Abstract
Objective
To investigate the differences in the viscoelastic properties between normal trapezius muscles and those in patients with trapezius myofascial pain syndrome (MPS) using real-time shear-wave elastography (SWE).
Materials and Methods
This study included 31 patients with trapezius MPS and 31 volunteers. Sixty-one trapezius muscles (41 and 20 on the affected and non-affected side, respectively) of patients with MPS and 62 normal trapezius muscles in volunteers were assessed. Conventional ultrasonic parameters, including skeletal muscle thickness, resistance index (RI), and mean shear wave velocity (SWVmean) of trapezius muscles, were obtained in the seated position with the shoulders and neck relaxed. The daily neck leaning time (unit:hours) of all participants was obtained using a questionnaire.
Results
Ultrasound showed no statistically significant differences in thickness or RI of the trapezius muscles of the affected and non-affected sides in MPS patients versus normal trapezius muscles (p = 0.976 and 0.106, respectively). In contrast, the SWVmean of trapezius muscles in patients with MPS was significantly higher than that of normal trapezius muscles in both the affected and non-affected sides (4.41 ± 1.02 m/s vs. 3.35 ± 0.79 m/s, p < 0.001; 4.05 ± 0.63 m/s vs. 3.35 ± 0.79 m/s, p = 0.002). There was no significant difference between the SWVmean of the trapezius muscles on the affected and non-affected sides in patients with MPS (4.41 ± 1.02 m/s vs. 4.05 ± 0.63 m/s, p = 0.225). Correlation analysis showed that daily neck forward time was positively correlated with the SWVmean of the trapezius muscles on the affected and non-affected sides in patients with MPS (r = 0.635, p < 0.001; r = 0.576, p = 0.008).
Conclusion
SWE can quantitatively evaluate stiffness of trapezius muscles in patients with trapezius MPS. The stiffness of both affected and non-affected trapezius muscles increased in patients with trapezius MPS, and the degree of increase positively correlated with the time of cervical forward leaning.
Introduction
Myofascial pain syndrome (MPS) is a pain syndrome caused by skeletal muscle strain, the main symptoms of which are pain, stiffness, dysfunction, and other symptoms caused by myofascial trigger points (MTrPs) in skeletal muscle [Citation1]. MTrPs typically occur on the trunk, most commonly in the shoulders and neck, and do not develop in the arms or legs. These MTrPs predominantly affect the trapezius muscle, especially the superior trapezius muscle; moreover, the maximum amount of MTrPs in the human body occur in the upper trapezius muscle [Citation1,Citation2]. MPS is the most common cause of chronic pain [Citation1,Citation3]. Chronic pain affects approximately 100 million adults in the United States, and is associated with an annual cost of $560 to $635 billion [Citation3].
Historically, MPS was often ignored by people as they considered the pain caused by MPS to be less serious than that caused by fracture, angina pectoris, and other diseases. However, patients with myofascial pain reported visual analog scale ratings of pain equivalent to or higher than pain due to other causes [Citation1,Citation2,Citation4]. Currently, no laboratory tests or imaging modalities (such as magnetic resonance imaging [MRI], computed tomography [CT], or radiography) can detect MTrPs in skeletal muscle for diagnosing MPS. Instead, MPS is typically identified by feeling knots in the muscles or small areas of muscle spasm within a taut or tense band of muscle, which are tender, and cause referred pain that can then be treated [Citation5]. At present, the diagnosis of MPS mainly relies on palpation by clinicians. This method has poor reliability and is easily affected by differences in clinical experience and patient perception [Citation1,Citation5]. In addition, for patients with preclinical MPS, because they have no positive symptoms of skeletal muscle pain, spasm, dysfunction, among others, doctors cannot detect the preclinical lesions of the skeletal muscle by palpation of the pain stimulation points; therefore, detection and accurate diagnosis of MPS in the early stage currently poses the greatest challenge for doctors.
Studies have found that the generation of MTrPs in skeletal muscle is closely related to fatigue and relaxation delay or disappearance after lasting tense contraction and spasms [Citation1,Citation5]. Therefore, skeletal muscle fatigue is the main early injury in MPS, manifesting as delayed or absent skeletal muscle relaxation [Citation1,Citation5–7]. There are no morphological changes in the affected skeletal muscles during fatigue injury; therefore, routine imaging is usually not positive [Citation1,Citation5]. According to the 2018 EFSUMB guidelines for the clinical practice of elastography in non-hepatic applications, skeletal muscle pathologies alter the passive elastic properties of skeletal muscles. Therefore, assessment of muscle stiffness has an important reference value for the diagnosis of skeletal muscle diseases [Citation8]. This study aimed to investigate the differences in viscoelastic properties between normal and trapezius MPS, using real-time shear-wave elastography (SWE) to evaluate characteristics of muscle stiffness in trapezius MPS.
Materials and methods
Participants
This study was approved by the Ethical Review Committee of the Third Hospital of Shanxi Medical University (Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, and Tongji Shanxi Hospital, China). None of the authors received any specific support from any industry for this study. All patients and volunteers were enrolled between November 2020 and August 2021, and provided written permission for the anonymous use of their medical data for scientific purposes before the imaging examinations.
The inclusion criteria for volunteers were as follows: age: 20–45 years old, body mass index (BMI): 18.5–23.9, right hand dominance, no pain on both sides of shoulder and neck, and written informed consent. The exclusion criteria for volunteers were pregnancy; history of shoulder and neck diseases, trauma, surgery, and radiotherapy; history of primary muscle disease; history of systemic, metabolic, or endocrine diseases; psoriasis; and treatment with corticosteroids, estrogens, quinolones, and cholesterol drugs because of known associations between these factors and skeletal muscle disease.
The inclusion criteria for MPS patients were: age 20–45 years, BMI 18.5–23.9, right-hand dominance, referral for shoulder and neck pain, and confirmed diagnosis of trapezius MPS. Trapezius MPS was diagnosed by two clinicians with more than 10 years of experience using the widely adopted criteria proposed by Simons et al. The major criteria include: (I) palpable taut band (if muscle is accessible); (II) exquisite spot tenderness of a palpable nodule in a taut band; (III) the patient reports concurrent pain after pressure is applied on the tender nodule (for active MTrPs); and (IV) painful limit to full stretch range of motion [Citation1]. All MPS patients met these diagnostic criteria, while healthy volunteers did not. Other neck pain disorders in all subjects were ruled out through diagnostic tests such as imaging. The exclusion criteria for patients were the same as those for healthy volunteers [Citation9,Citation10].
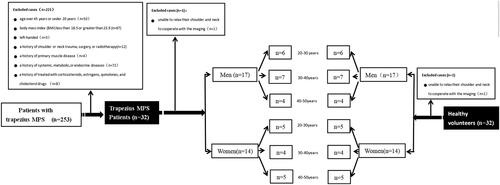
Based on the above exclusion criteria, 32 patients with MPS were included in this study (15 females and 17 males). Men and women were then assigned to the following age groups: 20–30 years old, 30–40 years old, and 40–50 years old. The volunteers were matched for each subgroup at a 1:1 ratio of volunteers to patients, and 32 volunteers were included in this study ().
Procedure
Ultrasound images of the trapezius muscle were collected by two ultrasonographers with more than 10 years of experience, who were blinded to shoulder and neck pain and other clinical information. The Supersonic Imagine AixPlore real-time ultrasonic shear wave elastic imaging diagnostic instrument (Supersonic Imagine, Aix-en-Provence, France), with an L10-2 linear array probe and a probe frequency of 2–10 MHz, was used in this study. All participants were seated and fully exposed to the shoulder and neck, with their forearms relaxed and their palms facing upward on the ipsilateral thigh (). The midpoints of the line between the foramen magnum and left or right acromion were selected as measurement points of the trapezius muscle on both sides () [Citation7]. This measurement point is one of the sites most prone to the occurrence of pain trigger points [Citation1]; all subjects in this study had explicit or implicit pain trigger points at this location. A thick coupler and probe were positioned at the measuring point. During examination, the probe was kept perpendicular to the skin's surface and gently released without pressure [Citation8,Citation11,Citation12]. The orientation of the probe was adjusted so that it was perpendicular to the long axis of the abdomen of the trapezius muscle, the transverse section of the trapezius muscle was obtained, and the thickness was measured (). To obtain a longitudinal section of the trapezius muscle, the probe was rotated 90° counterclockwise such that the probe direction was parallel to the long axis of the body of the trapezius muscle. The resistance index (RI) was investigated using Doppler ultrasonography () [Citation13–15]. Finally, we selected the SWE mode, maintained probe direction parallel to the long axis of the trapezius muscle, and placed the region of interest (ROI) in the middle of the image to cover the trapezius muscle. The ROI was uniformly set to a square area measuring 2.0 cm × 3.0 cm [Citation12,Citation16–20]. The image was frozen after it was stable and Q-BOX, which is set as a circle with a diameter of 5 mm. was initiated. The system then automatically calculated the elastic parameters of the trapezius muscle: the mean shear wave velocity [SWVmean] (m/s) (). The above parameters were measured three times, and the average value was used for statistical analysis.
Figure 2. (a) The participants were seated, fully exposed to the shoulder and neck, with their forearms relaxed and palms facing upward on the same thigh. (b) The midpoints of the line between foramen magnum and left or right acromion were selected as the image Collection points of trapezius muscle on both sides.
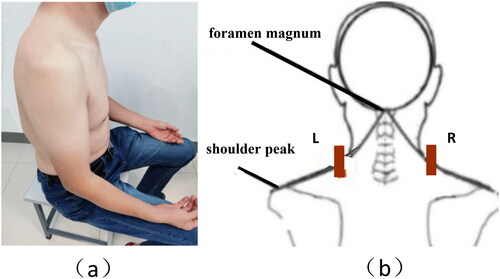
Figure 3. (a) Transverse section and longitudinal section of trapezius muscle; (b) Mean shear-wave propagation velocity (SWVmean [m/s]) of the trapezius muscle. *traps, trapezius; LS, levator scapularis muscle.
![Figure 3. (a) Transverse section and longitudinal section of trapezius muscle; (b) Mean shear-wave propagation velocity (SWVmean [m/s]) of the trapezius muscle. *traps, trapezius; LS, levator scapularis muscle.](/cms/asset/e9730cf0-22ff-4b01-bc99-539a23f8eef9/iann_a_2252442_f0003_c.jpg)
The daily neck-leaning time (hours) of all patients and volunteers was obtained using a questionnaire. The daily neck forward time was taken as the average of the daily neck forward time over the last three months, which was mainly composed of daily mobile phone screen time, daily computer operating time, and other neck forward times. The participants selected appropriate time periods (<3 h, 3–6 h, 6–9 h, >9 h) according to their situation over the last three months.
During image acquisition, one patient with unilateral MPS and one volunteer could not relax their shoulder and neck muscles for image acquisition, and the image transmission of the right trapezius muscle of one patient with bilateral MPS was incomplete. Finally, 31 MPS patients (41 and 20 trapezius on the affected and non-affected side in patients with MPS, respectively) and 31 volunteers (62 normal trapezius muscles) were included in this study.
Intra-observer and inter-observer reproducibility
Ultrasonic elasticity image acquisition and analysis of the trapezius muscle were repeated in 10 randomly selected participants. Intra-observer reliability assessments were performed 5 days apart by the same observer on the same participants. The assessment of inter-observer reproducibility was performed by another independent observer.
Statistical analysis
All data were analyzed using SPSS statistical software (SPSS for Windows, version 22.0; IBM, Armonk, NY, USA) and MedCalc software (MedCalc for Windows, version 19.6.4; MedCalc Software, Mariakerke, Belgium). Continuous variables were expressed as means and standard deviations. The Shapiro–Wilk test was used to analyze the normality of the distributions. Levene's test was used to analyze the variance homogeneity of the measurement data in each group. Differences between the affected and unaffected sides in patients with MPS and volunteers with normal trapezius were analyzed using analysis of variance (ANOVA) or Kruskal–Wallis H tests. Spearman's rank correlation coefficient was used to analyze the correlation between trapezius SWVmean and daily neck-leaning time. P values were two-sided and were used only for the primary endpoint. Statistical significance was set at p < 0.05.
Bland–Altman plots were used to compare SWE measurements of the 10 participants that were recorded by the same two investigators and observer as those mentioned above. The intraclass correlation coefficient (ICC) was used to evaluate inter- and intra-observer variabilities.
Results
Population
A total of 31 volunteers (62 normal trapezius muscles) and 31 patients were included. Among the patients, 20 had unilateral and 11 had bilateral trapezius MPS; all diagnoses were confirmed according to the four essential criteria proposed by Simons et al. Each trapezius muscle was considered separately. Due to incomplete right image transmission in one patient with bilateral trapezius MPS, 41 trapezius muscles (the trapezius of the affected side in 20 patients with unilateral MPS and 11 patients with bilateral MPS) were included in the affected-side MPS groups, and 20 trapezius muscles (the trapezius of the non-affected side in 20 patients with unilateral MPS) were included in the non-affected-side MPS groups.
lists the basic data of patients with MPS and volunteers, and includes the clinical characteristics of patients with MPS. The patients with trapezius MPS included 17 males and 14 females, aged 20–44 years, with a mean age of 31.03 ± 6.27 years. The volunteers included 17 males and 14 females, aged 20–44 years with an average age of 31.45–5.88 years. There were no significant differences in sex, age, and body mass index (BMI) between the two groups (all p > 0.05). There were 0, 8, 12, and 11 patients with MPS; and 3, 16, 8, and 4 cases in the volunteers, who reported daily neck forward times of 1–3 h, 3–6 h, 6–9 h, and >9 h, respectively; the difference was not statistically significant (p = 0.016).
Table 1. Basic clinical data of MPS patients and volunteers.
Inter- and intra-observer variability
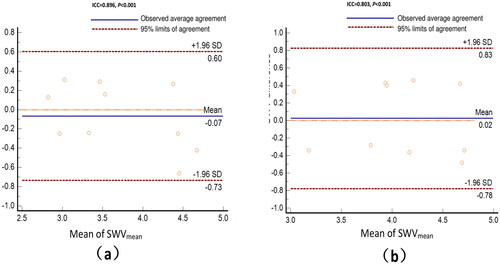
Bland–Altman agreement plots for the trapezius SWVmean are shown in (one observer) and (two observers). The ICCs for inter- and intra-observer reproducibility were 0.803 (95% CI, 0.375–0.947; p = 0.001) and 0.896 (95% CI, 0.646–0.973; p < 0.001), respectively, indicating good reproducibility for both.
Figure 4. (a) Bland–altman plots of SWVmean measurements by the same observer on the same participants in a random order performed 5 days apart; (b) Bland–altman plots of SWVmean measurements by two observers. Plots represent the difference between observers' and mean measurements. The top and bottom lines show the 95% limits of the agreement; the middle line shows the mean difference. *ICC: intraclass correlation coefficient; SD; standard deviation.
Ultrasound
There was no significant difference in trapezius muscle thickness and RI between the MPS-affected side (n = 41), non-affected side (n = 20), and normal trapezius muscles (n = 62) (p = 0.976 and 0.106, respectively) ().
Table 2. Comparison of conventional ultrasound parameters and SWVmean of trapezius muscle between the affected and the non-affected sides in MPS patients、normal trapezius in volunteers.
Elastography
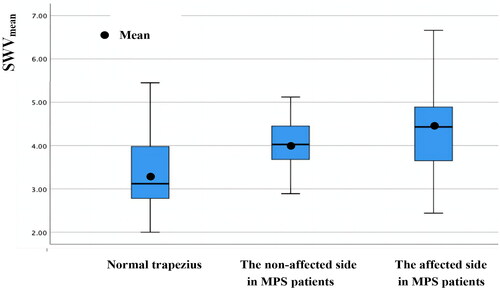
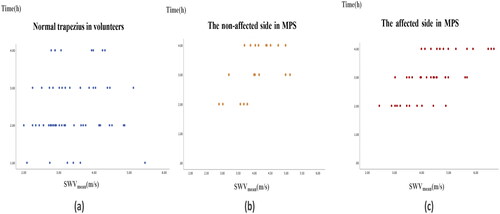
The SWVmean of the trapezius on the affected and non-affected side in MPS patients was significantly higher than that of the normal trapezius muscles in volunteers (4.41 ± 1.02 m/s vs. 3.35 ± 0.79 m/s, p < 0.001; 4.05 ± 0.63 m/s vs. 3.35 ± 0.79 m/s, p = 0.002), and the difference between groups was 1.06 m/s (95% CI:0.71–1.39 m/s) and 0.70 m/s (95% CI:0.77–1.13 m/s), respectively. There was no significant difference between the SWVmean of the trapezius on the affected and non-affected side in MPS patients (4.41 ± 1.02 m/s vs. 4.05 ± 0.63 m/s, p = 0.225) (, ).
Figure 5. Box diagram of the SWVmean of trapezius in volunteers, the affected and non-affected sides in MPS patients. The SWVmean of trapezius on the affected and non-affected sides in MPS patients was significantly higher than that of normal trapezius in volunteers. However,there was no significant difference between the SWVmean of trapezius on the affected and non-affected sides in MPS patients.
Correlation analysis
Daily neck forward time was positively correlated with the SWVmean of the trapezius muscles on the affected and non-affected sides in patients with MPS (). The correlation coefficients were 0.635(95% CI: 0.405–0.801, p < 0.001), 0.576 (95% CI: 0.085–0.816, p = 0.008), respectively. Daily neck forward time was not significantly correlated with the SWVmean of the normal trapezius muscle in volunteers (correlation coefficient = 0.154 [95% CI: −0.096–0.392, p = 0.232]).
Figure 6. Correlation analysis between SWVmean of trapezius muscles and the daily neck forward time. (a) The daily neck leaning time was strongly correlated with SWVmean of the trapezius muscles on both the affected and non-affected sides in patients with trapezius MPS (r = 0.635, 95% CI: 0.405-0.801, p < 0.001; r = 0.576, 95% CI: 0.085-0.816, p = 0.008). (b) The daily neck forward time was weakly correlated with the SWVmean of normal trapezius muscles in volunteers (r = 0.154, 95% CI: −0.096–0.392, p = 0.232).
Discussion
Musculoskeletal soreness and pain are ubiquitous and cause great human suffering. However, MPS, which is one of the leading causes of this type of pain, is often overlooked and misunderstood. Physicians commonly overlook this condition because of a lack of awareness and training, although it is a relatively simple diagnosis [Citation1–5, Citation21]. However, as there are no morphological changes in MPS-affected muscles and no positive findings in conventional imaging and laboratory tests, the diagnosis of MPS is still mainly based on clinical diagnosis, which relies on doctors' palpation experience of skeletal muscle pain points and patients' subjective symptoms, with poor reliability [Citation1,Citation22]. This study aimed to quantify the differences in trapezius muscle stiffness between normal volunteers and MPS patients, and to evaluate muscle stiffness characteristics in trapezius MPS using SWE.
The change in tissue stiffness is an important feature in the evaluation of human soft tissue and organ lesions, such as inflammation and cancer, both of which can lead to changes in tissue stiffness [Citation12]. Real-time shear wave ultrasonic elastic imaging technology can be used as a powerful tool to quantify tissue stiffness. It has been proven to provide diagnostic information for tumor diagnosis by evaluating the elastic changes in diseased tissues and has been widely used in the diagnosis of diseases in the thyroid, breast, liver, and other organs [Citation12,Citation21–24]. However, the assessment of skeletal muscle diseases using this technology is still in its infancy [Citation25–27]. Studies have found that due to the extensive use of electronic devices, remaining in the forward head posture for long periods of time leads to abnormal discharge at the motor endplate. This causes muscle fiber dysfunction and the release of catecholamines [Citation1,Citation14] In turn, this results in skeletal muscle pain and fatigue and interferes with normal skeletal muscle function, leading to delayed relaxation and increased muscle tension [Citation1,Citation5,Citation6,Citation14,Citation28,Citation29]. Therefore, changes in stiffness of affected muscles in patients with cervical MPS are closely related to occurrence and development of the disease [Citation14,Citation28]. In this study, muscle stiffness in the trapezius muscles of patients with MPS was significantly higher than that in the trapezius muscles of volunteers. In addition, trapezius muscle stiffness on the unaffected side in patients with unilateral MPS was significantly higher than that of normal trapezius muscles in volunteers. In patients with unilateral trapezius MPS, the contralateral asymptomatic trapezius muscle also exhibits elastic changes and increased stiffness. Therefore, trapezius stiffness measurements by SWE may have potential clinical value for early detection and diagnosis of asymptomatic subclinical MPS. Therefore, quantifying muscle stiffness may have potential diagnostic value for MPS, and requires further study.
Changes in MPS muscle stiffness are affected by many factors and several studies have shown that long-term neck leaning is an important factor in the development of MPS [Citation1,Citation14,Citation26,Citation27]. In this study, the SWVmean of trapezius MPS was found to be significantly positively correlated with neck-leaning time, suggesting that increased trapezius stiffness is associated with long-term neck-leaning, overuse of neck muscles, and muscle strain, in study participants. The results of this study suggest that MTrPs in the skeletal muscles of patients with MPS may be related to increased stiffness caused by chronic improper posture. In addition, long-term use of mobile phones and computers in the forward head posture may simultaneously affect the bilateral trapezius muscles. Although patients with unilateral trapezius MPS show symptoms on only one side, the contralateral asymptomatic trapezius muscles also show changes in stiffness, such as increased muscle stiffness. Therefore, when assessing skeletal muscle stiffness in patients with MPS, attention should be paid to changes in muscle stiffness on the non-affected side as well as on the affected side.
Conclusion
In patients with trapezius MPS, the muscle stiffnesses in the affected and non-affected sides of the trapezius muscle were significantly higher than that of normal trapezius muscles, and the extent of the increase was positively correlated with the time of cervical forward leaning. This suggested that increased skeletal muscle stiffness in trapezius MPS was associated with long-term neck leaning, neck muscle overuse, and damage due to muscle fatigue.
Limitations
This study had a few limitations. First, only the stiffness of the trapezius muscle, the most vulnerable skeletal muscle in patients with MPS, was analyzed; the characteristics of other skeletal muscles involved in MPS pathology require further investigation. Second, this study only analyzed the correlation between neck leaning time and SWVmean and did not consider other relevant factors such as the occupation of the participants, the time and intensity of daily physical exercise, and the time and frequency of staying up late. Third, electromyography (EMG) was not conducted in this study. Assessing EMG activity during the SWE measurements would strengthen our findings [Citation30,Citation31]. Furthermore, the number of cases in this study was relatively small; therefore, further research is needed in future studies to obtain more definite conclusions.
Ethical approval
This study was approved by the Ethical Review Committee of the Third Hospital of Shanxi Medical University (Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, and Tongji Shanxi Hospital, China), and was performed in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from all participants of this study.
Author contributions
CJ Hao and QB Zhang participated in the conception and design of the experiments; CJ Hao, WL Xiao performed most of the experiments; XM Tan analyzed and interpreted the data; CJ Hao drafted the paper and critically revised it for intellectual content. All authors read and approved the final manuscript. And that all authors agree to be accountable for all aspects of the work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data used and analysed in the study are available by contacting the corresponding authors upon reasonable request.
Additional information
Funding
References
- Simons DG, Travel JG, Simons LS. Myofascial pain and dysfunction: the trigger point manual. Vol. 1. Baltimore (MD): Williams & Wilkins/Wolters Kluwer Health Inc; 1999.
- Kumbhare D, Shaw S, Grosman-Rimon L, et al. Quantitative ultrasound assessment of myofascial pain syndrome affecting the trapezius: a reliability study. J Ultrasound Med. 2017;36(12):1–9. doi:10.1002/jum.14308.
- Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724. doi:10.1016/j.jpain.2012.03.009.
- Skootsky SA, Jaeger B, Oye RK. Prevalence of myofascial pain in general internal medicine practice. West J Med. 1989;251:157–160.
- Money S. Pathophysiology of trigger points in myofascial pain syndrome. J Pain Palliat Care Pharmacother. 2017;31(2):158–159. doi:10.1080/15360288.2017.1298688.
- Hagberg H, Kvarnstrom S. Muscular endurance and electromyographic fatigue in myofascial shoulder pain. Arch Phys Med Rehabil. 1984;65:522–525.
- Akagi R, Kusama S. Comparison between neck and shoulder stiffness determined by shear wave ultrasound elastography and a muscle hardness meter.ltrasound. Ultrasound Med Biol. 2015;41(8):2266–2271. doi:10.1016/j.ultrasmedbio.2015.04.001.
- Mannion AF, Dolan P. Relationship between myoelectric and mechanical manifestations of fatigue in the quadriceps femoris muscle group. Eur J Appl Physiol Occup Physiol. 1996;74(5):411–419. doi:10.1007/BF02337721.
- Ishikawa H, Muraki T, Morise S, et al. Changes in stiffness of the dorsal scapular muscles before and after computer work: a comparison between individuals with and without neck and shoulder complaints. Eur J Appl Physiol. 2017;117(1):179–187 doi:10.1007/s00421-016-3510-z.
- Taş S, Korkusuz F, Erden Z. Neck muscle stiffness in participants with and without chronic neck pain: a Shear-Wave elastography study. J Manipulative Physiol Ther. 2018;41(7):580–588. doi:10.1016/j.jmpt.2018.01.007.
- Săftoiu A, Gilja OH, Sidhu PS, et al. The EFSUMB guidelines and recommendations for the clinical practice of elastography in Non-Hepatic applications: update 2018. Ultraschall Med. 2019;40(4):425–453. doi:10.1055/a-0838-9937.
- Cosgrove D, Piscaglia F, Bamber J, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography part 2: clinical applications. Ultraschall Med. 2013;34(3):238–253. doi:10.1055/s-0033-1335375.
- Adigozali H, Shadmehr A, Ebrahimi E, , et al. Reliability of upper trapezius morphology, its mechanical properties and blood flow in female patients with myofascial pain syndrome using ultrasonography. J Bodyw Mov Ther. 2017;21(1):35–40. doi:10.1016/j.jbmt.2016.04.010.
- Ballyns JJ, Turo D, Otto P, et al. Office-based elastographic technique for quantifying mechanical properties of skeletal muscle. J Ultrasound Med. 2012;31(8):1209–1219. doi:10.7863/jum.2012.31.8.1209.
- Sikdar S, Ortiz R, Gebreab T, et al. A new application of ultrasound imaging to characterize tissue properties and blood flow in myofascial pain syndromes. IEEE. 2010. p. 1380–1383.
- Taljanovic MS, Gimber LH, Becker GW, et al. Shear-Wave elastography: basic physics and musculoskeletal applications. Radiographics. 2017;37(3):855–870. doi:10.1148/rg.2017160116.
- Brandenburg JE, Eby SF, Song P, et al. Quantifying passive muscle stiffness in children with and without cerebral palsy using ultrasound shear wave elastography. Dev Med Child Neurol. 2016;58(12):1288–1294. doi:10.1111/dmcn.13179.
- Dubois G, Kheireddine W, Vergari C, et al. Reliable protocol for shear wave elastography of lower limb muscles at rest and during passive stretching. Ultrasound Med Biol. 2015;41(9):2284–2291. doi:10.1016/j.ultrasmedbio.2015.04.020.
- Du LJ, He W, Cheng LG, et al. Ultrasound shear wave elastography in assessment of muscle stiffness in patients with parkinson's disease: a primary observation. Clin Imaging. 2016;40(6):1075–1080. doi:10.1016/j.clinimag.2016.05.008.
- Chen XM, Cui LG, He P, et al. Shear wave elastographic characterization of normal and torn achilles tendons: a pilot study. J Ultrasound Med. 2013;32(3):449–455. doi:10.7863/jum.2013.32.3.449.
- Gerwin RD. Diagnosis of myofascial pain syndrome. Phys Med Rehabil Clin N Am. 2014;25(2):341–355. doi:10.1016/j.pmr.2014.01.011.
- Asteria C, Giovanardi A, Pizzocaro A, et al. US-elastography in the differential diagnosis of benign and malignant thyroid nodules. Thyroid. 2008;18(5):523–531. doi:10.1089/thy.2007.0323.
- Schaefer FK, Heer I, Schaefer PJ, et al. Breast ultrasound elastography–results of 193 breast lesions in a prospective study with histopathologic correlation. Eur J Radiol. 2011;77(3):450–456. doi:10.1016/j.ejrad.2009.08.026. Epub 2009 Sep 20.
- Barr RG, Wilson SR, Rubens D, et al. Update to the society of radiologists in ultrasound liver elastography consensus statement. Radiology. 2020;296(2):263–274. doi:10.1148/radiol.2020192437.
- Brandenburg JE, Eby SF, Song PF, et al. Feasibility and reliability of quantifying passive muscle stiffness in young children by using shear wave ultrasound elastography. J Ultrasound Med. 2015;34(4):663–670. doi:10.7863/ultra.34.4.663.
- Yoshitake Y, Takai Y, Kanehisa H, et al. Muscle shear modulus measured with ultrasound shear-wave elastograghy across a wide range of contraction intensity. Muscle Nerve. 2014;50(1):103–113. doi:10.1002/mus.24104.
- Aubry S, Nueffer J-P, Michel F, et al. Viscoelasticity in achilles tendonopathy:quantitative assessment by using real-time shear-wave elastography. Radiology. 2015;274(3):821–829. doi:10.1148/radiol.14140434.
- Chen Q, Wang H-J, Gay RE, et al. Quantification of myofascial taut bands. Arch Phys Med Rehabil. 2016;97(1):67–73. doi:10.1016/j.apmr.2015.09.019.
- Valera-Calero JA, Sánchez-Jorge S, Buffet-García J, et al. Is Shear-Wave elastography a clinical severity indicator of myofascial pain syndrome? An observational study. J Clin Med. 2021;10(13):2895. doi:10.3390/jcm10132895.
- Westgaard RH, Vasseljen O, Holte KA. Trapezius muscle activity as a risk indicator for shoulder and neck pain in female service workers with low biomechanical exposure. Ergonomics. 2001;44(3):339–353. doi:10.1080/00140130119649.
- Østensvik T, Veiersted KB, Nilsen P. Association between numbers of long periods with sustained low-level trapezius muscle activity and neck pain. Ergonomics. 2009;52(12):1556–1567. doi:10.1080/00140130903199889.