Abstract
Objective
This study aimed to compare the repeatability and diagnostic efficiency of shear wave elastography (SWE) while using coupling gel and gel pads in the diagnosis of superficial breast lesions.
Methods
Two experienced sonographers, trained in SWE, used different methods to perform the maximum Young’s modulus (Emax) measurement of the lesion while using coupling gel SWE and gel pad SWE at different time points. All 80 lesions were in the superficial layer of the breast. The interclass correlation coefficient (ICC) was calculated to evaluate the intraobserver and interobserver repeatability. Meanwhile, the receiver operating characteristic curve (ROC curve) was used to calculate the sensitivity, specificity and area under the curve of the two methods.
Results
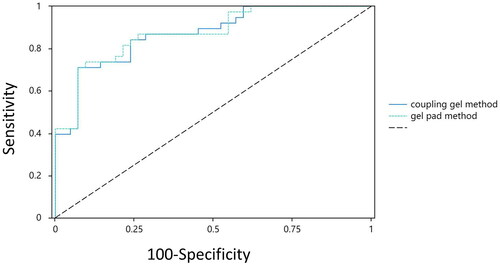
In the 80 breast lesions, the intraobserver and interobserver reproducibility of SWE measurements using coupling gel were considered good, and the ICCs were 0.728 (95% CI: 0.509–0.813) and 0.702 (95% CI: 0.492–0.795), respectively. The intraobserver and interobserver reproducibility of the SWE measured by the gel pad were also considered good, and the ICCs were 0.745 (95% CI: 0.501–0.801) and 0.713 (95% CI: 0.498–0.802), respectively. The sensitivity, specificity and area under the curve were 0.711 and 0.737, 0.929 and 0.905, and 0.873 and 0.878, respectively.
Conclusions
In the SWE measurement of superficial breast lesions, the use of a gel pad does not affect the repeatability and diagnostic efficiency of the measurement.
KEY MESSAGES
The use of gel pads does not affect repeatability and diagnostic efficiency but also improves the near-field resolution of images.
The gel pad has certain advantages in the observation of superficial lesions.
Breast diseases are more prevalent in women. Conventional ultrasonic diagnosis of breast diseases relies mainly on two-dimensional and colour Doppler ultrasound, which have certain limitations in distinguishing the nature of lesions [Citation1]. In terms of colour Doppler studies, some new techniques have been developed. Superb microvascular imaging technology can improve the ultrasound visualization of dermal blood vessels, which cannot be achieved with conventional power Doppler. This is very valuable for the study of dermal abnormalities [Citation2]. A new inspection method, shear wave elastography (SWE), objectively evaluates tissue hardness, which is an inaccessible parameter for traditional methods [Citation3]. At present, SWE has been proven to be effective and reproducible in the diagnosis of benign and malignant breast diseases [Citation4,Citation5]. In clinical ultrasound, gel pads are often used for SWE imaging and the measurement of superficial tissues or lesions [Citation6,Citation7]. However, there are some controversies about whether the use of gel pads will further increase the hardness of the measured target and affect the accuracy of SWE measurement. There are few relevant studies to assess this possibility, especially for superficial tissues or lesions. Therefore, in this study, superficial lesions located within 0–1 cm of the breast were evaluated, and by considering aspects of measurement repeatability and diagnostic efficiency, we determined whether the use of gel pads would affect the SWE measurement of superficial lesions.
Materials and methods
Statement of ethics
This study was approved by the Ethics Committee of the University-Town Hospital of Chongqing Medical University (LL-202326), and the subjects’ written informed consent was obtained. All methods were performed in accordance with the Declaration of Helsinki.
Research objects
From February 2022 to February 2023, 80 patients who were prequalified for breast nodule resection were enrolled in this study, and a total of 80 lesions were examined. All 80 breast nodules were biopsied or surgically removed and pathologically diagnosed. The gold standard is the pathological diagnosis. The included participants had previous ultrasound examinations that revealed breast lesions located 0–1 cm away from the body surface (the posterior edge of the lesion was less than 1 cm away from the body surface). Previous history of breast surgery, trauma, skin scarring, skin oedema and other factors affecting measurement were excluded.
Instruments and measurement methods
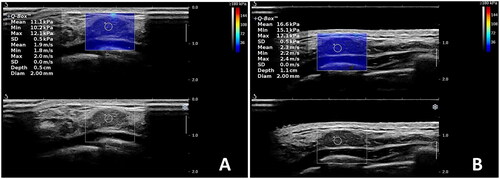
The ultrasonic equipment used was a SuperSonic Imagine AixPlorer, which is a French shear wave elastic imaging ultrasonic diagnostic instrument with a linear array probe of 4–15 MHz. The coupling gel selected for this study was medical-grade ultrasonic coupling gel, in which the main component was liquid gel. The gel pad was solid gelatin, round and approximately 7 mm thick. The subjects were in a supine position with their hands abducted and their breasts fully exposed. The operators were two sonographers with 10 years of experience in ultrasound diagnosis. Two operators performed SWE measurements on 80 lesions at different time points using different methods. Specific methods: Adjust the two-position image quality, enable SWE, select the appropriate area of interest according to the size of the lesion, cover the lesion as much as possible, and freeze the image when the colour filling is stable, as shown in . The Q-Box with a default diameter of 2 mm was activated and placed on the hardest part of the lesion displayed by SWE, and the Emax value was measured. Specific detection steps: examiner 1, according to the above principles, first measured each lesion 3 consecutive times with the coupling gel and calculated the average value to obtain the first measurement results of examiner 1 with the coupling gel. Then, examiner 1 measured each lesion 3 consecutive times with the gel pad and calculated the average value to obtain the first measurement results of examiner 1 with the gel pad. After 10 min, examiner 1 followed the same procedure to obtain the results of examiner 1’s second measurement with coupling gel and examiner 1’s second measurement with a gel pad. One hour later, the procedure was repeated by examiner 2 to obtain the relevant measurements. During the measurement process, examiners did not know the measurement results at any stage. A total of eight groups of data were obtained and stored in Excel for analysis.
Statistical methods
SPSS 19.0 software (SPSS Inc., Chicago, IL) was used to analyse the intraobserver and interobserver repeatability of the two examiners using the interclass correlation coefficient (ICC). Intraobserver repeatability is defined as ICC values measured at different time points using the same method for the same examiner. Interobserver repeatability was defined as the ICC values measured by two examiners using the same method. Repeatability score: <0.40 is poor, 0.40–0.75 is good and ≥0.75 is very good. At the same time, receiver operating characteristic curves (ROC curves) were drawn to calculate the sensitivity, specificity and area under the curves of the two methods. p < .05 was considered to indicate a statistically significant difference.
Results
The 80 female participants ranged in age from 20 to 62 years, with a mean of 42.0 ± 11.2 years. All 80 lesions were located 0–1 cm from the body surface (the posterior edge of the lesion was less than 1 cm from the body surface). The left and right diameters were 8–11 mm, with an average of 9.3 ± 1.1 mm; the upper and lower diameters were 6–9 mm, with an average of 7.6 ± 1.1 mm; and the anterior and posterior diameters were 4–8 mm, with an average of 5.9 ± 1.5 mm.
Comparing the mean Emax values of 80 nodules measured by the two ultrasound methods, there was no significant difference (p = .072). The intraobserver and interobserver repeatability of SWE measurements of breast lesions taken with the coupling gel or with the gel pad were each rated as good, as shown in and .
Table 1. Results of intraobserver repeatability analysis of Emax values of breast nodules repeatedly measured by examiner 1 using the same method (n = 80).
Table 2. Results of interobserver repeatability analysis of Emax values of breast nodules repeatedly measured by examiners 1 and 2 using the same method (n = 80).
All 80 lesions were pathologically diagnosed, among which 38 cases were malignant (47.50%) and 42 cases were benign (52.50%). The sensitivity and specificity of coupling gel SWE were 0.711 and 0.929, respectively. The sensitivity and specificity of gel pad SWE were 0.737 and 0.905, respectively. The areas under the ROC curves of the coupling gel and gel pad were 0.873 and 0.878, respectively. The area under the ROC curve of the two measurement methods showed no significant difference (p = .559), as shown in and .
Table 3. Area under the ROC curve and confidence interval of coupling gel and gel pad SWE (n = 80).
Conclusions
The application principle of ultrasonic elastic imaging in medicine is that human tissues will deform after being stressed, and different hardness values will be displayed according to different degrees of tissue deformation. Different hardness values reflect different properties of tissues, thus providing certain diagnostic information for clinical practice [Citation8]. For traditional strain elastography, the operator needs to artificially apply pressure to the tested tissue to obtain the elastic value of the tissue. This method has high requirements for the operator’s techniques and a strong dependence on experience. At the same time, it will produce different measurement results due to the different pressures applied by different operators. These factors make the measurement accuracy and repeatability of the elasticity value low. Because shear wave elastic imaging does not require external force during operation, its measurement repeatability and stability are better than those of traditional elastic imaging [Citation9]. As a result, it is widely used in clinical settings, especially in the evaluation of lesions of the breast, thyroid and musculoskeletal system [Citation10]. Studies have shown that there is a statistically significant difference in the elasticity between benign and malignant breast lesions, suggesting that the measurement of breast elasticity is valuable in the differential diagnosis of benign and malignant breast lesions [Citation5].
Currently, ultrasonic technology and equipment continue to improve with good resolution. Studies have shown that high-frequency probes (>15 MHz) can better reveal the morphology and vascular distribution of breast lesions. Ideally, two frequencies of probes should be used during breast examination: one frequency range between 7.5 and 14 MHz and the other frequency range between 15 and 24 MHz. The former transducer is advantageous for deep tissue and large masses due to its high penetrating power, while the latter transducer is more advantageous for detailed observation of superficial lesions due to its higher resolution [Citation11]. However, based on the ultrasonic imaging principle, the near-field shallow resolution is poor, and ultrasonic artefacts are easily produced. Therefore, in the clinical observation of superficial tissue, gel pads are often used to increase the near-field distance and improve the permeability of media to achieve ultrasonic resolution in superficial tissue. Studies have shown that gel pads are superior to ordinary liquid coupling gels through the transmission of high-frequency sound energy, and with coupling gels, tiny bubbles are contained in liquid couplings, possibly causing ultrasonic artefacts and affecting the visibility of superficial skin structures [Citation12,Citation13]. Furthermore, some masses in superficial tissues are raised to the skin surface, irregularly shaped or located in uneven skin sites, which creates contact difficulty between the ultrasound probe and tissue, limiting the image display range. Clinically, the use of a gel pad can fill the gap between the probe and the examined tissue so that the two are in full contact, increasing the display range and improving the image quality. The role of gel pads has been confirmed, and they are widely used in ultrasound examinations of superficial tissues, especially to provide a wider scanning area and comprehensive visualization of the target area [Citation14,Citation15]. Studies have shown that gel pads can improve blood flow signals in and around the lesion, which is extremely important for evaluating the blood supply of the tumour [Citation16]. Similarly, when performing SWE detection, for shallow tissues, gel pads are also widely used, and it is easy to obtain stable SWE images. However, there is concern that the use of gel pads may affect the repeatability of SWE measurement results and the diagnostic efficiency of lesions. In particular, there is concern that the weight of the gel pad itself could enhance the hardness of the measured tissue. The results of this study show that for superficial breast lesions, the use of gel pads and coupling gels can achieve good repeatability, as there is no significant difference in diagnostic efficacy between the use of gel pads or coupling gels. The possible reasons are as follows: (1) the weight of the gel pad itself may have little influence on the pressure of the tissue, which is not enough to cause deformation of the tissue and will not affect the measurement results. (2) The gel pad has a large contact area with the skin, so the pressure is evenly distributed on the skin, and the actual influence on the strength of the measured nodules may be overestimated. It should be noted that regardless of whether the coupling gel is used or the gel pad is used for SWE detection of superficial tissue, the operator of the probe should try to avoid pressure on the tissue or the gel pad. Studies have shown [Citation17] that the lack of unified quantitative indicators for the pressure of probes used by the same operator or different operators will lead to differences in measurement results.
The gel pad also has good permeability, which improves the image quality and increases the near-field distance of ultrasound so that the near-field image display is clearer. Studies have shown that the gel pad provides high-quality imaging of thyroid nodules and skin tumours at the elbow and fingers [Citation18]. However, high-quality two-dimensional images have advantageous measurement results, which can improve the repeatability and accuracy of the measurement results. Therefore, the gel pad is considered to have certain advantages in the measurement of superficial two-dimensional ultrasound and SWE.
Limitations of this study: The number of lesions included in this study was small, and a larger sample study is needed to confirm the influence of the gel pad on the measured SWE values in the future. Moreover, the breast nodules included in this study were generally small and did not protrude from the skin to form a bulge. This makes the pressure distribution of the gel pad on the skin more uniform, and no independent compression of the nodule occurs. Therefore, whether the gel pad will affect the SWE measurement results of skin-raised nodules should be further studied.
In conclusion, we believe that the use of a gel pad will not affect the repeatability and diagnostic efficiency of SWE measurement in superficial breast lesions and can also increase the two-dimensional image resolution of superficial tissues.
Author contributions
Zhijun Zhang: conception and design, drafting of the paper; Hui Wang and Shu He: conception and design, analysis and interpretation of the data; Zhijun Zhang, Shu He, Yu Zhong, Hairong Zou, Lu Cai and Yan Zhang: analysis and interpretation of the data. All authors agree to be accountable for all aspects of the work.
Ethical approval
This study was approved by the Ethics Committee of the University-Town Hospital of Chongqing Medical University.
Acknowledgements
The authors thank all volunteers who participated in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data may be obtained from the corresponding author upon reasonable request.
Additional information
Funding
References
- Meuwly JY. Ultrasound for breast cancer screening: an effective tool in a personalized screening. Praxis (Bern 1994). 2015;104(25):1–6. doi: 10.1024/1661-8157/a002208.
- Corvino A, Varelli C, Cocco G, et al. Seeing the unseen with superb microvascular imaging: ultrasound depiction of normal dermis vessels. J Clin Ultrasound. 2022;50(1):121–127. doi: 10.1002/jcu.23068.
- Schellhaas B, Strobel D, Wildner D, et al. Two-dimensional shear-wave elastography: a new method comparable to acoustic radiation force impulse imaging? Eur J Gastroenterol Hepatol. 2017;29(6):723–729. doi: 10.1097/MEG.0000000000000846.
- Feldmann A, Langlois C, Dewailly M, et al. Shear wave elastography (SWE): an analysis of breast lesion characterization in 83 breast lesions. Ultrasound Med Biol. 2015;41(10):2594–2604. doi: 10.1016/j.ultrasmedbio.2015.05.019.
- Tian J, Liu Q, Wang X, et al. Application of 3D and 2D quantitative shear wave elastography (SWE) to differentiate between benign and malignant breast masses. Sci Rep. 2017;7:41216.
- Kim YJ, Kim SH, Jeh SK, et al. Gel pad application for automated breast sonography. J Ultrasound Med. 2015;34(4):713–719. doi: 10.7863/ultra.34.4.713.
- Del Signore F, De Dominicis S, Mastromatteo G, et al. Sonoelastography of normal canine common calcaneal tendon: preliminary results. Vet Comp Orthop Traumatol. 2021;34(3):200–205. doi: 10.1055/s-0040-1721660.
- Cui XW, Li KN, Yi AJ, et al. Ultrasound elastography. Endosc Ultrasound. 2022;11(4):252–274. doi: 10.4103/EUS-D-21-00151.
- Celletti I, Fresilli D, De Vito C, et al. TIRADS, SRE and SWE in INDETERMINATE thyroid nodule characterization: which has better diagnostic performance? Radiol Med. 2021;126(9):1189–1200. doi: 10.1007/s11547-021-01349-5.
- Franckenberg S, Gubler C, Frauenfelder T, et al. Radiologie-Update Ultraschall-Elastografie – Quintessenz für die Praxis [Radiology update ultrasound elastography – quintessence for the primary care physician]. Praxis (Bern 1994). 2016;105(3):139–145. doi: 10.1024/1661-8157/a002249.
- Corvino A, Varelli C, Catalano F, et al. Use of high-frequency transducers in breast sonography. J Pers Med. 2022;12(12):1960. doi: 10.3390/jpm12121960.
- Chhay S, Hanazono K, Kitahara J, et al. The effects of gel pad thickness on the evaluation of skin structures using ultrasonography in normal dogs. J Vet Med Sci. 2021;83(9):1472–1475. doi: 10.1292/jvms.21-0086.
- Klucinec B. The effectiveness of the aquaflex gel pad in the transmission of acoustic energy. J Athl Train. 1996;31(4):313–317.
- Tsui BC, Tsui J. A flexible gel pad as an effective medium for scanning irregular surface anatomy. Can J Anaesth. 2012;59(2):226–227. doi: 10.1007/s12630-011-9623-2.
- Woo JW, Kim SK, Park I, et al. A novel gel pad laryngeal ultrasound for vocal cord evaluation. Thyroid. 2017;27(4):553–557. doi: 10.1089/thy.2016.0402.
- Corvino A, Sandomenico F, Corvino F, et al. Utility of a gel stand-off pad in the detection of Doppler signal on focal nodular lesions of the skin. J Ultrasound. 2020;23(1):45–53. doi: 10.1007/s40477-019-00376-3.
- Adler DD, Carson PL, Rubin JM, et al. Doppler ultrasound color flow imaging in the study of breast cancer: preliminary findings. Ultrasound Med Biol. 1990;16(6):553–559. doi: 10.1016/0301-5629(90)90020-d.
- Chen L, Zeng G, Guo D, et al. Soft elastic hydrogel couplants for ultrasonography. Mater Sci Eng C Mater Biol Appl. 2021;119:111609. doi: 10.1016/j.msec.2020.111609.