Abstract
Background
Decrease in estimated glomerular filtration rate (eGFR) during Tenofovir disoproxil fumarate (TDF) treatment remains a concern, and few patients experience partial recovery of eGFR. This study aimed to investigate the risk factors for eGFR recovery in patients with and without hypertriglyceridemia.
Methods
A total of 203 patients with chronic HBV infection were prospectively recruited and followed up for three years. Data were collected at baseline, first, second, and third years during TDF treatment.
Results
Most patients achieved normal ALT (80.0% vs. 82.5%) and undetectable HBV DNA (95.0% vs. 95.6%) in both groups (p > 0.05). For patients with hypertriglyceridemia, eGFR and cholesterol did not change significantly during the 3-year follow-up, while triglyceride (TG) decreased significantly in the first year and persisted at a lower level in the subsequent two years. For patients without hypertriglyceridemia, eGFR declined significantly in the first year of treatment, then gradually recovered during the subsequent two years, and eGFR was negatively correlated with TG at the four time points. Fifteen (15/183, 8.2%) patients without hypertriglyceridemia experienced eGFR partial recovery in the third year. Univariate and multivariate analyses showed that baseline eGFR <90 mL/(min·1.73 m2) (p < 0.01; 95% CI: 0.019–0.284) and age (p < 0.01; 95% CI: 0.817–0.960) were independent risk factors for eGFR recovery.
Conclusion
eGFR partially recovered in patients without hypertriglyceridemia during TDF treatment, and TG regulation might be a useful strategy to hinder renal function decline, although larger, confirmatory studies are necessary to validate our findings.
For patients with normal triglyceride, eGFR declined significantly at the first year of TDF treatment, then gradually recovered during the subsequent two years, and eGFR was negatively correlated with TG. Baseline eGFR <90 mL/(min·1.73 m2) and age were independent risk factors for eGFR recovery.
Key messages
Introduction
Chronic hepatitis B virus (HBV) infection remains the leading cause of liver cirrhosis (LC) and hepatocellular carcinoma (HCC) in the Asia-Pacific region [Citation1,Citation2]. At present, nucleos(t)ide analogs (NAs) are the main antiviral agents for treating chronic hepatitis B (CHB) [Citation3]. However, NA resistance is a major public health concern in recent decades [Citation4].
Tenofovir disoproxil fumarate (TDF) is a potent NA with a high barrier to resistance in treating chronic HBV or HIV infection [Citation5]. Although renal and bone toxicities were reported during TDF treatment, it was well tolerated in the globally registered phase III clinical trial and phase III clinical trial in China [Citation6,Citation7]. Renal function remained stable in European studies [Citation1,Citation8], even for patients with abnormal baseline estimated glomerular filtration rate (eGFR) [Citation9,Citation10]. We previously found that eGFR was partially restored in a 2-year real-world study, but it was difficult to select patients with reversible eGFR [Citation11,Citation12].
Moreover, a significant reduction in low-density lipoprotein (LDL) was reported in patients with HIV infection after TDF treatment [Citation13,Citation14], which may be potentially beneficial for the prevention of cardiovascular diseases. LDL was increased in patients switching from TDF to tenofovir alafenamide (TAF)-containing regimen [Citation15]. Moreover, total cholesterol and triglyceride (TG) decreased significantly after switching back from TAF to TDF [Citation16].
In addition, patients treated with TDF had lower TG levels than those in the non-TDF group [Citation17]. However, whether TDF impacts lipid profile in patients with CHB, and the relationship between lipid profile and eGFR remain unclear.
In the present 3-year real-world study, we analyzed the dynamic changes of eGFR and lipid profile in patients with CHB and hypertriglyceridemia and provided evidence for selecting patients with reversible eGFR.
Methods
Study population and data collection
A total of 355 patients with CHB were prospectively recruited from the Third People’s Hospital of Changzhou and Nanjing Drum Tower Hospital, Nanjing University Medical School. Until the last follow-up visit on 20 November 2021, data from 203 patients who had taken TDF for three years, were analyzed. Hypertriglyceridemia was defined as a serum TG level >1.7 mmol/L [Citation18]. Demographic and laboratory data, including age, sex, alanine transaminase (ALT), aspartate aminotransferase (AST), total bilirubin, total cholesterol, eGFR, TG, cholesterol (CHOL), creatinine, phosphorus, HBV serological markers, and HBV DNA, were collected at baseline, first, second and third year. Reversible eGFR was confirmed when the GFR increased by 30 ml/(min·1.73m2) or a 25% increase compared to the lowest level [Citation18].
The study was approved by the Ethics Committee of the Third People’s Hospital of Changzhou. As described in our previous study, [Citation8] it is a prospective cohort study wherein all consecutive individuals with chronic HBV infection (non-hypertriglyceridemia and hypertriglyceridemia), who initiated the first prescription of TDF between January 2016 and May 2017, were prospectively recruited, and all individuals signed consent to participate during this period.
Statistical analysis
All data were analyzed using SPSS 23.0 software (Chicago, IL, USA). Continuous variables were presented as the median and interquartile range (IQR), and were compared using Mann-Whitney U tests. Categorical variables were expressed as frequencies, and analyzed by the Chi-square test. Risk factors for eGFR recovery were analyzed using logistic regression analyses. A p value <0.05 was considered statistically significant.
Results
Baseline characteristics of patients
Among the 203 patients, 20 were diagnosed with hypertriglyceridemia. The baseline characteristics of enrolled patients are shown in . Baseline ALT was significantly higher in the hypertriglyceridemia group (p = 0.05), and there was no significant difference in baseline eGFR, creatinine and HBV DNA between the two groups.
Table 1. Demographic and clinical characteristics of the patients.
Table 2. Risk factors for partial recovery of eGFR in patients with TG <1.7 mmol/L.
Dynamic changes in eGFR, TG and CHOL during 3-year TDF treatment
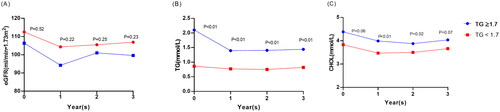
For patients with hypertriglyceridemia, eGFR and CHOL did not change significantly during 3-year follow-up, while TG decreased significantly at the first year and persisted at a lower level in the subsequent two years ().
Figure 1. Dynamic changes of eGFR, TG, and CHOL in patients with and without hypertriglyceridemia. (A) total population; (B) patients with hypertriglyceridemia; (C) patients without hypertriglyceridemia. *, p < 0.05. eGFR, estimated glomerular filtration rate; TG, triglyceride; CHOL, cholesterol.

For patients without hypertriglyceridemia, eGFR declined significantly in the first year of treatment, and then gradually recovered during the subsequent two years (). Moreover, TG and CHOL had similar changes as eGFR.
Both TG and CHOL were higher in the hypertriglyceridemia group than in the non-hypertriglyceridemia group at all time points ().
Correlation between eGFR, TG and CHOL
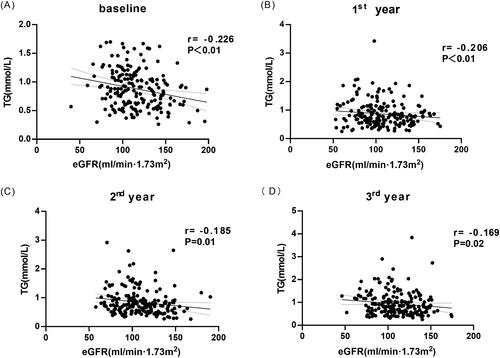
For patients with TG <1.7 mmol/L, eGFR was negatively correlated with TG at all time points (all p < 0.05). For patients with hypertriglyceridemia, the correlations between eGFR and TG were not significant (all p > 0.05) ().
For patients with TG <1.7 mmol/L, the correlations between eGFR and CHOL were not significant (p > 0.05) except for the second-year time point (r=-0.166, p = 0.03). For patients with hypertriglyceridemia, the correlations between eGFR and CHOL were not significant at all time points (all p > 0.05).
Risk factors for eGFR recovery at the third year in the TG <1.7 mmol/L group
Among the 183 patients without hypertriglyceridemia, 15 patients experienced partial recovery of eGFR in the third year. Univariate analysis showed that age and baseline eGFR <90 mL/(min·1.73 m2) were related to partial recovery of eGFR in the third year, and multivariate analysis validated that age (OR: 0.886, 95% CI [0.817–0.960], p < 0.01) and baseline eGFR <90 mL/(min·1.73 m2)(OR: 0.073, 95% CI [0.019–0.284], p < 0.01) were independent risk factors for partial recovery of eGFR ().
Discussion
In the present study, we investigated the dynamic changes of eGFR, CHOL and TG in patients with and without hypertriglyceridemia during TDF treatment. Fifteen (15/183, 8.2%) patients with normal TG experienced partial recovery of eGFR. Multivariate analysis showed that age and baseline eGFR <90 mL/(min·1.73 m2) were independent risk factors for eGFR recovery in the third year. Drug-resistance is a major concern due to the widespread use of antivirals, and TDF is one of the first-line agents for treating CHB [Citation4]. Although nephrotoxicity is a potential side effect, data from the present study suggested that patients may benefit from TDF in terms of TG regulation. Interestingly, TG showed no significant relationship with eGFR in patients with hypertriglyceridemia, while TG was negatively correlated with eGFR in patients without hypertriglyceridemia. It has been reported that TG has a negative relationship with eGFR in children and adolescents [Citation11]. Our previous study also showed that TG negatively correlated with eGFR in patients without overweight [Citation19]. Decreased eGFR may result from delayed hepatic clearance of lipoproteins during dyslipidemia [Citation20]. Taking together, these findings suggest that the correlation between TG and eGFR is complicated, and down-regulation of TG may help to prevent renal function deterioration during TDF treatment. To note, patients with hypertriglyceridemia are few in the present study, further studies are necessary to validate these findings.
Recently, data from a large cohort study showed that elevated TG and reduced HDL-C levels were associated with the onset of advanced chronic kidney disease (CKD) [Citation21]. In addition, the ratio of TG to HDL-C, which is associated with insulin resistance [Citation22] and cardiovascular events, was found to be associated with the risk of CKD in the Japanese population [Citation23], while another study showed that elevated TG/HDL-C was positively correlated with CKD development in Korean males but not females [Citation24]. It would be more interesting to investigate the relationship between TG/HDL ratio and eGFR during TDF treatment. It is a pity that we did not test HDL in most patients in the present study, so the TG/HDL ratio as well as its relationship with eGFR could not be calculated.
In the present study, eGFR was found to be relatively stable in patients with hypertriglyceridemia during the 3-year follow-up, and a significant decrease in TG may have contributed to the stabilization of eGFR. This important finding suggests that TDF may be more suitable in patients with hypertriglyceridemia. Considering that the underlying mechanisms remain unclear, whether the decrease of eGFR can be alleviated by a combination of TDF and hypolipidemic drugs, remains unknown. Although TG is a risk factor for cardiovascular events, but the hypolipidemic drug is cautiously recommended for patients with underlying liver disease.
Moreover, age and baseline eGFR <90 mL/(min·1.73 m2), but not TG, were independent risk factors for eGFR recovery in the third year. Notably, another important finding was that eGFR could partially recover in patients without hypertriglyceridemia, especially younger patients. Few patients with baseline eGFR <90 mL/(min·1.73 m2) experienced eGFR recovery, which may be due to the compensatory mechanisms of the kidneys. Although TG is not independently related to eGFR recovery, it has a negative relationship with eGFR and it may be an important indicator to guide the treatment revision. Basic research studies on TG metabolism are warranted to reveal the mechanisms of TG decline and its protective effect on eGFR.
This study had several limitations. First, the mechanisms underlying eGFR recovery and its relationship with TG remain unknown. Second, the sample size was relatively small, especially for patients with hypertriglyceridemia, and multi-center studies with large sample size are needed to validate these findings. Third, fewer patients receiving hypolipidemic drugs were included, thus the renal protective effects of hypolipidemic drugs combined with TDF, could not be analyzed in the present study.
Conclusions
Partial recovery of eGFR was observed in patients without hypertriglyceridemia during TDF treatment, and TG regulation might be a useful strategy to hinder renal function decline, although larger, confirmatory studies are necessary to validate our findings.
Author contributions
Jian-chun Lu and Long-gen Liu conceived and designed the study. Ya-ru Pan, Si-qi Liu, Yi-shan He, Yuan Xue, Jian Wang, Rui Huang, Chao Wu, Jian-chun Lu and Long-gen Liu collected and confirmed the data. Ya-ru Pan and Si-qi Liu analyzed the data and drafted the manuscript. Yuan Xue, Jian-chun Lu and Long-gen Liu revised the manuscript. All authors read and approved the final manuscript. Ya-ru Pan and Si-qi Liu contributed equally to this work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data are available from the corresponding author upon request.
Additional information
Funding
References
- Agarwal K, Brunetto M, Seto WK, et al. 96 weeks treatment of tenofovir alafenamide vs. tenofovir disoproxil fumarate for hepatitis B virus infection. J Hepatol. 2018;68(4):672–681.
- Baldin G, Ciccullo A, Capetti A, et al. Efficacy and safety of switching to dolutegravir plus emtricitabine/tenofovir disoproxil fumarate (TDF) or elvitegravir/cobicistat/emtricitabine/TDF in virologically suppressed HIV-infected patients in clinical practice: results from a multicentre, observational study. HIV Med. 2019;20(2):164–168.
- Bazinet M, Pântea V, Placinta G, et al. Safety and efficacy of 48 weeks REP 2139 or REP 2165, tenofovir disoproxil, and pegylated interferon alfa-2a in patients with chronic HBV infection naïve to nucleos(t)ide therapy. Gastroenterology. 2020;158(8):2180–2194.
- Pan CQ, Afdhal NH, Ankoma-Sey V, et al. First-line therapies for hepatitis B in the United States: a 3-year prospective and multicenter real-world study after approval of tenofovir alefenamide. Hepatol Commun. 2022;6(8):1881–1894.
- Charlton MR, Alam A, Shukla A, et al. An expert review on the use of tenofovir alafenamide for the treatment of chronic hepatitis B virus infection in Asia. J Gastroenterol. 2020;55(9):811–823.
- Fanning GC, Zoulim F, Hou J, et al. Therapeutic strategies for hepatitis B virus infection: towards a cure. Nat Rev Drug Discov. 2019;18(11):827–844.
- Yang YM, Choi EJ. Renal safety of tenofovir and/or entecavir in patients with chronic HBV monoinfection. Ther Clin Risk Manag. 2017;13:1273–1285.
- Zheng S, Liu L, Lu J, et al. Efficacy and safety of tenofovir disoproxil fumarate in Chinese patients with chronic hepatitis B virus infection: a 2-year prospective study. Medicine . 2019;98(42):e17590.
- Curran A, Rull A, Navarro J, et al. Lipidomics reveals reduced inflammatory lipid species and storage lipids after switching from EFV/FTC/TDF to RPV/FTC/TDF: a randomized open-label trial. J Clin Med. 2020;9(5):1246.
- Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. Aids. 2019;33(9):1455–1465.
- Moafi M, Assadi F, Heshmat R, et al. Impact of dyslipidemia on estimated glomerular filtration rate in apparently healthy children and adolescents: the CASPIAN-V study. World J Pediatr. 2019;15(5):471–475.
- Marcellin P, Zoulim F, Hézode C, et al. Effectiveness and safety of tenofovir disoproxil fumarate in chronic hepatitis B: a 3-year, prospective, real-world study in France. Dig Dis Sci. 2016;61(10):3072–3083.
- Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/tenofovir disoproxil fumarate (TDF) versus efavirenz/emtricitabine/TDF in treatment-© adults with human immunodeficiency virus type 1 infection: week 96 results of the randomized, double-blind. Clin Infect Dis. 2021;73(1):33–42.
- Pilkington V, Hughes SL, Pepperrell T, et al. Tenofovir alafenamide vs. tenofovir disoproxil fumarate: an updated meta-analysis of 14 894 patients across 14 trials. AIDS. 2020;34(15):2259–2268.
- Squillace N, Ricci E, Menzaghi B, et al. The effect of switching from tenofovir disoproxil fumarate (TDF) to tenofovir alafenamide (TAF) on liver enzymes, glucose, and lipid profile. Drug Des Devel Ther. 2020;14:5515–5520.
- Milinkovic A, Berger F, Arenas-Pinto A, et al. Reversible effect on lipids by switching from tenofovir disoproxil fumarate to tenofovir alafenamide and back. AIDS. 2019;33(15):2387–2391.
- Yang J, Chen J, Ji Y, et al. Lipid profile and renal safety of tenofovir disoproxil fumarate-based anti-retroviral therapy in HIV-infected Chinese patients. Int J Infect Dis. 2019;83:64–71.
- Birken SA, Powell BJ, Presseau J, et al. Combined use of the consolidated framework for implementation research (CFIR) and the theoretical domains framework (TDF): a systematic review. Implement Sci. 2017;12(1):2.
- Liu SQ, Zhang XJ, Xue Y, et al. Dynamic changes of estimated glomerular filtration rate are conversely related to triglyceride in non-overweight patients. World J Clin Cases. 2022;10(31):11371–11380.
- Cases A, Coll E. Dyslipidemia and the progression of renal disease in chronic renal failure patients. Kidney Int Suppl. 2005;(99):S87–S93.
- Weldegiorgis M, Woodward M. Elevated triglycerides and reduced high-density lipoprotein cholesterol are independently associated with the onset of advanced chronic kidney disease: a cohort study of 911,360 individuals from the United Kingdom. BMC Nephrol. 2022;23(1):312.
- Kim J, Shin SJ, Kim YS, et al. Positive association between the ratio of triglycerides to high-density lipoprotein cholesterol and diabetes incidence in Korean adults. Cardiovasc Diabetol. 2021;20(1):183.
- Tsuruya K, Yoshida H, Nagata M, et al. Association of the triglycerides to high-density lipoprotein cholesterol ratio with the risk of chronic kidney disease: analysis in a large Japanese population. Atherosclerosis. 2014;233(1):260–267.
- Kim J, Bae YJ, Shin SJ, et al. The ratio of triglycerides to high-density lipoprotein cholesterol is associated with the risk of chronic kidney disease in Korean men. Lipids. 2021;56(5):475–483.