29(8):722–733.
- Luryi AL, Tower JI, Preston J, et al. Cochlear implant mapping through Telemedicine - A feasibility study. Otol Neurotol. 2020;41(3):e330–e333.
- Slager HK, Jensen J, Kozlowski K, et al. Remote programming of cochlear implants. Otol Neurotol. 2019;40(3):e260–e266.
- Herrmann M, Boehme P, Mondritzki T, et al. Digital transformation and disruption of the health care sector: internet-based observational study. J Med Internet Res. 2018;20(3):e104.
- Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Affairs. 2013;32(2):207–214.
- Helen Cullington. Cochlear implant care: putting patients in charge. National Cochlear Implant Users Association Newsletter. 2017.
- Robinson JD, Turner JW, Levine B, et al. Expanding the walls of the health care encounter: support and outcomes for patients online. Health Commun. 2011;26(2):125–134.
