?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
To compare CO2 laser resection and laryngeal microsurgery for vocal cord polyps and provide evidence for the optimal surgical method.
Methods
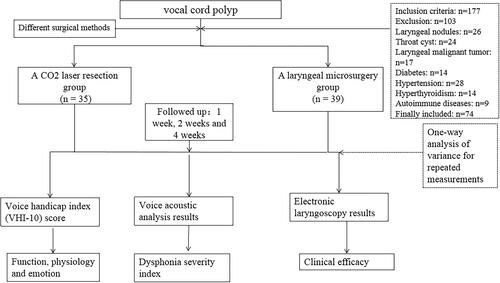
This was a retrospective cohort study that included 74 patients with vocal cord polyps who underwent either CO2 laser resection or laryngeal microsurgery in our hospital from August 2018 to December 2021. According to their preference, 77 patients were divided into two groups: a CO2 laser resection group (n = 35) and a laryngeal microsurgery group (n = 39). Patients were evaluated two days before surgery, and follow-ups were conducted one, two and four weeks after surgery. The voice handicap index (VHI-10) score, voice acoustic analysis results and electronic laryngoscopy results were collected for each patient, and the differences between the two groups were evaluated.
Results
The basic demographic characteristics of the 74 patients were comparable, and all patients completed postoperative follow-up observations. A total of 30 (85.71%) patients in the CO2 laser resection group and 22 (56.41%) patients in the laryngeal microsurgery group were healed. The total effectiveness rate of the CO2 laser resection group (94.29%) was significantly higher than that of the laryngeal microsurgery group (82.05%), and the difference between the two groups was statistically significant (p = .037). Both surgical methods had a positive effect on reducing VHI-10 scores with the effect of CO2 laser resection being more obvious. The difference between the two groups in this regard was statistically significant (p < .001). The effects of each surgical method on the average fundamental frequency perturbation (jitter), amplitude perturbation (shimmer), maximum phonation time and dysphonia severity index were not statistically significant (p > .05).
Conclusion
CO2 laser resection and laryngeal microsurgery have similar effects on voice quality, but CO2 laser resection has higher clinical efficacy.
1. Introduction
Voice functionality plays an important role in human communication and social interaction. A vocal cord polyp is a common benign lesion of the vocal cords that can affect voice quality and cause hoarseness, vocal fatigue, sore throat and other symptoms [Citation1,Citation2]. The main cause of a vocal cord polyp is chronic vocal abuse or overuse, such as excessive shouting, singing, coughing or smoking [Citation3]. Primary clinical symptoms include hoarseness and dysphonia, which can seriously affect the quality of life and work performance of patients [Citation4,Citation5]. A diagnosis of a vocal cord polyp mainly depends on the observations made during laryngeal endoscopy, which can show the location, size, shape and colour of the polyp [Citation6]. The treatment of a vocal cord polyp mainly includes conservative and surgical treatments. Conservative treatment includes voice therapy, medication, lifestyle modification and other methods that can alleviate the symptoms and improve voice quality to some extent [Citation7]. However, for patients with large or persistent polyps, conservative treatment alone is not enough to achieve satisfactory results, and surgical treatment is often required [Citation8].
Surgical treatment of a vocal cord polyp is primarily performed by laryngeal microsurgery or CO2 laser resection. Laryngeal microsurgery is a traditional surgical method that uses a laryngeal knife, scissors and forceps to excise the polyp under a self-retaining laryngoscope [Citation9]. CO2 laser resection is a relatively new surgical method that uses a CO2 laser beam to vaporise and cut the polyp under a suspension laryngoscope [Citation10]. Both methods have advantages and disadvantages. Laryngeal microsurgery has the advantages of low cost, simple operation and good bleeding control. However, it also has some disadvantages, such as a large trauma area, poor visual field and risk of damage to the vocal cord mucosa [Citation11]. Further, CO2 laser resection has the advantages of high precision, minimal trauma, good haemostasis and a clear visual field. However, it also has some disadvantages, such as a high cost, complex operation and the risk of thermal injury to the surrounding tissues [Citation12].
Few studies have compared the clinical efficacy and voice outcomes of these two surgical methods for vocal cord polyps. Therefore, this study aims to compare the clinical efficacy and voice outcomes of CO2 laser resection versus laryngeal microsurgery for vocal cord polyps under a suspension laryngoscope and to provide evidence for choosing the optimal surgical method for vocal cord polyp treatment.
2. Materials and methods
2.1. Study participants
This was a retrospective cohort study that included patients with vocal cord polyps who underwent either CO2 laser resection or laryngeal microsurgery in our hospital from August 2018 to December 2021. The inclusion criteria were as follows: (1) patients aged 18 years or older; (2) patients diagnosed with vocal cord polyps by laryngeal endoscopy; and (3) patients who underwent either CO2 laser resection or laryngeal microsurgery as a first-line treatment. The exclusion criteria were as follows: (1) patients with other laryngeal diseases, such as vocal cord nodules, cysts, papillomas, granulomas or malignancies; (2) patients with systemic diseases, such as diabetes, hypertension, thyroid disorders or autoimmune diseases; and (3) patients who refused to participate or had incomplete outcome data. The study protocol was approved by the ethics committee of our hospital and informed consent was obtained from all participants.
2.2. Surgical method
The operations were performed by two senior otolaryngologists who had similar experience and skills in both surgical methods. Each operator performed half of the operations in each group. The laryngoscope used in this study was a Karl Storz support laryngoscope (Karl Storz SE & Co. KG, Tuttlingen, Germany), and the micromanipulator used for CO2 laser resection was an ExplorENT laryngeal micromanipulator (ExplorENT GmbH, Berlin, Germany). All patients underwent general anaesthesia and endotracheal intubation. The laryngoscope was fixed on a suspension device and inserted into the oral cavity to expose the glottis. The surgical field was adjusted to obtain a clear view of the vocal cords.
For the CO2 laser resection group, a CO2 laser beam (AcuPulse Duo CO2 Laser System, Lumenis Ltd., Yokneam, Israel) with a wavelength of 10.6 μm was delivered through a flexible fibre to the micromanipulator. The output power was set between 1.5–3 W according to the size and location of the polyp. The operator used the micromanipulator to control the direction and focus of the laser beam and vaporised and cut the polyp along the edge of the vocal cord mucosa. The operator also attempted to preserve as much normal mucosa as possible and avoid thermal injury to the surrounding tissue.
For the laryngeal microsurgery group, conventional surgical instruments, such as a laryngeal knife, scissors and forceps, were used to excise the polyp under direct observation. The operator used one hand to fix and pull the polyp to the middle with forceps and used another hand to cut off the polyp with a knife or scissors along the edge of the vocal cord mucosa. The operator also tried to preserve as much normal mucosa as possible and avoid damage to the vocal cord muscle.
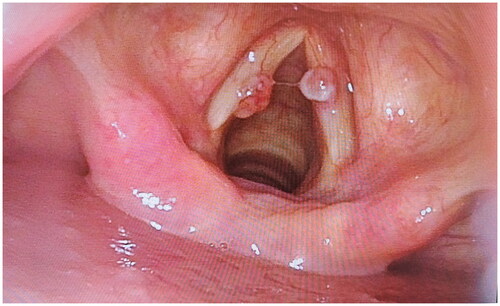
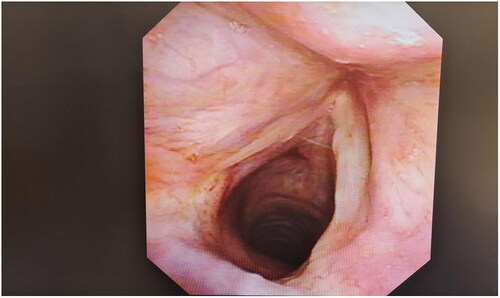
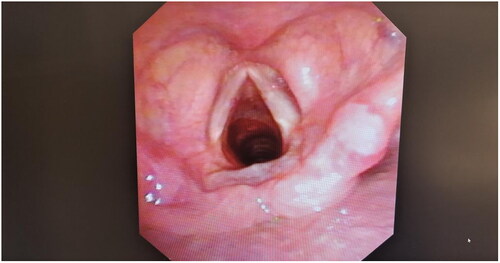
For both groups, epinephrine cotton was applied to compress the wound and stop bleeding after resection. The resected specimens were sent for pathological examination. Patients were instructed to rest for 2 weeks after surgery, with the first week including absolute voice rest and the second-week relative voice rest.To better illustrate the conditions under consideration, shows the vocal cord polyp located at the anterior third junction of the vocal cord before treatment. and depict the same location after undergoing.
2.3. Follow-up and measurement indicators
Patients were evaluated 2 d before surgery, and follow-ups were conducted one, two and four weeks after surgery. During follow-ups, voice handicap index (VHI-10) scores and voice acoustic analysis results were obtained, and electronic laryngoscopy was conducted to evaluate the clinical efficacy of each procedure.
The VHI-10 self-evaluation scale [Citation13,Citation14] is used to assess patients with voice disorders [Citation15]. The scale evaluates the influence of voice on a patient’s life and is divided into three areas, i.e. function, physiology and emotion. Each area comprises 10 questions, and each question receives a score of 0–4 points. The total score ranges from 0–40 points. The higher the score, the greater the degree of influence the patient’s voice has over their life.
All patients underwent voice acoustic detection at 40 dB indoor noise control (Xi ON, DiVAS2.7, Germany). Voice analysis mode was used for the analysis [Citation16]. Before the examination, the patient’s tension was eliminated; they were informed of the correct pronunciation method for the vowel sound and were prompted to keep the mouth microphone 30 cm from the microphone. The vowel | a: | was then continuously issued. Each pronunciation lasted more than 3 s, and the central stable sound segment was selected as a parameter of the test. The average fundamental frequency perturbation (jitter) and amplitude perturbation (shimmer) were calculated for three consecutive tests. The range analysis module was then used to assess the full vocal range, determining both the highest and lowest frequencies the patient could produce. The participants first used the comfortable, daily-use pronunciation of the vowel tone | a: |, and scale intensity was gradually increased until the highest possible scale was achieved. In this manner, the highest fundamental frequency (Fmax) was obtained. The tone was then gradually reduced until the lowest possible scale was attained. The resultant minimum volume (Imin) produced was recorded. The patient was told to continuously and steadily pronounce the | a: | vowel after deep inhalation until they could no longer pronounce it. The patient was detected twice, and the longer pronunciation time was taken as the maximum phonation time (MPT). Dysphonia severity index (DSI) was automatically generated by voice detection software using the following formula: DSI = 0.13 × MPT + 0.0053 × Fmax − 0.26 × Imin − 1.18 × jitter + 12.4 [Citation16,Citation17].
Clinical efficacy was based on electronic laryngoscopy results 4 weeks after surgery [Citation18]. Electronic laryngoscopy is a technique that uses a rigid endoscope with a high-definition camera system (Olympus Corporation, Tokyo, Japan) to capture and store images of the vocal cords. Two experienced otolaryngologists who were blinded to the group allocation independently reviewed the images and rated the healing status of vocal cords according to the following criteria: patients were considered healed if their voice quality returned to normal, their vocal cords were without congestion or swelling, the mucosal surface was smooth and of normal colour and there was normal glottic closure; patients were considered to show markedly effective healing if their voice quality was normal but accompanied by slight hoarseness and a slightly red vocal cord colour; patients were considered to show effective healing if their hoarseness was significantly reduced, there was slight congestion of vocal cords and some swelling and the glottis closed with a small gap; patients were considered to show ineffective healing if there was no significant improvement in voice quality, vocal cords exhibited obvious congestion, there was the presence of hyperplasia or polyp formation and the glottis closed with an obvious gap. The interrater agreement was calculated by Cohen’s kappa coefficient. The total effectiveness rate was calculated as follows: total effectiveness rate = (healed + markedly effective + effective)/sample size × 100.
2.4. Statistical methods
The SPSS Statistics (v. 26.0) software was used for data management and analysis. The count data are described as a frequency (%), and the measurement data are described as mean ± standard deviation (). The t-test or chi-square (χ2) test was used to compare participants with different characteristics. A variance analysis was employed to compare the measurement parameters of the two groups at different points in time, and a non-parametric test was used to compare the clinical efficacy of each procedure. Unless otherwise specified, statistical significance was set at p = .05.
3. Results
3.1. Basic information and characteristics
Among the 177 patients who met the inclusion criteria, 103 patients were excluded for the reasons noted above. Finally, 74 patients were included in this study. According to their preference, 74 patients were divided into two groups: a CO2 laser resection group (n = 35) and a laryngeal microsurgery group (n = 39). shows the flowchart of patient enrollment. The basic demographic characteristics of the 74 patients are shown in . There were no significant differences between the two groups in terms of age, gender, smoking history, drinking history, duration of disease, type/size of the polyp, completion of pre-operative voice therapy and professional voice user/occupation (p > .05).
Table 1. Basic demographic characteristics of 74 subjects.
3.2. Clinical efficacy of each therapeutic method
The clinical efficacy of each procedure 4 weeks after surgery is shown in . A total of 30 (85.71%) patients in the CO2 laser resection group were healed, and 22 (56.41%) patients in the laryngeal microsurgery group were healed. The total effectiveness rate of the CO2 laser resection group (94.29%) was significantly higher than that of the laryngeal microsurgery group (82.05%), and the difference between the two groups was statistically significant (p = .037). The interrater agreement for rating the healing status of vocal cords was good, with a Cohen’s kappa coefficient of 0.81.
Table 2. Clinical effect of CO2 laser and laryngeal microsurgery apparatus in resection of vocal cord polyp.
3.3. The effect of each treatment method on voice handicap index
The VHI-10 scores of the two groups before and after surgery are shown in . The preoperative VHI-10 scores of the two groups were 21.69 ± 0.83 and 22.58 ± 0.94. The VHI-10 scores decreased significantly one week after the operation, even though the patients were on absolute voice rest during this period. This may reflect a subjective improvement of voice quality based on patients’ reduced vocal discomfort and effort. The VHI-10 scores continued to decrease at 2 and 4 weeks after the operation, indicating that patients’ voice function gradually recovered with time. The VHI-10 scores of the CO2 laser resection group were lower than those of the laryngeal microsurgery group at each time point, suggesting that CO2 laser resection had a more obvious effect on relieving the psychological and emotional impact of voice disorders on patients’ lives. The difference between the two groups was statistically significant (p < .001).
Table 3. VHI subjective score results of patients after CO2 laser and laryngeal microsurgery for vocal cord polyps.
3.4. Influence of each treatment method on voice test results
The voice acoustic analysis results of the two groups before and after surgery are shown in . Both surgical methods had a positive effect on improving the voice quality of patients, as measured by jitter, shimmer, MPT and DSI. Compared with the preoperative evaluation results, both CO2 laser resection and laryngeal microsurgery significantly reduced jitter and shimmer and increased MPT and DSI at 1, 2 and 4 weeks after surgery (p < .05). However, there was no significant difference between the two groups in terms of jitter (p = .216), shimmer (p = .385), MPT (p = .551) and DSI (p = .235), indicating that the effects of CO2 laser resection and laryngeal microsurgery on voice acoustic parameters were similar. With the passage of postoperative time, MPT (p = .003) and DSI (p = .033) gradually increased, and their difference was statistically significant. However, there was no correlation between time and surgical method, and the difference was not statistically significant (p > .05).
Table 4. Voice examination results of patients with vocal cord polyps after CO2 laser and laryngeal microsurgery.
4. Discussion
In this study, the authors found that CO2 laser resection under a suspension laryngoscope had higher clinical efficacy than conventional laryngeal microsurgery for vocal cord polyps as measured by the healing status of vocal cords 4 weeks after surgery, which was consistent with the results of some previous studies [Citation18,Citation19]. This may have been due to the advantages of CO2 laser resection, such as high precision, minimal trauma, good haemostasis and a clear visual field [Citation12]. These factors may contribute to more complete removal of polyps and better preservation of vocal cord mucosa, which are essential for voice recovery [Citation20]. Moreover, it was found that both surgical methods had similar effects on improving the voice quality of patients as measured by VHI-10 and voice acoustic analysis, which was in agreement with the findings of other studies [Citation21,Citation22]. This suggests that both methods could effectively restore the vocal function of patients with vocal cord polyps [Citation23]. However, the authors also found that CO2 laser resection had a more obvious effect on reducing VHI-10 scores than laryngeal microsurgery, which contrasted the results of some studies that reported no significant difference between the two methods in terms of VHI-10 scores [Citation24,Citation25]. This may indicate that CO2 laser resection can better relieve the psychological and emotional impact of voice disorders on patients’ lives [Citation26].
Vocal cord polyps is a chronic inflammatory disease of the larynx, which occurs at the edge of one or both vocal cords (mostly in the anterior and middle 1/3 of the vocal cords). The main cause of the disease is long-term improper or excessive use of vocal cords. Smoking and alcoholism are also disease causes [Citation19]. The anatomical location of vocal cord polyps is complex and is more common at the edge and surface of the vocal cords. It can present as translucent, white or pink tissue hyperplasia. The surface of polyps is smooth and both sides of the polyp can be simultaneously observed. Most vocal cord polyps will affect pronunciation after formation, and after the appearance of polyps, conservative treatment alone cannot significantly inhibit their further growth. Excision is the main treatment for vocal cord polyps [Citation20]. The key to evaluating the success of surgical treatment is to assess the patient’s VHI and voice acoustic analysis results and use an electronic laryngoscope to evaluate the patient’s clinical efficacy [Citation21,Citation22].
The mechanism of CO2 laser treatment is to vaporise and cut diseased tissue through the thermal effect of a laser, which has the benefits of high precision and a small trauma area. Vocal cord polyps directly affect a patient’s voice and normal life; the accuracy and thoroughness of polyp resection will directly affect the patient’s postoperative voice [Citation23]. Prior research has juxtaposed conventional cold instrument resection with CO2 laser resection for benign vocal cord lesions. The consensus suggests that both surgical methods have comparable efficacy, with patients experiencing notable postoperative recovery improvements after undergoing either method [Citation24]. Conversely, some researchers believe that laser resection may cause thermal damage and affect postoperative recovery. Studies have shown that, with increased power, the degree of thermal damage caused by CO2 laser microsurgery increases, along with the recovery time of surgical wounds [Citation25]. Therefore, strict control of output power is key to successful laser surgery. In this study, the output power was between 1.5–3 W; the attending doctor adjusted the output power during the operation as the situation demanded. The smaller output power used in this study may account for the positive postoperative recovery of patients with vocal cord polyps who underwent this procedure. Remacle et al. [Citation26] employed micro-CO2 laser treatment at 3 W for 251 patients with benign vocal cord lesions, observing marked enhancements in haemostasis and the visual field range.
There were some limitations to this study. First, the outcome of clinical efficacy was based on an unvalidated scale that was inconsistently explained and applied, which may have introduced some bias and uncertainty in the results. Second, because patients have the right to know about the surgical procedures before surgery and to choose the surgical procedure, patients and their families were grouped according to their wishes, and there was no randomisation of the study participants. Therefore, there may be a confounding bias between the two groups. Third, due to the limitations of the research conditions, this study was primarily carried out in the treating hospital, and participants from multiple centres were not screened. This may have resulted in the research results being non-representative of the general population.
5. Conclusion
In conclusion, CO2 laser resection under a suspension laryngoscope and conventional laryngeal microsurgery have similar effects on improving the voice quality of patients with vocal cord polyps, but the clinical efficacy of CO2 laser resection is higher. Due to the limitations of this study, more high-quality, multi-centre studies with larger sample sizes are needed to further confirm its conclusions.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Zhumadian Central Hospital of Henan Province. We obtained signed informed consent from the participants/legal guardians in this study.
Disclosure statement
No potential competing interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article.
Additional information
Funding
References
- Pestana PM, Vaz-Freitas S, Manso MC. Prevalence of voice disorders in singers: systematic review and meta-analaysis. J Voice. 2017;31(6):1–8. doi: 10.1016/j.jvoice.2017.02.010.
- Sanssené C, Bardi J, Welby-Gieusse M. Prevalence and risk factors of voice disorders in French tour guides. J Voice. 2020;34(6):911–917. doi: 10.1016/j.jvoice.2019.05.002.
- Trinite B. Epidemiology of voice disorders in Latvian school teachers. J Voice. 2017;31(4):508.e1–508.e9. doi: 10.1016/j.jvoice.2016.10.014.
- Xiang X. Retrospective clinical study of CO2 laser microsurgery with self-retaining laryngoscope for laryngeal neoplasms. Shandong University; 2016.
- Zhang Y, Liang G, Sun N, et al. Comparison of CO2 laser and conventional laryngomicrosurgery treatments of polyp and leukoplakia of the vocal fold. Int J Clin Exp Med. 2015;15;8(10):18265–18274.
- Li LH, Hu WP, Zhang ZL, et al. The adhesion separation operation with CO2 laser combined with triamcinolone acetonide vocal cord submucosal injection for the treatment to vocal cord adhesion. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017;31(9):700–702. doi: 10.13201/j.issn.1001-1781.2017.09.013.
- King RE, Dailey SH, Thibeault SL. Role of voice therapy in adherence to voice rest after Office-Based vocal fold procedures. Am J Speech Lang Pathol. 2021;30(6):2542–2553. doi: 10.1044/2021_AJSLP-21-00082.
- He F, Wang Y, Chen W, et al. Clinical reseach of early laryngocarcinoma treatment by carbon dioxide laser microsurgery. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2014;28(7):493–495.
- Sataloff RT, Spiegel JR, Hawkshaw M, et al. Laser surgery of the larynx: the case for caution. Ear Nose Throat J. 1992;71(11):593–595. doi: 10.1177/014556139207101112.
- Devaiah AK, Shapshay SM, Desai U, et al. Surgical utility of a new carbon dioxide laser fiber: functional and histological study. Laryngoscope. 2005;115(8):1463–1468. doi: 10.1097/01.mlg.0000171021.73635.3b.
- Choi SS, Cotton RT. Surgical management of voice disorders. Pediatr Clin North Am. 1989;36(6):1535–1549. doi: 10.1016/s0031-3955(16)36805-5.
- Benninger MS. Microdissection or microspot CO2 laser for limited vocal fold benign lesions: a prospective randomized trial. Laryngoscope. 2000;110(2 Pt):1–17. doi: 10.1097/00005537-200002001-00001.
- Rosen CA, Lee AS, Osborne J, et al. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549–1556. doi: 10.1097/00005537-200409000-00009.
- Wen X, Hongyan L, Rong H, et al. Reliability and validity evaluation of voice handicap index scale Chinese version. Chin J Otorhinolaryngol Head Neck Surg. 2008;09:670–675.
- Zhang WN, Tang AZ, Xu ZW, et al. Analysis of VHI subjective assessment and DSI voice test in patients with vocal cord polyp before and after operation. J Audiol Speech Pathol. 2013;5:494–496. doi: 10.3969/j.issn.1006-7299.2013.05.015.
- Wu XF, Xu JJ, Qiao MZ, et al. The voice acoustic analysis of patients with laryngopharyngeal reflux disease. J Audiol Speech Pathol. 2012;20(3):221–224. doi: 10.3969/j.issn.1006-7299.2012.03.08.
- Wuyts FL, De Bodt MS, Molenberghs G, et al. The dysphonia severity index: an objective measure of vocal quality based on a multiparameter approach. J Speech Lang Hear Res. 2000;43(3):796–809. doi: 10.1044/jslhr.4303.796.
- Yang C. Curative effect evaluation of carbon dioxide laser resection under self-retaining laryngoscope in the treatment of vocal cord polyp. China J Endoscopy. 2016;22(7):18–21. doi: 10.3969/j.issn.1007-1989.2016.07.005.
- Lechien JR, Chiesa-Estomba CM, Hans S, et al. Laryngopharyngeal reflux and vocal fold polyps. Am J Otolaryngol. 2021;42(2):102833. doi: 10.1016/j.amjoto.2020.102833.
- Zhang HL, Ding HF, Sun W, et al. Clinical effect of nasal endoscope combined with supporting laryngoscope surgery in the treatment of polyps of vocal cord and its influence on voice function of patients. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2019;33(3):272–274. PMID: 30813701. doi: 10.13201/j.issn.1001-1781.2019.03.021.
- Mobarsa V, Samdani SK, Gurjar VS. Outcome analysis of microlaryngeal surgery for benign lesions of vocal cord using videostroboscopy and voice handicap index. Indian J Otolaryngol Head Neck Surg. 2019;71(Suppl 1):327–332. doi: 10.1007/s12070-018-1300-0.
- Muslih I, Herawati S, Pawarti DR. Association between voice handicap index and praat voice analysis in patients with benign vocal cord lesion before and after microscopic laryngeal surgery. Indian J Otolaryngol Head Neck Surg. 2019;71(Suppl 1):482–488. doi: 10.1007/s12070-018-1363-y.
- Xidong C, Xia Z, Chenjie X, et al. Management of difficult suspension laryngoscopy using a GlideScope® video laryngoscope. Acta Otolaryngol. 2012;132(12):1318–1323. doi: 10.3109/00016489.2012.703326.
- Hörmann K, Baker-Schreyer A, Keilmann A, et al. Functional results after CO2 laser surgery compared with conventional phonosurgery. J Laryngol Otol. 1999;113(2):140–144. doi: 10.1017/s0022215100143397.
- Peng LH. Curative effect analysis of supporting laryngoscope combined with nasal endoscopic surgery in treatment of vocal cord leukoplakia. J Med Inform. 2016;29(16):47–48. doi: 10.3969/j.issn.1006-1959.2016.16.037.
- Remacle M, Lawson G, Watelet JB. Carbon dioxide laser microsurgery of benign vocal fold lesions: indications, techniques, and results in 251 patients. Ann Otol Rhinol Laryngol. 1999;108(2):156–164. doi: 10.1177/000348949910800210.