Abstract
Objective
Exercise has traditionally been viewed as a contraindication for individuals with asthma, as it was believed to trigger or worsen acute asthma attacks. However, with scientific and appropriate exercise training, it has been proven that respiratory function and exercise capacity can be effectively improved and enhanced in asthma patients. This study aimed to compare the effects of different types of exercise on pulmonary function in adult patients with asthma using Network Meta-analysis.
Methods
We conducted a comprehensive search of electronic databases such as PubMed, Cochrane Library, Web of Science, CNKI for randomized controlled trials (RCTs) that investigated the effects of exercise on lung function in adult patients with asthma from inception to February 2023. Information including on first author, publication time, total sample size, intervention period, interventions, and outcome indicators were collected, and relevant statistical analyses were performed using Stata 17.0 software and Revman 5.4.
Results
A total of 28 randomized controlled trials with 2,155 patients with asthma were finally included. The results of Network Meta-analysis showed that compared with control group, breathing training (BT)、aerobic training (AT)、relaxation training (RT)、yoga training (YG) and breathing combined with aerobic training (BT + AT) improved Forced Expiratory Volume in the first second (FEV1) levels; AT、BT、YG and BT + AT improved the level of Forced Vital Capacity (FVC); BT、AT、RT、YG and BT + AT improved Peak Expiratory Flow (PEF); BT、AT、and YG improved Forced Expiratory Volume in the first second/Forced Vital Capacity (FEV1/FVC).The results of SUCRA probability ranking showed that RT had the most significant effect on improving the FEV1[SMD = 1.13,95%CI(0.83,1.43), p<0.001] levels, BT + AT had the most significant effect on improving the FVC[SMD = 0.71,95%CI(0.47,0.95), p<0.001] level; YG had the most significant effect on improving the PEF[SMD = 0.79,95%CI(0.55,1.02), p<0.001] level.
Conclusions
BT + AT and YG may be more advantageous in improving lung function in adult asthmatics.
1. Introduction
Bronchial asthma, or simply asthma, is a heterogeneous disease characterized by recurring episodes of wheezing, shortness of breath, chest tightness, and cough [Citation1]. It is influenced by both genetic and environmental factors, affecting a considerable population of approximately 339 million individuals worldwide and imposing a significant burden on healthcare systems [Citation2].
Traditionally, exercise has been perceived as contraindicated for individuals with asthma due to the potential risk of inducing or exacerbating acute asthma attacks [Citation3]. However, some studies have shown that scientific and reasonable exercise training can effectively improve and enhance the level of respiratory function and exercise capacity in asthma patients [Citation4]. Respiratory training plays a vital role in the rehabilitation of asthma patients. Targeted nursing training can effectively enhance the endurance of respiratory muscles, promote diaphragm movement, reduce respiratory oxygen consumption, increase tidal volume, and improve pulmonary ventilation function. Aerobic training, combining chest breathing with diaphragmatic breathing, particularly emphasizing diaphragmatic breathing, facilitates the contraction and relaxation of the diaphragm. This rhythmic movement of the diaphragm increases, creating variations in chest and abdominal pressure, ensuring ample blood supply to the respiratory organs. Relaxation training can enhance the ventilation function of asthma patients by eliminating negative excitatory focus in the cerebral cortex, stabilizing the regulatory function of the neuroendocrine system, reducing the release of inflammatory mediators, and alleviating bronchial mucosal edema. Furthermore, yoga incorporates various movements such as twists, forward bends, and backward bends, which stimulate blood circulation, metabolic rate, and expand the chest cavity. Through deep lung breathing, yoga practice massages the internal organs, while the combination of chest and diaphragmatic breathing improves organ function. Systematic reviews have consistently demonstrated the positive association between exercise and aerobic capacity in individuals with asthma, revealing significant improvements in maximal oxygen consumption and endurance [Citation5,Citation6]. A meta-analysis on the effects of breathing training on pulmonary function in adult asthmatics highlighted notable improvements across various parameters [Citation7].
Currently, in the existing randomized controlled trials (RCTs) conducted on adult asthma patients, there are variations in specific exercise intervention methods, leading to a need for improvement in evidence-based medicine. The effectiveness of different exercise rehabilitation training programs on lung function in adult asthma patients remains a subject of debate and shows heterogeneity among studies. Despite these promising findings, there is still a need to investigate the optimal exercise intervention modalities for adult asthma patients based on evidence-based medical evidence [Citation8]. Therefore, this study further analyzed and evaluated randomized controlled studies regarding exercise intervention on pulmonary function in adult asthma patients using network Meta-analysis to provide a scientific basis for conducting clinical work and further research.
2. Materials and methods
2.1. Methods
This systematic review and meta-analysis was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [Citation9]. The protocol of this systematic review was published in the International Prospective Register of Systematic Reviews (PROSPERO-CRD42023437033).
2.2. Search strategy
A comprehensive search was conducted in electronic databases including PubMed, Cochrane Library, Web of Science, and CNKI to identify relevant literature on the impact of exercise interventions on lung function in adult patients with asthma. The search spanned from the inception of the databases up to February 2023. We used mesh terms: (exercise OR training OR TaiChi OR Yoga OR aerobics OR intermittent movement OR exercise prescription OR breathing exercise OR movement OR breathing) AND (asthma OR bronchial asthma) as search strategy. In addition, references of included studies were retrospectively included to supplement access to relevant literature.
2.3. Inclusion and exclusion criteria
For the search strategy, four domains, namely participants, intervention, outcomes, and study design, were utilized. The key terms selected were as follows: (1) participants: asthma OR bronchial spasm OR bronchoconstriction; (2) intervention: Exercise OR Breathing training (BT) OR Aerobic training (AT) OR Relaxation training (RT) OR Yoga training (YG) OR Breathing training and Aerobic training (BT + AT); (3) outcomes: Forced Expiratory Volume in the first second (FEV1) OR Forced Vital Capacity (FVC) OR Peak Expiratory Flow (PEF) OR Forced Expiratory Volume in the first second/Forced Vital Capacity (FEV1/FVC); (4) study design: the search strategy recommended by Cochrane was employed to include Randomized Controlled Trials (RCTs) and quasi-experimental studies. The general search strategy was then tailored to each specific database.
Exclusion criteria: (1) duplication of published literature; (2) unavailable full-text literature; (3) literature with abstracts only; (4) unavailable or transformed data in the original study.
2.4. Assessment of methodological quality
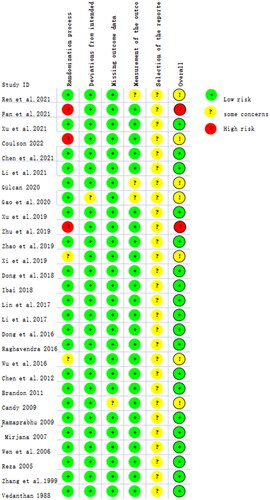
Two independent reviewers assessed the methodological quality of included studies using the revised Cochrane's risk of bias tool (ROB2) [Citation10]. The literature was evaluated from five aspects: randomization process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of the reported result. Upon evaluation, it was found that nine reports had at least one domain with an 'unclear risk', indicating insufficient information to make a clear judgment. Additionally, nine reports had at least one domain with a 'high risk', suggesting a substantial risk of bias in those domains. Specifically, three reports raised concerns regarding the randomization process, indicating potential issues in the allocation of participants to intervention groups.
2.5. Data extraction
The following variables from the included studies were extracted independently by two authors: (1) characteristics of the study (authors, year of publication, and study design) and the sample (size and age); (2) description of the program conducted by the training (type of intervention) and control group; (3) FEV1, FVC, PEF, and FEV1/FVC; (4) overall effect of the outcome of interest. If insufficient data were reported in the published article or supplementary material provided, the corresponding author was contacted to request further data.
2.6. Statistical methods
In this study, the software Stata 17.0 and Revman 5.4 were utilized for conducting the network Meta-analysis. The study adhered to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020). Standardized mean difference (SMD) and 95% CI were used as effect sizes for outcome indicators of continuous variables. When I2 <50% and p > 0.1, it indicated no significant heterogeneity among independent studies, and fixed-effects model was used; surface under the cumulative ranking (SUCRA) was utilized to rank and compare various exercise interventions. When there were three or more studies focusing on the same exercise intervention, an effect ranking was performed. The SUCRA value, ranging from 0 to 100, indicated the effectiveness of each intervention, with higher values indicating better intervention outcomes. By evaluating the SUCRA values of Bone Mineral Density (BMD) in the lumbar spine, femoral neck, and Ward's triangle, cluster stratification analysis was employed to identify the most optimal exercise interventions. This approach allows for a comprehensive assessment and comparison of the interventions, enabling researchers to determine the most effective exercise strategies for improving BMD in different anatomical regions.
3. Results
3.1. Search results
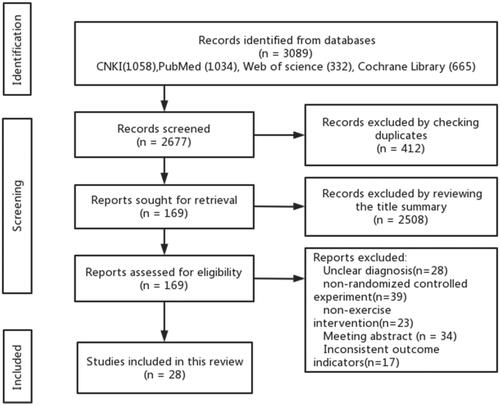
The initial electronic search yielded a total of 3,089 articles that were potentially relevant to the study. After removing duplicates, 2,677 articles underwent screening based on title and abstract. From this, the full texts of 169 articles were assessed for eligibility according to the predetermined inclusion and exclusion criteria. Ultimately, 28 articles met the inclusion criteria and were included in the present review ().
3.2. Basic characteristics of the included literature
Among the included literature, a total of 28 randomized controlled trials (RCTs) were identified, with 18 articles published in Chinese literature and 10 articles in English literature. Among these studies, 3 were multi-arm studies, involving multiple interventions in .
Table 1. Basic characteristics of the included literature.
3.3. Assessment of methodological quality
The methodological quality of the 28 RCTs included in the study was assessed for risk of bias. Among these studies, 26 were rated as 'low risk' or 'having some concerns' regarding bias, while 2 studies were rated as 'high risk' due to inadequate information regarding outcome measurement and missing outcome data ().
3.4. Consistency analysis results
The included 28 randomized controlled trials (RCTs) were subjected to nodal analysis to assess for inconsistency. The nodal analysis model revealed that the results of the comparisons for Forced Expiratory Volume in the first second (FEV1) (p = 0.345), Forced Vital Capacity (FVC) (p = 0.157), and Peak Expiratory Flow (PEF) (p = 0.215) were all greater than 0.05, indicating that the direct and indirect comparisons were consistent. As a result, the consistency model was deemed appropriate for further analysis.
3.5. Network meta-analysis
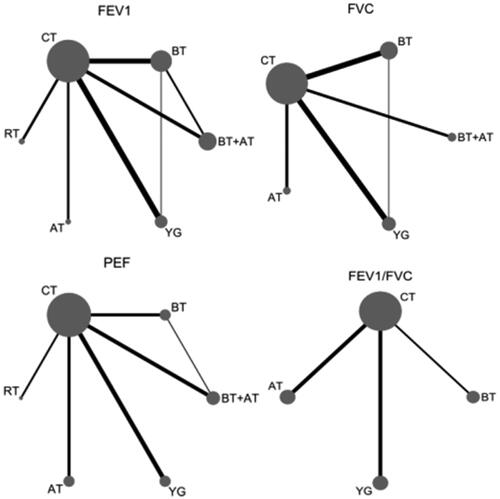
A total of 28 RCTs were included, including 8 studies comparing BT with CT [11–14, 19, 20, 27, 31], 7 studies comparing AT with CT [15, 21–23, 31, 34, 36]; 3 studies comparing RT with CT [25, 35, 36]; 3 studies comparing YG with CG [17, 32, 33]; and 5 studies comparing BT + AT with CT [16, 18, 26, 30, 31]; 2 studies comparing BT + AT with BT [24, 29].
3.5.1. Network meta-analysis of FEV1
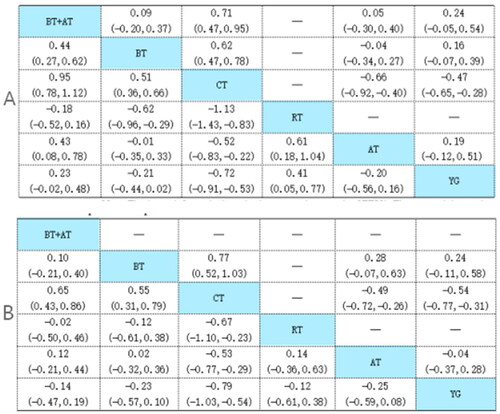
A total of 22 publications and 1,670 subjects were involved. The results of network Meta-analysis showed that AT[SMD = 0.52,95%CI(0.22,0.82), p < 0.001], BT[SMD = 0.53, 95%CI(0.36,0.71), p < 0.001], RT[SMD = 1.13,95%CI(0.84,1.42), p < 0.001], YG[SMD = 0.67,95%CI(0.48,0.87), p < 0.001] and BT + AT[SMD = 0.98,95%CI(0.77,1.18), p < 0.001] all demonstrated improvement on FEV1. The differences between the exercise modalities compared with each other were not statistically significant (p > 0.05; ). The results of SUCRA probability showed that RT was the most effective and BT was the least effective in improving FEV1 ().
Table 2. Probability ranking results of different exercise styles on FEV1, FVC, PEF and FEV1/FVC.
3.5.2. Network meta-analysis of FVC
A total of 17 publications and 1,297 subjects were involved. The results of network Meta-analysis showed that AT[SMD = 0.53,95%CI(0.30,0.76), p < 0.001], BT[SMD = 0.66,95%CI(0.50,0.83), p < 0.001], YG[SMD = 0.42,95%CI(0.22,0.61), p < 0.001] and BT + AT[SMD = 0.71,95%CI(0.47,0.95), p < 0.001] all demonstrated improvement on FVC. The differences between the exercise modalities compared with each other were not statistically significant (p > 0.05; ). The results of SUCRA probability showed that BT + AT was the most effective and YG was the least effective in improving FVC ().
3.5.3. Network meta-analysis of PEF
A total of 17 publications and 1,256 subjects were involved. The results of network Meta-analysis showed that BT[SMD = 0.61,95%CI(0.36,0.85), p < 0.001], AT[SMD = 0.53,95%CI(0.30,0.76), p < 0.001], RT[SMD = 0.67,95%CI(0.24,1.09), p = 0.002], YG[SMD = 0.79,95%CI(0.53,1.02), p < 0.001] and BT + AT[SMD = 0.60,95%CI(0.38,0.82), p < 0.001] all demonstrated improvement on PEF. The differences between the exercise modalities compared with each other were not statistically significant (p > 0.05; ). The results of SUCRA probability showed that YG was the most effective and AT was the least effective in improving PEF ().
Figure 5. Relative effect estimates for the contrasts between the different exercise intervention and placebo arms on FEV1, FVC, PEF and FEV1/FVC. Note A: the upper right part of the top table in the figure represents FVC, and its lower left part represents FEV1; Note B: the upper right part of the middle table in the figure represents FEV1/FVC, and the lower left part represents PEF.
3.5.4. Network meta-analysis of FEV1/FVC
A total of 10 publications and 637 subjects were involved. The results of network Meta-analysis showed that BT[SMD = 0.77,95%CI(0.52,1.03), p < 0.001], AT[SMD = 0.49,95%CI(0.26,0.72), p < 0.001], and YG[SMD = 0.54,95%CI(0.31,0.77), p < 0.001] all demonstrated improvement on FEV1/FVC. The differences between the exercise modalities compared with each other were not statistically significant (p > 0.05; ). The results of SUCRA probability showed that BT was the most effective and AT was the least effective in improving FEV1/FVC ().
3.6. Publication bias
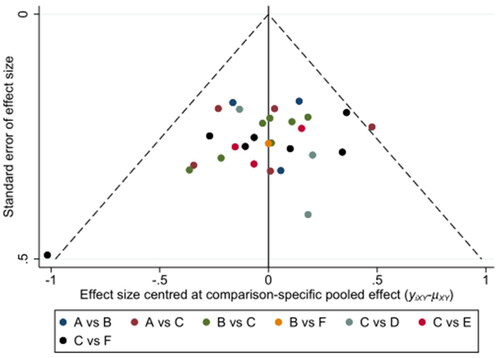
The assessment of publication bias was conducted using the funnel plot for the comparison of Forced Expiratory Volume in the first second (FEV1). The funnel plot displayed a symmetrical distribution of studies on both sides of the middle line in the upper part, indicating a lower likelihood of publication bias. However, there was a scatter point observed at the bottom of the funnel plot, suggesting the presence of a small sample effect ().
4. Discussion
In recent years, exercise intervention has gained widespread popularity in the field of complementary alternative medicine [Citation39]. The Global Initiative for Asthma (GINA) emphasizes that patients with asthma may experience varying degrees of altered pulmonary ventilation function at different times, often manifesting as a decrease in FEV1 and FEV1/FVC. Therefore, pulmonary ventilation function tests are used as an important tool for diagnosing asthma and for assessing the severity and level of control of asthma. Studies have shown that exercise can promote longitudinal growth of lung volume, improve the FEV1, FVC, FEV1/FVC and PEF indexes, and improve lung function in asthmatic patients. This results in less frequent emergency room visits, less frequent hospitalizations and fewer days in the hospital. It can also reduce the overall medication and economic burden of patients with asthma [Citation40], which has positive implications for the rehabilitation of asthma patients. This article uses the network meta-analysis method to comprehensively analyze the research results of multiple different exercise modes, and displays the clustering and layering results. Through direct and indirect comparison with p-values greater than 0.05, it indicates that the study is reliable and accurate, and provides more specific guidance for intervention in asthma patients. The results of this study showed that five exercise interventions, including BT, AT, RT, YG, and BT + AT were superior in improving lung function in adult asthmatics compared with the conventional rehabilitation control group, YG, BT + AT are the optimal training to improve pulmonary function in adult asthma patients [Citation41].
BT combined with AT can enhance the physical and psychological condition of adult asthmatics, primarily through the reinforcement of respiratory function during exercise. The combination of thoracic and abdominal breathing, with an emphasis on abdominal breathing, increases diaphragmatic contraction, facilitating diaphragmatic rise and fall and improving respiratory organ function by continuously altering thoracic and abdominal pressures. YG predominantly involves twisting, forward bending, and backward bending positions, which can enhance blood circulation, metabolism, and chest cavity volume. Additionally, YG incorporates lung breathing techniques that massage internal organs and improve their function. Through specific breathing training, the diaphragm within the lungs can be activated, leading to increased alveolar mobility and improved muscle activity and coordination during the respiratory cycle. Consequently, this results in substantial changes in intrapulmonary pressure, enhanced alveolar expansion and contraction, and expansion of the respiratory tract, reducing airway resistance and promoting lung ventilation and gas exchange [Citation42]. Therefore, BT + AT and YG may represent the most effective intervention methods for enhancing lung function in adult asthmatics.
The meta-analysis presented in this study has several strengths that contribute to its reliability and validity. It adheres to the latest PRISMA 2020 statement and follows a prospective protocol registration on PROSPERO, which ensures scientific rigor and provides a solid foundation for clinical prevention measures. However, there are also limitations that should be acknowledged, potentially affecting the generalizability of the results: (1) There is inherent variability among the included studies, including individual differences and variations in the type, intensity, frequency, and duration of exercise interventions. These differences may introduce heterogeneity and influence the overall interpretation of the results. (2) The majority of the patients included in the study were under 60 years of age. Therefore, caution should be exercised when extrapolating the findings to patients over 60 years of age, as their response to exercise interventions may differ. (3) Exercise prescription typically considers factors such as exercise type, duration, intensity, and frequency. However, the included randomized controlled trials did not consistently provide detailed descriptions of exercise intensity and frequency. Moreover, the limited number of studies available did not allow for subgroup analysis specifically focused on intensity and frequency.
5. Conclusions
According to the study findings, the exercise interventions of BT + AT and YG are effective in improving lung function in adult asthmatics. These findings can serve as valuable references for exercise prescription in this population. However, it is crucial to consider individual factors, such as patient characteristics, family history, environmental influences, and disease duration, when designing exercise programs. Tailoring interventions to individual physical and mental health conditions, with careful consideration of exercise intensity, frequency, and duration, is important for optimizing treatment outcomes. Future research should aim for objective, standardized, and well-designed experimental studies focusing on various aspects such as exercise mode, intensity, frequency, age, and gender. Large-scale, diversified, double-blind randomized controlled trials are needed to further validate and expand upon the findings of this study.
Authors' contributions
StX and SjF searched the literatures, analyzed data and wrote manuscript. StX and DZ supported writing manuscript. All authors have read and agreed to the published version of the manuscript.
Author disclaimer'
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
Disclosure statement
The authors declare no conflict of interest.
Data availability statement
All data generated or analysed during this study are included in this published article.
Additional information
Funding
References
- Group, A. Chinese society of respiratory medicine. Bronchial asthma guidelines (2020 edition). Chin J Tubercul Respir Dis. 2020;43:1–11. doi: 10.3760/cma.j.cn112147-20200618-00721.
- Menzies-Gow A, Bafadhel M, Busse WW, et al. An expert consensus framework for asthma remission as a treatment goal. J Allergy Clin Immunol. 2020;145(3):757–765. doi: 10.1016/j.jaci.2019.12.006.
- Coelho CM, Reboredo MM, Valle FM, et al. Effects of an unsupervised pedometer-based physical activity program on daily steps of adults with moderate to severe asthma: a randomized controlled trial. J Sports Sci. 2018;36(10):1186–1193. doi: 10.1080/02640414.2017.1364402.
- Hou YS, Li J, Hou L. The effect of rehabilitation exercise prescription on breathing function of teenage bronchial asthma sufferers. J Phys Educ. 2006;13:58–60. doi: 10.3969/j.issn.1006-7116.2006.01.018.
- Carson KV, Chandratilleke MG, Picot J, et al. Physical training for asthma. Cochrane Database Syst Rev. 2013;30(9):CD001116. doi: 10.1002/14651858.CD001116.pub4.
- Eichenberger PA, Diener SN, Kofmehl R, et al. Effects of exercise training on airway hyperreactivity in asthma: a systematic review and meta-analysis. Sports Med. 2013;43(11):1157–1170. doi: 10.1007/s40279-013-0077-2.
- Ana L, Bouza CL, Cristina J, et al. Effect of respiratory muscle training in asthma: a systematic review and meta-analysis. Ann Phys Rehabil Med. 2022;66(3):101691.
- Liu F, Liu YR, Liu L Effect of exercise rehabilitation on exercise capacity and quality of life in children with bronchial asthma: a systematic review. Zhongguo Dang Dai Er Ke Za Zhi. 2021;23(10):1050–1057. doi: 10.7499/j.issn.1008-8830.2104124.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71.
- Cumpston MS, McKenzie JE, Welch VA, et al. Strengthening systematic reviews in public health: guidance in the cochrane handbook for systematic reviews of interventions, 2nd edition. J Public Health (Oxf). 2022;44(4):e588–e592. doi: 10.1093/pubmed/fdac036.
- Ren YJ. Clinical observation of montelukast sodium combined with hanchuan zupa granules and respiratory exercise for treating cough variant asthma with wind–cold attacking lung syndrome in adults. J Baot Med Coll. 2021;37:88–91,100. doi: 10.16833/j.cnki.jbmc.2021.07.019.
- Fan YQ, Zhang C, Zhu YX, et al. Clinical effect of Expiration-Inspiration breathing exercise combined with acupoint application in treatment of chronic persistent bronchical asthma. J Anhui Univ Chin Med. 2021;40:55–59. doi: 10.3969/j.issn.2095-7246.2021.03.015.
- Xu RQ. Effects of breathing exercises combined with lip contraction and abdominal breathing training on lung function and exercise tolerance in patients with asthma. China Pract Med. 2021;16:191–193. doi: 10.14163/j.cnki.11-5547/r.2021.16.073.
- Coulson E, Carpenter LM, Georgia TE, et al. Breathing exercises in older adults with asthma: a blinded, randomized, placebo-controlled trial. J Asthma. 2022;59(7):1438–1444. doi: 10.1080/02770903.2021.1936015.
- Chen DL. Effect of baduanjin combined with compound ipratropium bromide on bronchial asthma and lung function. Med Forum. 2021;25:74–75. doi: 10.19435/j.1672-1721.2021.01.038.
- Li D, Shi YQ. Effect of respiratory training combined with exercise therapy on exercise endurance and pulmonary function of the patients with asthma in stable stages. China Modern Doctor. 2021;59:29–32.
- Bahçecioğlu Turan G, Tan M. The effect of yoga on respiratory functions, symptom control and life quality of asthma patients: a randomized controlled study. Complement Ther Clin Pract. 2020;38:101070. doi: 10.1016/j.ctcp.2019.101070.
- Gao W. Effectiveness analysis of respiratory training combined with exercise therapy in patients with asthma remission stage. China Practical Medical. 2020;15:154–156. doi: 10.14163/j.cnki.11-5547/r.2020.24.068.
- Xu JL, Zhu JH. Effect of abdominal breathing combined with biofeedback training on lung function and quality of life in patients with asthma. Nurs Pract Res. 2019;16:62–63. doi: 10.3969/j.issn.1672-9676.2019.21.025.
- Zhu WW. Effects of vertical breathing exercises combined with lip contraction and abdominal breathing on exercise tolerance and quality of life in patients with asthma. Nurs Pract Res. 2019;16:77–79. doi: 10.3969/j.issn.1672-9676.2019.23.032.
- Zhao L. Observation on the application of wuqinxi exercise in patients with bronchial asthma in remission stage. Mod Diag Treat. 2019;30:4076–4078.
- Xi YZ. Application and value evaluation of exercise therapy in clinical treatment of senile asthma. Home Med. 2019;001(006):131.
- Dong LH. Efficacy of power bicycle training in the treatment of bronchial asthma. Biped Health. 2018;27(15):99–100. doi: 10.19589/j.cnki.issn1004-6569.2018.15.099.
- López-de-Uralde-Villanueva I, Candelas-Fernández P, de-Diego-Cano B, et al. The effectiveness of combining inspiratory muscle training with manual therapy and a therapeutic exercise program on maximum inspiratory pressure in adults with asthma: a randomized clinical trial. Clin Rehabil. 2018;32(6):752–765. doi: 10.1177/0269215517751587.
- Lin HQ. Effect of progressive relaxation therapy on respiratory function and negative emotion in elderly patients with asthma. Chin Gen Pract Nurs. 2017;15:1985–1986. doi: 10.3969/j.issn.1674-4748.2017.16.027.
- Li HM, Li XB. Influence of respiratory management team on respiratory function recovery and quality of life in elderly patients with asthma. Chin Nurs Res. 2017;31:1897–1899. doi: 10.3969/j.issn.1009-6493.2017.15.034.
- Dong Y. Effect of balloon breathing training on respiratory function in patients with asthma. Lab Med Clinic. 2016;13:2032–2034. doi: 10.3969/j.issn.1672-9455.2016.14.051.
- Raghavendra P, Shetty P, Shetty S, et al. Effect of high-frequency yoga breathing on pulmonary functions in patients with asthma: a randomized clinical trial. Ann Allergy Asthma Immunol. 2016;117(5):550–551. doi: 10.1016/j.anai.2016.08.009.
- Wu CR. Effects of lip contraction and abdominal breathing combined with breathing exercises on lung function and quality of life in patients with asthma. J Clin Res. 2016;33:2025–2027. doi: 10.3969/j.issn.1671-7171.2016.10.052.
- Chen M, Yang G. Analysis of curative effects of exercise on patients with asthma. Acta Acad Med Wannan. 2012;31:458–461. doi: 10.3969/j.issn.1002-0217.2012.06.010.
- Shaw BS, Shaw I. Pulmonary function and abdominal and thoracic kinematic changes following aerobic and inspiratory resistive diaphragmatic breathing training in asthmatics. Lung. 2011;189(2):131–139. doi: 10.1007/s00408-011-9281-8.
- Sodhi C, Singh S, Dandona PK. A study of the effect of yoga training on pulmonary functions in patients with bronchial asthma. Indian J Physiol Pharmacol. 2009;53(2):169–174.
- Vempati R, Bijlani RL, Deepak KK. The efficacy of a comprehensive lifestyle modification programme based on yoga in the management of bronchial asthma: a randomized controlled trial. BMC Pulm Med. 2009;9:37. doi: 10.1186/1471-2466-9-37.
- Arandelović M, Stanković I, Nikolić M. Swimming and persons with mild persistant asthma. ScientificWorldJournal. 2007;7:1182–1188. doi: 10.1100/tsw.2007.221.
- Wen YH, Sun XM, Guo JE. Study on the intervention of relaxation training on patients with bronchial asthma. Chin J Prac Nurs. 2006;22:23–24. doi: 10.3760/cma.j.issn.1672-7088.2006.12.010.
- Farid R, Azad FJ, Atri AE, et al. Effect of aerobic exercise training on pulmonary function and tolerance of activity in asthmatic patients. Iran J Allergy Asthma Immunol. 2005;4(3):133–138.
- Zhang SM, Sun L, Huang JF. Study on effect of relaxation intervention in asthma patients. Chin J Nurs. 1999;34:200.
- Vedanthan PK, Kesavalu LN, Murthy KC, et al. Clinical study of yoga techniques in university students with asthma: a controlled study. Allergy Asthma Proc. 1998;19(1):3–9. doi: 10.2500/108854198778557971.
- Yue CC, Chen X, Sun X, et al. Efficacy of five types of rehabilitation exercise therapies on the exercise capacity intervention in stroke patients: a network meta-analysis. Chin J Evid Based Med. 2022;22:299–308.
- Spruit MA, Singh SJ, Garvey C, et al. An official American thoracic society/european respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13-64–e64. doi: 10.1164/rccm.201309-1634ST.
- Ma LB, Sun JY. Clinical application of respiratory rehabilitation therapy in bronchial asthma. Chin J Preven Cont Chronic Dis. 2020;28:475–479. doi: 10.16386/j.cjpccd.issn.1004-6194.2020.06.018.
- Xing ST, Feng SJ, Zhang YF, et al. A network meta-analysis of the role of different exercises in pulmonary function in children with asthma. J Henan Norm Univ (Nat Sci Ed). 2023;51(02):149–156. doi: 10.16366/j.cnki.1000-2367.2023.02.019.