Abstract
Purpose
To evaluate the retinal and choroidal microvasculature after one or two horizontal rectus muscle surgeries in strabismus patients using swept-source optical coherence tomography angiography (SS-OCTA).
Methods
30 eyes of 26 patients who underwent horizontal rectus muscle surgery were included in this study. Group A, A’ and Group B , B’ respectively consisted preoperative and postoperative measurements of patients who underwent one or two horizontal rectus muscle surgeries. We analyzed the vessel density (VD) of the superficial vascular complex (SVC), the deep vascular complex (DVC), the choriocapillary layer (CC), choroidal vascular index (CVI), choroidal thickness (T-Ch) and retinal nerve fiber layer thickness (T-RNFL) preoperatively, and one week postoperatively.
Results
Only in the nasal sector of the perifoveal zone, the VD in SVC demonstrated a significant increase in Group A’ (p = 0.027). There was a statistically significant difference in the VD changes of SVC between Group A and Group B (p = 0.043). The VD in DVC did not change significantly in the whole macular compared with the preoperative. Moreover, in both Group A’ and Group B’, the VD in CC showed a reduction in a single sector of the parafoveal area (p < 0.05). Group A’ have increased CVI in the nasal sector of the perifoveal region (p = 0.008). In addition, the T-Ch increase in the perifoveal region was more significant in Group B’ than in Group A’ (p < 0.05). Group A’ showed statistically significant decreases in T-RNFL in the foveal and parafoveal regions (p < 0.05).
Conclusion
This study revealed that the increase in choroidal thickness was more significant after two rectus muscle surgery. In addition, there were microvascular changes in sectional macular regions after strabismus surgery. OCTA is an excellent way to study the impact of strabismus surgery on the macular structure and blood flow.
Key Messages
We used SS-OCTA, which provided more objective and accurate measurements, to assess macular vessel density and thickness of retinal and choroid after one or two horizontal rectus muscle surgeries.
Introduction
The anterior ciliary artery (ACA) originates from the ophthalmic artery (OA) and crosses the sclera into the eye accompanying four rectus muscles. Typically, there is only one ACA on the lateral rectus muscle (LR) while there are two ACAs on the other three rectus muscles [Citation1,Citation2]. The ACAs provide 70–80% of the blood supply to the anterior segment of the eye [Citation3,Citation4]. Strabismus surgery on the rectus muscles may transect the ACAs and result in altered hemodynamics in the anterior segment. Anterior segment ischemia (ASI) is a serious complication of strabismus surgery [Citation5]. The risk of ASI is increased when strabismus surgery is performed on two or more muscles [Citation6,Citation7]. The retinal arteries, the posterior ciliary arteries, and the ACAs all originate from the OA [Citation8]. The transection of the ACAs in strabismus surgeries results in altered hemodynamics of the OA and then affects the blood flow of retinal arteries and posterior ciliary artery, which supply the retina and choroid. All rectus muscles carry ACAs, so the number of operated muscles may influence the postoperative hemodynamics of the retinal and choroid in varying degrees.
Previously, the changes in ocular hemodynamics after strabismus surgery have been evaluated by colour Doppler ultrasonography (CDI) [Citation1–3,Citation9,Citation10], fluorescein angiography [Citation11] and indocyanine green angiography [Citation6,Citation12], fundus photography [Citation4]. However, there are conflicting results on whether ocular hemodynamics changes after strabismus surgery on one or two horizontal rectus muscles. In addition, some OCT studies have also analyzed the structural changes of the macula and the choroid after strabismus surgery, but no consistent conclusions have been obtained [Citation13–19]. Therefore, it is of significance to explore the postoperative changes in microvasculature and thickness of the retina and choroid in strabismus patients.
Swept-source optical coherence tomography angiography (SS-OCTA) is a noninvasive method of imaging the retina and optic disc with faster scan speeds, denser scan patterns, and larger scan widths [Citation20]. It allows visualization of the posterior pole microvasculature without dye injection and allows assessment of vessel density (VD) in specific retina and choroid layers [Citation21]. Only a few recent OCTA studies have evaluated microvascular changes in the retinal capillaries plexus and choroidal capillaries plexus after strabismus surgery, which have provided diverse results depending on the different times of follow-up [Citation22–25]. Besides, they have not investigated whether there is a difference in the retinal and choroid changes after one or two horizontal rectus muscle surgeries [Citation22–25]. The aim of this study was to use SS-OCTA to assess macular vessel density and thickness of retinal and choroid 1 week after one or two horizontal rectus muscle surgeries in strabismus patients, which provided more objective and accurate measurements.
Subjects and methods
The study was approved by the Ethics Committee of Renmin Hospital of Wuhan University (WDRY2020-K234) and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects for this study.
Subjects
Patients who underwent horizontal rectus muscle surgery in the Eye Center of Renmin Hospital of Wuhan University from May 2021 to April 2022 were included in this study. Exclusion criteria were as follows: (1) age < 18 or > 30; (2) the best corrected visual acuity < 1.0 or axial length > 26.5 mm; (3) history of strabismus surgery or intraocular surgery within the past 6 months; (4) history of glaucoma, intraocular inflammation, intraocular media opacifications, and retinal diseases; (5) history of neurodegenerative diseases; (6) patients who were unable to cooperate at OCTA imaging and those whose images had significant artifacts or poor image quality.
Patients were divided into two groups based on the number of muscles operated. Group A comprised preoperative data from 16 eyes of 12 patients, each of whom underwent one horizontal rectus muscle recession (the medial rectus or the lateral rectus). Group B comprised preoperative data from 14 eyes of 14 patients who underwent two horizontal rectus muscle surgeries, including recession of the medial rectus (MR), recession of the LR, resection of the MR and resection of the LR. Group A’ and B’ respectively comprised postoperative data from patients who underwent one and two horizontal rectus muscle surgeries.
After obtaining a comprehensive medical history, all patients underwent a comprehensive ophthalmologic examination preoperatively and one week postoperatively, including assessment of visual acuity, detailed slit-lamp anterior segment examination, fundoscopy, intraocular pressure measurement, eye movement examination, degree of deviation (alternating coverage tests using prisms at near (33 cm) and distant (6 m)), and OCTA assessment.
OCTA
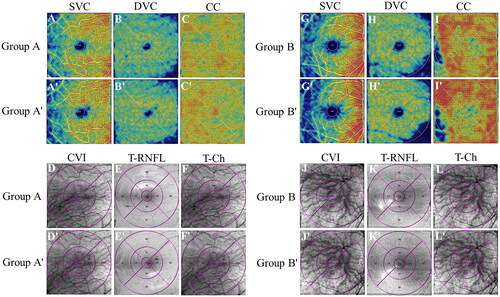
OCTA data were acquired using a commercial SS-OCTA instrument (VG100, SVision Imaging, Ltd., Luoyang, China). A 6 × 6mm2 scanning pattern centered on the fovea was used to assess the macular microvasculature. The retinal vasculature was evaluated in three horizontal segmentations: the superficial vascular complex (SVC), the deep vascular complex (DVC), and the choriocapillary layer (CC). The SVC was defined as the layer starting from 5 μm above the inner limiting membrane to the junction of the inner plexiform and inner nuclear layers (IPL/INL). The DVC extended from the junction of IPL/INL to 25 μm below the outer plexiform layer. The CC consisted of the capillaries in the layer from 10 μm above the Bruch’s membrane to 25 μm below it. The VD of SVC, DVC and CC, choroidal vascular index (CVI, the ratio of the luminal area to total choroidal area), choroidal thickness (T-Ch) and retinal nerve fiber layer thickness (T-RNFL) were automatically measured using the built-in software ().
Figure 1. Representative OCTA macular images of different groups. Measurements of a 11-year-old female who underwent one horizontal rectus muscle surgery are shown in the left column (A-F and A’-F’) and measurements of a 17-year-old female who underwent two horizontal rectus muscle surgery are shown in the right column (G-L and G’-L’). all measurements are automatically calculated in the superior, temporal, inferior, and nasal sectors of the parafoveal and perifoveal area. SVC, superficial vascular complex; DVC, deep vascular complex; CC, choriocapillary layer; CVI, choroidal vascular index; T-Ch, choroidal thickness; T-RNFL, retinal nerve fiber layer thickness.
The Early Treatment Diabetic Retinopathy Study (ETDRS) macular subfields consist of foveal area (1.0 mm diameter circle), parafoveal area (1.0 mm inner diameter, 3.0 mm outer diameter ring), and perifoveal area (3.0 mm inner diameter, 6.0 mm outer diameter ring). The parafoveal area and perifoveal area were divided into superior, temporal, inferior, and nasal sectors.
Data analysis
The SPSS version 23.0 was used for statistical analysis. The Shapiro-Wilk test was used to determine the distribution and normality of the data. Paired sample t test or paired Wilcoxon signed rank test was performed to compare differences between preoperative and postoperative 1 week. Independent sample t test or Mann-Whitney U test was used for comparison between Group A and Group B. p < 0.05 was considered to be statistically significant. All data were expressed as mean and standard deviation (SD).
Results
A total of 30 eyes of 26 strabismus patients (16 women, 62%) undergoing horizontal rectus muscle surgery were included, with a mean patient age of 18.00 ± 10.96 years in Group A and 25.57 ± 9.33 years in Group B. The average deviation in Group A was 29.00 ± 8.95PD at near and 21.41 ± 5.45PD at distant while the average deviation in Group B was 59.71 ± 15.31PD at near and 51.36 ± 10.59PD at distant. There was a significant difference in the average deviation between the two groups (p < 0.05). The modalities of the strabismus surgery included recession and resection of the extraocular muscles. No intraoperative or postoperative complications were observed.
Measurement of capillary vessel density
Only in the nasal sector of the perifoveal zone, the VD in SVC demonstrated a significant increase in Group A’ compared with Group A (p = 0.027; ). The VD in SVC did not change significantly in Group B’ (p > 0.05; ). One week after surgery, there was a statistically significant difference in the VD changes of SVC between Group A’ and Group B’ (p = 0.043; ). Moreover, comparisons between Group A and A’, Group B and B’ revealed that the VD in DVC did not change significantly in the whole macular (p > 0.05). In addition, in Group A’ and Group B’, the VD in CC all showed a reduction in a single sector of the parafoveal area (p = 0.045, p = 0.025). In addition, Group A’ showed increased CVI in the nasal sector of the perifoveal region after surgery (p = 0.008).
Figure 2. Changes in macular vessel densities, retinal nerve fiber layer and choroidal thickness preoperatively and postoperatively in eyes undergoing one horizontal rectus surgery. VD, vessel density; SVC, superficial vascular complex; DVC, deep vascular complex; CC, choriocapillary layer; CVI, choroidal vascular index; T-Ch, choroidal thickness; T-RNFL, retinal nerve fiber layer thickness; S, superior; T, temporal; I, inferior; N, nasal.
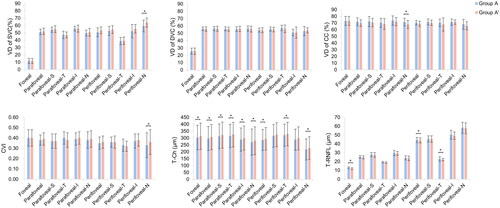
Table 1. Comparision of retinal and choroidal blood flow changes between patients under one or two horizontal rectus muscle surgeries.
Retinal nerve fiber layer and choroidal thickness measurements
The T-Ch in the foveal, parafoveal and perifoveal areas of the operated eyes were significantly increased in both Group A’ and Group B’ (p < 0.05; ) (except for the superior and inferior sectors of the perifoveal area in Group A’). Moreover, the T-Ch increase in the perifoveal region was more significant in Group B’ than in Group A’ (p < 0.05; ). Eyes in Group A’ showed statistically significant decreases in T-RNFL in the foveal and parafoveal regions (p < 0.05). The temporal T-RNFL in the parafoveal and perifoveal regions decreased in Group B’ (p = 0.026, p = 0.023).
Figure 3. Changes in macular vessel densities, retinal nerve fiber layer and choroidal thickness preoperatively and postoperatively in eyes undergoing two horizontal rectus surgery. VD, vessel density; SVC, superficial vascular complex; DVC, deep vascular complex; CC, choriocapillary layer; CVI, choroidal vascular index; T-Ch, choroidal thickness; T-RNFL, retinal nerve fiber layer thickness; S, superior; T, temporal; I, inferior; N, nasal.
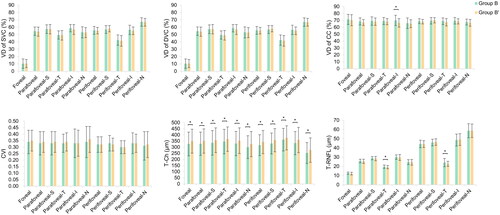
Table 2. Comparision of choroidal and retinal nerve fiber layer thickness changes between patients under one or two horizontal rectus muscle surgeries.
Discussion
Our study showed some peripheral microvascular changes in the retina and choroid after strabismus surgery, but the central macular area was unaffected. For thickness, the choroidal thickness increased significantly and the RNFL thickness decreased after surgery. In addition, by comparing OCTA measurements of patients undergoing one or two horizontal rectus muscle surgeries, we found that the increase in choroidal thickness was more significant after two rectus muscles surgery.
In our study, we observed an increase in SVC and CVI in the nasal sector of the perifoveal region 1 week after surgery, which may result from an inflammatory response induced by surgery or a compensatory mechanism to prevent hypoperfusion after injury to the ACAs [Citation22–25]. Earlier color Doppler ultrasound studies have shown an increase in the retrobulbar blood flow velocity 1 day after single or double rectus muscle surgeries, and the increase was thought to be the expected outcome in an inflammatory state [Citation2,Citation9]. However, it may signal a reduction in inflammation that all velocities and measurements had returned to baseline by postoperative day 7 [Citation2,Citation9]. Recently, OCTA studies were performed to measure hemodynamic changes in the retina and choroid, one of which revealed a transient increase in deep capillary plexus(DCP) and CC 1 day after strabismus surgery, with no significant change in superficial capillary plexus(SCP) [Citation24]. Our results showed significant differences in just some subregions, which may be because the inflammation has gradually reduced at postoperatively one week or the compensatory capacity is so strong that the vascular perfusion of the retina and choroid have not been affected widely. In addition, the retinal and choroidal blood flow in some peripheral regions changed after strabismus surgery while the foveal blood flow remained the same as before surgery in our study, which may be due to the stronger compensatory capacity of the foveal region. Moreover, Vagge et al. [Citation24] reported no alteration in VD of the retina 1 month after strabismus surgery by fornix approach while Inal et al. [Citation23] claimed that there was still a significant increase in VD measurements in both SCP and DCP 3 months after surgery by limbal conjunctival incision. We speculated that the duration of the hemodynamic disturbances varied because of different surgical methods. Furthermore, there was no significant difference in VD changes between Group A’ and Group B’ except the VD of SVC in the perifoveal nasal sector, indicating that one or two muscle procedures did not influence the extent to which blood flow was altered. OCTA is an excellent way to detect changes of microvessel in the retina and choroid for early discovery of ischemia or inflammation.
Consistent with the results of Mintz et al. Atalay et al. and Alis et al. [Citation15,Citation17,Citation19], we found that rectus muscle surgery resulted in increased choroidal thickness, which may be due to mechanical traction of choroidal microcirculation during the operation and postoperative inflammation. On the one hand, the disruption of ACAs and obstruction of venous drainage caused by recession or resection of the rectus muscle may lead to choroidal circulation disturbance, resulting in the thickening of the choroid [Citation17]. Another possible explanation is that the temporary increase of T-Ch is related to inflammation. Surgical trauma can lead to the release of proinflammatory cytokines and prostaglandins in the aqueous humor, and then they reach the retina through the vitreous body and damage the internal and external blood-retinal barrier [Citation17]. The increased vascular permeability can cause a large amount of fluid to leak into the retina, leading to choroidal thickening. Regardless of the number of muscles that intervened, inflammation after strabismus surgery may cause an inflammatory cascade in the posterior segment [Citation19]. In contrast to Alis et al.’s result that there was no difference between one and two horizontal rectus muscle surgeries, we found a more significant increase in choroidal thickness in Group B’, which may result from the greater intraoperative strain and postoperative inflammatory response in two rectus muscles surgery. Therefore, strabismus patients’ fundus blood flow is suggested to be a consideration in surgical choice. In addition, we observed a decrease of T-RNFL in some regions after surgery compared with preoperative, which was more significant in patients who underwent one rectus surgery. Though Alis et al. [Citation19] did not find any significant changes in RNFL thickness 1 week after surgery, there was a decreasing trend in patients undergoing one horizontal rectus surgery, which may be the result of blood flow changes postoperatively. However, more researches are needed to confirm our above inference.
This study has the following limitations: First, the sample size is small. Further studies with a large sample size will help us to clarify the impact of strabismus surgery on ocular microvasculature and thickness changes. Second, the changes of the retinal and choroidal blood flow were mainly focused in the early postoperative period, while alteration of them in long-term follow-up was lacking. Third, comparison between the recession and resection should be undertaken to explore impact of surgical methods more convincingly. Finally, the effect of local anesthesia on ocular blood vessels was not considered.
In conclusion, this study revealed that the increase in choroidal thickness was more significant after two rectus muscle surgery compared to one rectus muscle surgery, which may be the result of the greater intraoperative strain and postoperative inflammatory response. In addition, there were microvascular changes in sectional macular regions after one or two horizontal rectus muscle surgery. OCTA is a very effective tool for monitoring impact of strabismus surgery or extraocular surgery on the structure and blood flow of the retina and choroid, with which the clinician can detect changes of microvessel in the retina and choroid earlier and give the patient appropriate intervention early on.
Author contributions
DH, YX, CC, HZ, YX and ZC were involved in the conception and design. DX, TC, and YM collected the data. DX, TC, DH, HZ and YX were involved in the analysis and interpretation of the data. DX drafted the manuscript. DH, HZ and YX contributed to the critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. All authors have read and agreed to be accountable for all aspects of the work.
Acknowledgment
The authors thank all of the patients who participated in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, DH and HZ, upon reasonable request.
Additional information
Funding
References
- Bayramlar H, Totan Y, Cekic O, et al. Evaluation of hemodynamic changes in the ophthalmic artery with color doppler ultrasonography after strabismus surgery. J Pediatr Ophthalmol Strabismus. 2000;37(2):1–7. doi:10.3928/0191-3913-20000301-08.
- Pelit A, Barutcu O, Oto S, et al. Investigation of hemodynamic changes after strabismus surgery using color doppler imaging. J Aapos. 2002;6(4):224–227. doi:10.1067/mpa.2002.124901.
- Güven D, Ziraman I, Tomaç S, et al. Hemodynamic changes after strabismus surgery. Strabismus. 2000;8(1):21–27. doi:10.1076/0927-3972(200003)811-6ft021.
- Zhou J, Fu J, Li J, et al. Quantitative measurement of retinal vascular diameter changes in the early postoperative period after strabismus surgery. J Aapos. 2017;21(4):274–277. doi:10.1016/j.jaapos.2017.04.004.
- Velez FG, Davila JP, Diaz A, et al. Association of change in iris vessel density in optical coherence tomography angiography with anterior segment ischemia after strabismus surgery. JAMA Ophthalmol. 2018;136(9):1041–1045. doi:10.1001/jamaophthalmol.2018.2766.
- Oltra EZ, Pineles SL, Demer JL, et al. The effect of rectus muscle recession, resection and plication on anterior segment circulation in humans. Br J Ophthalmol. 2015;99(4):556–560. doi:10.1136/bjophthalmol-2014-305712.
- Pineles SL, Chang MY, Oltra EL, et al. Anterior segment ischemia: etiology, assessment, and management. Eye (Lond). 2018;32(2):173–178. doi:10.1038/eye.2017.248.
- Reiner A, Fitzgerald MEC, Del Mar N, et al. Neural control of choroidal blood flow. Prog Retin Eye Res. 2018;64:96–130. doi:10.1016/j.preteyeres.2017.12.001.
- Lee NH, Lee SN. Investigation of hemodynamic changes in the ophthalmic artery using color doppler imaging after strabismus surgery. Korean J Ophthalmol. 2005;19(3):208–212. doi:10.3341/kjo.2005.19.3.208.
- Akyüz Unsal AI, Unsal A, Ozkan SB, et al. The effect of strabismus surgery on retrobulbar hemodynamics. J Aapos. 2007;11(3):277–281. doi:10.1016/j.jaapos.2006.12.059.
- Kaeser PF, Klainguti G. Anterior segment angiography in strabismus surgery. Klin Monbl Augenheilkd. 2012;229(4):362–364. doi:10.1055/s-0031-1299283.
- Chan TK, Rosenbaum AL, Rao R, et al. Indocyanine green angiography of the anterior segment in patients undergoing strabismus surgery. Br J Ophthalmol. 2001;85(2):214–218. doi:10.1136/bjo.85.2.214.
- Kasem MA, Sabry D. Detection of macular changes by optical coherence tomography after inferior oblique muscle surgery. J Aapos. 2011;15(4):334–337. doi:10.1016/j.jaapos.2011.07.003.
- Turan-Vural E, Unlu C, Erdogan G, et al. Evaluation of macular thickness change after inferior oblique muscle recession surgery. Indian J Ophthalmol. 2014;62(6):715–718. doi:10.4103/0301-4738.136230.
- Mintz HR, Waisbourd M, Kessner R, et al. Macular thickness following strabismus surgery as determined by optical coherence tomography. J Pediatr Ophthalmol Strabismus. 2016;53(1):11–15. doi:10.3928/01913913-20160113-07.
- Inan K, Niyaz L. The effect of strabismus surgery on choroidal thickness. Eur J Ophthalmol. 2018;28(3):268–271. doi:10.5301/ejo.5001025.
- Atalay HT, Arıbaş YK, Üçgül AY, et al. Subfoveal choroidal thickness change following strabismus surgery. Kocatepe Tıp Dergisi. 2019;20(1):183–187. doi:10.18229/kocatepetip.575058.
- Yetkin AA, Simsek A. Evaluation of choroidal thickness before and after strabismus surgery in paediatric patients by spectral-domain optical coherence tomography. Niger J Clin Pract. 2020;23(9):1243–1247. doi:10.4103/njcp.njcp_500_19.
- Guler Alis M, Alis A. Influence of one or two horizontal muscle surgeries on OCT findings. Strabismus. 2021;29(3):182–188. doi:10.1080/09273972.2021.1948075.
- Lains I, Wang JC, Cui Y, et al. Retinal applications of swept source optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA). Prog Retin Eye Res. 2021;84:100951. doi:10.1016/j.preteyeres.2021.100951.
- Spaide RF, Fujimoto JG, Waheed NK, et al. Optical coherence tomography angiography. Prog Retin Eye Res. 2018;64:1–55. doi:10.1016/j.preteyeres.2017.11.003.
- Huseyinhan Z, Ozcaliskan S, Gurez C, et al. Retinal and choroidal microvasculature is altered after strabismus surgery. Eur J Ophthalmol. 2022;33(2):774–778. doi:10.1177/11206721221137156.
- Inal A, Yilmaz I, Ocak OB, et al. Optical coherence tomography angiography: are there any changes in measurements after strabismus surgery? J Pediatr Ophthalmol Strabismus. 2019;56(2):95–100. doi:10.3928/01913913-20190128-01.
- Vagge A, Nucci P, Ferro Desideri L, et al. Evaluation of macular vessel density changes after strabismus surgery using optical coherence tomography angiography. J Aapos. 2022;26(2):71.e71–71.e74. doi:10.1016/j.jaapos.2021.11.011.
- Çelik S, Dıraçoğlu A, İnal A, et al. Comparison of quantitative measurement of macular vessel density before and after inferior oblique muscle-weakening surgery: an optical coherence tomography angiography study. J Aapos. 2021;25(5):282.e281–282.e285. doi:10.1016/j.jaapos.2021.04.007.
