?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective: To investigate the effect of different bladder filling states on positioning errors in radiotherapy for cervical cancer and obtain the reference range of bladder filling consistency during radiotherapy.
Methods: Patients who underwent postoperative radiotherapy for cervical cancer in Nantong Tumor Hospital from October 2018 to December 2019 were selected. According to the bladder filling deviation, they were divided into group A1 (deviation < 20%) and group B1 (deviation ≥ 20%). The bladder filling variations of the two groups were compared with different positioning errors. Group A2 has a positioning error of <0.4 cm, and group B2 has a positioning error of ≥0.4 cm. The reference range of bladder filling consistency during radiotherapy is obtained by analyzing the composition ratio of different positioning errors of bladder filling deviation.
Results: This study included 195 patients with cervical cancer. The error of longitudinal and vertical position in group B1 was significantly higher than that in group A1 (0.50 ± 0.34 vs. 0.26 ± 0.22 cm, p < 0.001, and 0.22 ± 0.17 vs. 0.16 ± 0.12 cm, p < 0.001). Compared with group B2, the absolute deviation of bladder filling in group A2 (54.1% ± 54.4% vs. 25.6% ± 22.7%, p < 0.001) was slight. The chi-square test showed significant differences in the proportion of the positioning state of different bladder filling forms (χ2 = 31.006, p < 0.001). In addition, there was a significant difference in the proportion of stability errors in patients with poor stability in different directions (χ2 = 118.551, p < 0.001).
Conclusion: In patients with cervical cancer fixed in the supine position, a bladder capacity deviation <20% is easier to achieve excellent positioning with, and it can better control the positioning error of radiotherapy and ensure the positioning accuracy of dose distribution to the target area. It can also achieve good tumor treatment effects. This range can be used as a reference for bladder filling consistency in patients with cervical cancer undergoing radiotherapy.
1. Introduction
Cervical cancer is the most common malignant tumor that affects the female genital tract in China [Citation1]. According to the World Health Organization, there are about 450,000 new cases per year globally. China has more than 130,000 new cases every year, accounting for over a fourth of the world's total patients [Citation2]. While the number of worldwide cervical cancer cases increase annually, 80% of the increase is in developing countries. In addition, 20,000–30,000 women die from cervical cancer each year in China, posing a severe threat to women's health [Citation3]. Radiotherapy is involved in treating 80% of diagnosed patients [Citation4]. Accurate positioning is the key to effective radiation therapy, and it can improve efficiency of radiotherapy and contribute to the treatment of cancer in patients. High repetition position-fixing modes can effectively reduce positioning errors during treatment. The motion of internal tissues and organs is controlled, although the positioning of the patient's body can also reduce positioning errors [Citation5–6]. Through the analysis of postoperative patients with cervical cancer, this study compared the positioning errors of radiotherapy patients in different bladder filling states (different positions and treatment types) to find the appropriate reference range of bladder filling deviation during treatment and achieve the reduction of positioning errors.
2. Materials and methods
2.1. Materials
2.1.1. Clinical data
This study was a retrospective analysis. Post-hysterectomy patients who received postoperative radiotherapy at the Nantong Tumor Hospital from October 2018 to December 2019 were selected. Case inclusion criteria: (1) confirmed postoperative pathological diagnosis; (2) cervical cancer patients with regular bladder morphology in the radiotherapy planning system (TPS); (3) no severe complications and a Karnofsky Scale score of more than 90; and (4) no contraindications to radiotherapy. Exclusion criteria: (1) urinary disorders; (2) treated with radiotherapy and chemotherapy; and (3) severe limb disorders and movement disorders. All patients were reviewed by the Unit Human Ethics Committee. It was approved by the Ethics committee of Nantong Tumor Hospital (number 2017-026). Finally, 195 patients with cervical cancer were included.
2.1.2. Material
Scanning device (Philips, Amsterdam, Holland), Network System (Elekta, Stockholm, Sweden), Planning System (Elekta), Verification System (IBA, Louvain-la-Neuve, Province of walloon Brabant, Belgium), Treatment machine (Elekta), and Position fixing device (Coleridi Medical Equipment Co. LTD, Guangzhou, China).
2.2. Methods
2.2.1. Criteria definition
Bladder filling deviation: The difference in bladder volume in different states of patients. The bladder filling deviation is the difference between the bladder volume at cone-beam computerized tomography (VCBCT) and computerized tomography (VCT) in patients receiving radiotherapy. Bladder filling deviation =
. With a standard treatment and localization bladder filling deviation of 20%, the data were divided into two groups. Patients with an absolute deviation of <20% were placed in group A1, and the patient’s bladder filling state was considered appropriate. Patients with a total deviation of ≥20% were placed in group B1 and supposed to have poor bladder filling status.
Positioning error: The positioning state was distinguished according to the comparison between the positioning error in the treatment process and that in the simulation. Positioning error =
. Taking the positioning error ± 0.4 cm as the standard, the absolute value of any positioning error less than 0.4 cm was recorded as group A2, and the patient was considered to have excellent positioning. The absolute value of any positioning error of ≥0.4 cm was recorded as group B2, and the patient’s position was marked as poor.
2.2.2. Simulation
Molding was performed according to the modified supine fixation technique with a fixed body position [Citation7]. First, all patients evacuated their bladder and rectum before localization. Then, one hour after drinking 500 mL, a CT simulation was performed when the patient reported feeling urinary urgency. The patient was placed supine, fixed with a vacuum pad and taken to be scanned. The scanning range was from the T10 vertebrae to the lower edge of the vaginal introitus. The mold position was repeated. The scan range included the abdomen and pelvic cavity with a 0.5-cm thickness.
2.2.3. Target volume delineation and design planning
The collected CT images were transmitted to the treatment planning system. An experienced radiologist delineated the named target region on the TPS according to the International Committee on Radiological Measurements (ICRU) No. 62 report [Citation8] delineation principles of a target region, combined with the literature [Citation9–11] target region nomenclature and delineation range. Gross tumor volume (GTV), including cervical tumor, uterine body, and pelvic metastatic lymph nodes, was delineated by MRI. The clinical target area (CTV) was drafted by CT images during bladder filling, including regional lymph nodes (common iliac, internal iliac, external iliac, obturator, and presacral lymphatic drainage areas), uterus, parametrium, and upper half of the vagina (the entire vagina was included when the lower third of the vagina was invaded), and the planning target area (PTV) was placed 0.5–1.0 cm above, below, anterior and posterior left and right of the CTV. It was finally confirmed by three persons, including radiologists and physicists. The planned dose was verified (the pass rate standard was 3%; over 3 mm, the pass rate was 95%) and later implemented [Citation12]. Full bladder can reduce the volume of the target area and reduce the volume of small intestine. Full bladder capacity is at least 250 ml, and more urine volume within this range is more advantageous for organ protection [Citation13].
2.2.4. Cone beam CT scan and treatment implementation
The first radiotherapy treatment required a doctor and a physical engineer to work with the therapist for positioning, verification and treatment. Fixed field intensity-modulated radiation therapy was used. The x-ray energy was 6 MV, the total dosage was 50 Gy, and the individual doses were 2 Gy, administered 25 times in total. The radiation field was set to seven areas of irradiation at the angles of 150°, 100°, 50°, 0°, 310°, 260°, and 210° [Citation14]. After confirmation of the treatment plan by the physician in charge, the image data used for the plan was transmitted to the radiotherapy workstation. Before treatment, CBCT was used for image radiation therapy (IGRT) verification, and the bone registration mode was used. Referring to the bones on CT and CBCT, combined with other tissues around the target area, the physician made manual fine-tuning. When the rotation error in any direction is more than 3°, the physician performs repeated positioning and then performs CBCT again. When the linear error in any direction was more than 0.5 cm, the physician adjusted the bed shift according to the CBCT verification results and then performed radiotherapy [Citation15]. The frequency of CBCT was three times before treatment and once a week during treatment.
2.3. Observation indicators
VCT: Bladder contours were obtained by TPS delineation on CT scans, the maximum diameter is measured, and their volumes were obtained after three-dimensional reconstruction. VCBCT: By retrospective analysis of the volume VCT delineated in the bladder in TPS and its relationship with length, width, and height, the approximate volume value VCBCT at treatment was calculated by linear fitting. Error data included three directional linear error values: X-axis (right–left), Y-axis (craniocaudal), and Z-axis (ventrodorsal). In addition, the bladder's length, width, and height were also measured on the CBCT images to compare the effects of different bladder statuses on the radiotherapy setup and different direction setup statuses of cervical cancer.
2.4. Statistical analysis
Data were analyzed and plotted using SPSS 26.0 and OriginPro 9.6.5 software. Linear fitting was selected for the bladder volume estimation formula [Citation16], and the Pearson correlation method was used for correlation analysis. Data are presented as mean ± standard deviation X ± SD). An independent sample t-test was used to make comparisons between the two groups. In addition, the chi-square test was used to compare the constituent ratios. p < 0.05 Indicated a significant difference.
3. Results
3.1. Clinical data
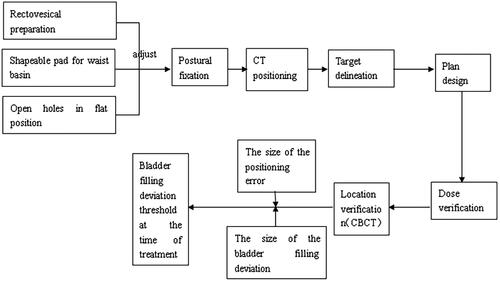
After the inclusion and exclusion criteria were applied, 195 post-operative patients with cervical cancer were included who ranged in age from 24 to 86 years old, with a mean age of 59.8 (see for the design flow of this study).
3.2. Linear fitting of the bladder volume
Equation (1) was obtained through linear fitting based on the TPS's bladder volume and length, width and height. The bladder volume (VCBCT) in the CBCT images was calculated with the fitting formula, thus obtaining the filling deviation from the bladder volume (VCT) in the CT localization image.
As shown in the , the length, width, and height (three axial lengths) of the bladder were measured. The filled bladder presented an ellipsoidal shape, but there were slight individual differences, so the volume of the filled bladder could not be calculated solely based on the ellipsoidal volume formula. By combining the ellipsoidal volume formula V = 4/3πabc (where abc represents the product of the three semi-axis lengths of the ellipsoid), it was observed that the volume V exhibited a linear relationship with the product of the three semi-axis lengths (abc). Therefore, a linear fitting of a large amount of data of the filled bladder was used to obtain the linear relationship between the bladder volume and the product of the bladder's length, width, and height (the three axial lengths). The Equation (1) is as follows: y = 17.58 + 0.56 * x (r = 0.988, y= bladder volume, x = product of length, width, and height). The calculated bladder volumes were as follows: VCT was 272.20 ± 160.3 mL (range: 27–983 mL), and VCBCT was 252.51 ± 172.29 mL (range: 18–889 mL) (See for the linear correlation between bladder filling and positioning in this study).
Figure 2. Schematic diagram of measuring the length, width and height of the bladder (three axial lengths).
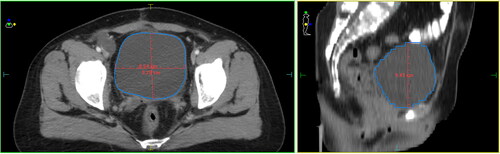
Figure 3. Linear correlation between bladder filling and positioning. The X-axis is the pendulum error value, and the Y-axis indicates the number of cases corresponding to a certain error. Three lines are shown, respectively: green Rt-Lt is the horizontal direction (Right-Left); red Sup-Inf is the longitudinal direction (Superior-Inferior); and blue Ant-Post is the vertical (Anterior-Posterior) direction.

3.3. Comparison of setup errors of different bladder filling deviations
The absolute deviation between VCBCT and VCT ranged from 0.87% to 285.55%, with nearly half of the patients (89 out of 195) having a bladder volume deviation within 20%. The error in group B1 was significantly higher than that in group A1 in the Y-axis (0.50 ± 0.34 vs. 0.26 ± 0.22, t = −6.012, p < 0.001) and Z-axis positions (0.22 ± 0.17 vs. 0.16 ± 0.12, t = −3.055, p < 0.001). These findings are shown in .
Table 1. Positioning error under different bladder filling deviations (x- ± s, cm).
3.4. Comparison of bladder filling deviation under different setup errors
The absolute deviation of bladder filling was smaller in A2 compared with B2 (25.6 ± 22.7 vs. 54.1 ± 54.4, t = − 4.729, p < 0.001). These findings are shown in .
Table 2. Bladder filling deviation with different positioning errors (x- ± s, %).
3.5. Composition of the proportion of different positioning states with different bladder filling states
A chi-square test showed significant differences in the proportion of positioning states with different bladder filling states (χ2 = 31.006, p < 0.001). The ratio of excellent positioning status with suitable bladder filling status reached 73.03%, the ratio of poor positioning status with suitable bladder filling status was 26.97%, the ratio of excellent positioning status with subpar bladder filling status was 33.02%, and the ratio of poor positioning status with subpar bladder filling status was 66.98%. This is shown in .
Table 3. Different positioning states with different bladder filling deviations.
3.6. Composition the proportion of setup errors in different directions of patients with inferior positioning states
Ninety-five of the 195 patients had poor positioning statuses (counting the positioning statuses in the X, Y, and Z axis). The chi-square test showed significant differences in the proportion of different positioning error directions between patients with poor positioning status (χ2 = 118.551, p < 0.001). The proportion of excellent positioning status in Rt – Lt direction reached 87.37%, the proportion of poor positioning status in Rt – Lt direction was 12.63%, the proportion of excellent positioning status in craniocaudal direction was 16.84%, the proportion of poor positioning status in craniocaudal direction reached 83.16%, the proportion of excellent positioning status in ventrodorsal direction reached 78.95%, the proportion of poor positioning status in ventrodorsal direction was 21.05%. This is shown in .
Table 4. The positioning error of patients with inferior positioning status in different directions.
4. Discussion
Positioning is vital in radiation therapy for patients; the choice of position can alter the external contours of the treated area and has the potential to alter the spatial relationships between the internal organs. The setup aims to achieve an optimal geometric position, thus improving the reproducibility and accuracy of treatment as much as possible. However, changes in the patient's physiological status and the presence of tissues (muscle, fat, intestines, and the bladder) makes it challenging to maintain the reproducibility of each position. Therefore more precise radiotherapy, such as IGRT, is currently used for tumor treatment. In IGRT, position verification is done before radiation treatment starts, using an immediate response with indicators to move the treatment bed to correct the patient's position; radiotherapy is then performed after position confirmation [Citation17]. However, CBCT and Electronic Portal Imaging Devices (EPID) have noticeable shortcomings. For example, the patient is subjected to an additional radiation dose, and the soft tissue contrast is poor. 12–18% of gynecological and prostate CBCT images are reported to be of poor quality for soft tissue visualization [Citation18–23]. CBCT is non-invasive and improves patient comfort.
In general, head and neck tumor radiotherapies require a fractional order repeat accuracy of ±0.3 cm, and pelvic tumor localization accuracy is poor, so it is relaxed to ±0.5 cm. There are fewer apparent bone markers, thick subcutaneous fat, relatively sizable mobility, multiple internal organs and a large amount of deformation in cervical cancer patients, leading to a large position deviation at each radiotherapy session. This is especially true with the differences in bladder filling status in patients with supine fixations. The bladder filling differences negatively affect the dose [Citation24] and lead to changes in patient setup errors. However, to date, there has not been much research on this. Different filling degrees of the bladder can make a difference in the dose and extent of the radiation therapy received by patients. This is completed by moving the treatment bed to correct an immediate response of the patient's position, followed by radiotherapy after position confirmation. For patients with little visceral fat, the position of organs can change with bladder filling status, which has a significant impact on localization errors. Zhou et al. [Citation25] used a digital simulator to verify the positional movement of patients with cervical cancer in different bladder volume states and found that the positioning of patients was highly repeated in the bladder filling form. Klein et al. [Citation26] compared the positioning errors of cervical cancer patients in different bladder serving forms and found that the linear errors in the X and Y axis in the bladder filling state were significantly smaller than those in the empty state. To improve the accuracy of patient positioning, it is recommended that the bladder status of the relative positioning for radiotherapy implementation is the same. In a study by Gonzalez et al. [Citation27], one group of patients suppressed their urine for radiotherapy while the other group underwent radiotherapy after measuring the localization volume. The results demonstrated that the linear error in the craniocaudal direction was smaller in the observation group than in the control group. This confirms that greater bladder filling consistency can result in better fixation positions, facilitating the achievement of more precise radiotherapy. Another study showed that patients with cervical cancer had smaller bladder volumes and an extensive range of fluctuations compared to CT simulation localization. The position of the bladder center varies significantly in the Y axis, and shape consistency needs to be improved [Citation28].
Patients with cervical cancer who received postoperative radiotherapy were included in this study. To minimize the impact of other uncertainties, bladder filling statuses and placement outcomes were monitored at the first session. Since only length measurement tools are available in the X-ray volumetric imaging system, the bladder volume cannot be delineated directly. Therefore, the formula for estimating bladder volume was obtained by linearly fitting the bladder volume in TPS to the product of bladder length, width and height. The results showed that for normal bladders, the filling volume was highly linear with the product of its length, width and height, so the bladder volume in CBCT images could be quickly calculated by Equation (1), and 20% was taken as the cut-off value for group analysis based on the distribution value of bladder volume deviation in postoperative patients. The results showed that the deviation of bladder volume during treatment was smaller than that of the setup (<20%), resulting in relatively less movement of the lower abdominal tissue. This resulted in a decrease in lower abdominal marker lines and marker points, which made the positioning error smaller than that of patients with larger bladder volume deviations. In contrast, patients with relatively small positioning errors (<0.4 cm in all directions) during treatment had smaller bladder volume deviations. This is because the lower abdominal marker lines of patients with high bladder repetition overlap well, suggesting that one of the sources of setup error is the difference in bladder filling. Then, 0.4 cm was used as the boundary to distinguish the localization states and analyze the composition ratio of different states. The results showed that when the bladder filling deviation was small (<20%), it was easier to obtain a better positioning state (73.03%). From the analysis of localization statuses in three directions, the main direction of lower localization errors caused by bladder filling deviation was along the Y axis (83.16%).
During this experiment, patients were asked to empty their bladders. Then, they were prepped and put in position and a CT scan was performed. However, a systematic error in the experiment resulted because the bladder cannot be completely emptied (due to physiological characteristics, 10–20 mL of urine remains). Furthermore, in selecting subjects, the sample size was insufficient, and there were differences between the individuals. There was not follow-up recurrence data, and the effect of bladder filling status on local recurrence was not explored. In addition, this study did not focus on the influence of the patients' rectal status on the CTV, which may have had an effect. A more systematic and in-depth study to confirm the results of this study will be performed in the future.
5. Conclusion
In conclusion, for patients with cervical cancer fixed in the supine position, a highly reproducible bladder capacity (deviation <20%) is more likely to achieve an excellent positional status (deviation <0.4 cm), which can better control the setup errors of radiotherapy, especially in the craniocaudal direction. Therefore, the positional accuracy of the dose distribution in the target area is ensured, and effective tumor treatment is achieved. While guaranteeing the therapeutic effect, the dose of normal tissue in the filling and emptying state of the bladder is studied to find a better treatment plan for the patient and obtain the more significant benefits. The results of this study can provide a reference for the consistency of bladder filling in patients with cervical cancer undergoing radiotherapy.
Authors contributions
Study conception and design: Bin-Bin Ge, Yu Liu, Jian-Hua Jin; Data collection: Jian-Ting Wu, Hai-Tao Liu. Data analysis and interpretation: Chen-Yun He, Yong-Liang Zhao, Gu-Fei Cao. Drafting of the article: Xiao-Gang Zhai, Kai-Yue Chu, Jun-Hui Wang. Critical revision of the article: Bin-Bin Ge, Yu Liu, Jian-Hua Jin, Jian-Ting Wu, Hai-Tao Liu, Chen-Yun He, Yong-Liang Zhao, Gu-Fei Cao, Xiao-Gang Zhai, Kai-Yue Chu, Jun-Hui Wang.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Nantong Tumor Hospital, The Affiliated Tumor Hospital of Nantong University (Approval No.2017-026). We obtained signed informed consent from the participants in this study.
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data availability statement
The data supporting the findings of this study are available within the article.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Li DJ, Shi J, Jin J, et al. Epidemiological trend of cervical cancer. Zhonghua Zhong Liu Za Zhi. 2021;43(9):1–8. PMID: 34530572. doi: 10.3760/cma.j.cn112152-20190904-00573.
- Han R, Wu M, Chen W, et al. Analysis on incidence and mortality of prostate cancer in China 2003–2007. China Cancer. 2012;21(11):805–811. doi: 10.11735/j.issn.1004-0242.2012.11.A002.
- Liu ZC, Li ZX, Zhang Y, et al. Interpretation on the report of Global Cancer Statistics 2020. J Multidisciplinary Cancer Manage (Electronic Version). 2021;7(02):1–14. doi: 10.12151/JMCM.2021.02-01.
- Li YX. Oncology radiotherapy. 5th ed. Beijing: Peking Union Medical College Press; 2018. p. 1371–1419.
- Wu WC, Chang YR, Lai YL, et al. Impact of body-mass factors on setup displacement during pelvic irradiation in patients with lower abdominal cancer. Radiol Oncol. 2019;53(2):256–264. doi: 10.2478/raon-2019-0017.
- An F, Wang S, Wang ZQ, et al. Analysis of lower urinary tract symptoms and related factors following radical hysterectomy for cervical cancer#br#. Chin J Clin Obstetr Gynecol. 2021;22(4):398–401. doi: 10.13390/j.issn.1672-1861.2021.04.017.
- Li X, Chen Y. Comparison of effects of thermoplastic film fixation in intensity modulated radiotherapy for cervical cancer with different postures. J Clin Med. 2017;4(27):5213–5214. doi: 10.3877/j.issn.2095-8242.2017.27.048.
- Taylor LS. Report of the international commission on radiological units and measurements (ICRU). Radiology. 1960;74(1):115–116. doi: 10.1148/74.1.115.
- Chen JW, Liu P, Chen WJ, et al. A study of changes in volume and location of target and organs at risk in intensity-modulated radiotherapy of cervical cancer. Chin J Radiat Oncol. 2015;24(4):395–399. doi: 10.03760/cam.j.issn.1004-4221.2015.04.010.
- Stroom JC, Heijmen BJ. Geometrical uncertainties, radiotherapy planning margins, and the ICRU-62 report. Radiother Oncol. 2002;64(1):75–83. doi: 10.1016/s0167-8140(02)00140-8.
- Liu Y, Yu J, Qian L, et al. Extended field intensity-modulated radiotherapy plus concurrent nedaplatin treatment in cervical cancer. Oncol Lett. 2016;11(5):3421–3427. doi: 10.3892/ol.2016.4416.
- Wang D, Bosch W, Kirsch DG, et al. Variation in the gross tumor volume and clinical target volume for preoperative radiotherapy of primary large high-grade soft tissue sarcoma of the extremity among RTOG sarcoma radiation oncologists. Int J Radiat Oncol Biol Phys. 2011;81(5):e775-80–e780. doi: 10.1016/j.ijrobp.2010.11.033.
- Ge BB, Wang JH, Wu JT, et al. Effect of different bladder filling on dose in cervical cancer radiotherapy. Biomed Engng Clinical Med. 2021;25(05):569–574. doi: 10.13339/j.cnki.sglc.20210820.020.
- Chino J, Annunziata CM, Beriwal S, et al. Radiation therapy for cervical cancer: executive summary of an ASTRO clinical practice guideline. Pract Radiat Oncol. 2020;10(4):220–234. doi: 10.1016/j.prro.2020.04.002.
- Wu JY, Wei HR. The application of cone beam CT in the setting error analysis of radiotherapy for cervical cancer and its influencing factors. J Med Imag. 2018;28(01):167–169.
- Lin Y, Dong P, Shi D, et al. Clinical values of transrectal ultrasound in judging GTV of cervical cancer. Brachytherapy. 2021;20(6):1172–1179. doi: 10.1016/j.brachy.2021.07.007.
- Rigaud B, Anderson BM, Yu ZH, et al. Automatic segmentation using deep learning to enable online dose optimization during adaptive radiation therapy of cervical cancer. Int J Radiat Oncol Biol Phys. 2021;109(4):1096–1110. doi: 10.1016/j.ijrobp.2020.10.038.
- Small WJr, Bosch WR, Harkenrider MM, et al. NRG oncology/RTOG consensus guidelines for delineation of clinical target volume for intensity modulated pelvic radiation therapy in postoperative treatment of endometrial and cervical cancer: an update. Int J Radiat Oncol Biol Phys. 2021;109(2):413–424. doi: 10.1016/j.ijrobp.2020.08.061.
- Glaser SM, Mohindra P, Mahantshetty U, et al. Complications of intracavitary brachytherapy for gynecologic cancers and their management: a comprehensive review. Brachytherapy. 2021;20(5):984–994. doi: 10.1016/j.brachy.2020.11.011.
- Weinstein R, Parikh-Das AM, Salonga R, et al. A systematic assessment of the epidemiologic literature regarding an association between acetaminophen exposure and cancer. Regul Toxicol Pharmacol. 2021;127:105043. doi: 10.1016/j.yrtph.2021.105043.
- Corral de la Calle MÁ, Encinas de la Iglesia J. Ultrasonography in infectious and neoplastic diseases of the bowel and peritoneum. Radiologia (Engl Ed). 2021;63(3):270–290. doi: 10.1016/j.rx.2020.12.004.
- Singh A, Singh S, Mani KR, et al. Comparing setup errors using portal imaging in patients with gynecologic cancers by two methods of alignment. J Med Imag Radiat Sci. 2020;51(3):394–403. doi: 10.1016/j.jmir.2020.04.001.
- Tsuboyama T, Takei O, Okada A, et al. Effect of uterine position and intrapelvic motions on the image quality of 3D T2-weighted MRI of the uterus: can short prescans predict the non-diagnostic image quality? Eur J Radiol. 2020;130:109186. doi: 10.1016/j.ejrad.2020.109186.
- Mosca L, Ilari A, Fazi F, et al. Taxanes in cancer treatment: activity, chemoresistance and its overcoming. Drug Resist Updat. 2021;54:100742. doi: 10.1016/j.drup.2020.100742.
- Zhou XB, Xu SW, Ye LP, et al. Progress of esophageal stricture prevention after endoscopic submucosal dissection by regenerative medicine and tissue engineering. Regen Ther. 2021;17:51–60. doi: 10.1016/j.reth.2021.01.003.
- Klein GT, Ajay D, Volk RJ, et al. Living with urinary diversions: patient insights to improve the perioperative experience. Urology. 2021;152:190–194. doi: 10.1016/j.urology.2021.01.009.
- Gonzalez Y, Shen C, Jung H, et al. Semi-automatic sigmoid Colon segmentation in CT for radiation therapy treatment planning via an iterative 2.5-D deep learning approach. Med Image Anal. 2021;68:101896. doi: 10.1016/j.media.2020.101896.
- Buijs M, Bloemers MCWM, Remeijer P. Impact of a fiducial marker based ART strategy on margins in postoperative IMRT of gynecological tumors. Radiother Oncol. 2021;158:1–6. doi: 10.1016/j.radonc.2021.01.039.