Abstract
Purpose
To investigate the alterations in biometric parameters among Chinese adolescents over an extended period of wearing orthokeratology lenses, as well as the subsequent changes after a one-month cessation of lens usage prior to the secondary lens fitting.
Methods
Twenty-four myopic patients aged 7–14 were enrolled in this 37-month prospective observational study. Ocular biometric parameters were measured in the study. Ocular biometric parameters were assessed, and the utilization of Generalized Estimating Equations (GEE) was employed in the analysis to address the correlation between the two eyes of each participant.
Results
The axial length (AL) increased by 0.55 mm after 36 months of lens wearing and further increased to 0.62 mm at the 37-month follow-up compared to the initial measurement. The differences in AL elongation per month between the 37-month time point and the 12-, 24-, and 36-month marks of lens wearing were found to be statistically significant (p12-month = 0.001; p24-month = 0.003; p36-month = 0.001). Following the cessation of lens wear for 1 month, there was no significant complete recovery observed in the flat and steep keratometry values. However, the intraocular pressure and anterior chamber depth returned to their baseline levels.
Conclusions
The AL elongation undergoes alterations during temporary discontinuation of lenses, with the flat and steep keratometry measurements remaining significantly flatter compared to the baseline. However, the intraocular pressure and anterior chamber depth return to their initial levels after one month of lens cessation.
Introduction
Myopia is a highly prevalent ocular disorder on a global scale [Citation1,Citation2], and it is associated with an elevated susceptibility to other ocular diseases [Citation3–7]. The recognition of the substantial burden and pathological consequences resulting from the progression of myopia has motivated our investigation into diverse interventions aimed at managing its progression [Citation8,Citation9]. Studies have demonstrated the advantageous effects of orthokeratology (ortho-k) lenses in slowing down the progression of myopia among adolescents [Citation8,Citation10].
The efficacy of ortho-k lenses has been extensively documented [Citation11]. However, in order to ensure the effectiveness of myopia control, individuals who wear ortho-k lenses tend to wear them for an extended period of time [Citation12,Citation13]. In China, it is common for ophthalmologists and optometrists to advise ortho-k lens wearers to discontinue lens use for approximately one month prior to transitioning to a new pair of lenses. This practice allows for adjustments to be made to the parameters of the ortho-k lenses based on individual eyeball parameters, thereby ensuring the efficacy of myopia control.
A scarcity of prospective studies exists regarding the changes in ocular biometric parameters during the 37-month follow-up period subsequent to a 1-month cessation of lens wear, despite previous research documenting varying durations for the complete or incomplete recovery of refractive error [Citation14–16], corneal topography [Citation16–18], corneal thickness [Citation19], corneal epithelium [Citation20,Citation21], and other parameters [Citation22]. It is imperative for clinicians to acknowledge the alterations in biometric parameters that occur during extended lens wear and the one-month cessation period, as this is vital for the accurate assessment of said parameters and subsequently informing the prescription of future ortho-k lenses.
The objective of this study was to examine the alterations in biometric parameters, such as axial length, anterior chamber depth, intraocular pressure, and corneal keratometry, among Chinese adolescents aged 7–14 years throughout an extended period of wearing ortho-k lenses, as well as during the subsequent 1-month period after lens discontinuation. Additionally, the study sought to investigate the potential occurrence of a ‘rebound’ effect following the cessation of long-term ortho-k lens usage.
Methods
Study design
This study was a prospective observational study, and each participant served as her/his control. The current study is a sequel to a study by Chen et al. [Citation23], this study includes 3-year data from the same cohort as the 2-year study reported by Chen et al. This study was conducted following the tenets of the Declaration of Helsinki and approved by the Ethics Committee of West China Hospital, Sichuan University, Chengdu, China. All participants were 7–14 years old and enrolled in the Contact Lenses clinic of West China Hospital, Sichuan University, between 2017 and 2018. All the participants or their guardians signed written informed consent before participation in the study.
The present study comprised individuals between the ages of 7 and 14 who exhibited myopia ranging from −1.00 diopters (D) to −5.00D, accompanied by astigmatism not exceeding 1.50D. Adherence to prescribed protocols and consistent attendance at follow-up appointments were deemed crucial. Participants with contraindications to contact lens usage, severe allergies to cycloplegia drugs (specifically compound tropicamide eye drops) or contact lens care solution, as well as those with other ocular or general ailments, were excluded from the study.
Lenses fitting procedures
All participants in this study were fitted with the ortho-k lenses of the identical brand to mitigate disparities and influences arising from diverse brands, thereby minimizing variations in measurements attributable to dissimilar lens designs. The lenses were Euclid VST designs (Euclid Systems Corporation, Herndon, VA, USA). The lens fitting procedures strictly adhered to the manufacturer’s guidelines (Euclid Systems Corp.) Additionally, as per the West China Hospital’s regulatory lens fitting protocols, all participants and their parents were educated on standard ortho-k lens aftercare procedures, as detailed in the preceding study [Citation23].
Follow-up timeline
The participants underwent consistent measurements conducted by the same examiner during each subsequent visit. The measurements were recorded at the beginning of the study and at various intervals (1, 3, 6, 12, 18, 24, 30, and 36 months) after wearing ortho-k lenses. Additionally, measurements were taken at the 37-month mark, following a one-month period of not wearing the lenses.
Measurements
The detailed measurement methods and instruments have been described in our previous study [Citation23]. The baseline spherical equivalent refraction (SER) was documented following the administration of cycloplegia. Cycloplegia was induced through the administration of one drop of 1% tropicamide (compound tropicamide eye drops, Shenyang Sinqi, sinqi.com) into each eye, with four repetitions at 5-min interval. A minimum resting period of 20 min was observed prior to achieving cycloplegia. The measurements of keratometry (K), encompassing flat keratometry (Flat K), steep keratometry (Steep K), corneal astigmatism (CA) (Tomey TMS-4, tomey.com), axial length (AL), anterior chamber depth (ACD) (ZEISS IOL Master 500, zeiss.com), and intraocular pressure (IOP) (Canon TX-20, Canon Medical Systems, eu.medical.canon), were conducted. All participants underwent assessment utilizing the specified instruments to determine the aforementioned parameters.
Statistical analysis
SPSS 22.0 and GraphPad Prism 8.0 software were used for statistical analyses. Normality was tested using the Shapiro–Wilk normality test, and variables were expressed as means (standard deviation) or medians with the interquartile range (Q1, Q3), as appropriate. The repeated measurement design reveals a correlation among the responses of individual participants, necessitating the consideration of this correlation for accurate inferences. In the present analysis, Generalized Estimating Equations (GEE) were employed to address the correlation between the responses of both eyes from the same participant. The significance of the Both Eyes × Times interactions in each analysis was determined using an analysis of Wald tests. Differences in ocular biometric parameters of participants were determined within follow-up time points relative to baseline using GEE models followed by Bonferroni correction.
Results
A cohort of 24 individuals were initially recruited for this research endeavour. However, a subset of five participants opted to withdraw from the study within the 12- and 24-month periods. The reasons for their departure included relocation outside the city (2 individuals) and a preference to revert back to spectacle lens usage due to demanding academic commitments and other personal factors (3 individuals). Consequently, the final analysis encompassed the data from the remaining 19 participants, corresponding to a total of 38 eyes, over a span of 37 months.
The baseline data of the participants are presented in . The participants’ age ranged from 7 to 14 years, the mean values of the binocular SER were −2.53 D in the right eye and −2.45 D in the left eye, respectively.
Table 1. Demographics of both eyes in participants at baseline.
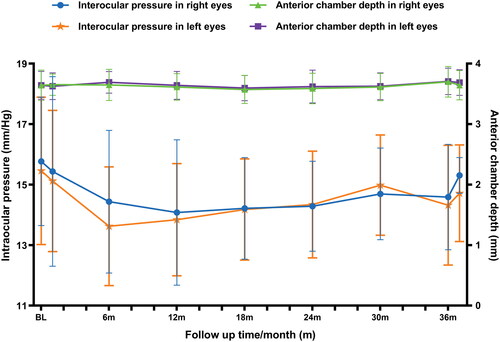
The changes in corneal keratometry changes, specifically flat K, steep K, and CA changes, were observed in both eyes of the participants over a 37-month follow-up period, as depicted in . The Both Eyes × Times interactions of corneal keratometry did not yield statistically significant results (flat K: Wald’s χ2 = 1.00, p > 0.99; steep K: Wald’s χ2 = 3.14, p = 0.93; CA: Wald’s χ2 = 4.13, p = 0.84). provides a comprehensive overview of the differences in corneal keratometry values at each time point compared to the baseline, spanning 36 months of lens-wearing and an additional month after lens cessation (at the 37-month time point).
Figure 1. The corneal keratometry (a). Flat keretyometry; (b). Steep keratometry; (c). Corneal astigmatism) in both eyes of participants in the follow-up time, including the 37-month time point following 1 month of lens cessation.
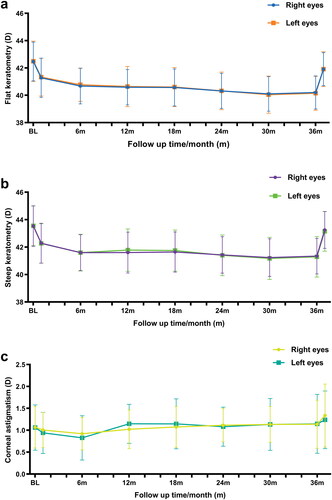
Table 2. The estimates and differences between the baseline measurement and each subsequent follow-up time point of the corneal keratometry in participants during the 37 months follow-up period.
The results of the study indicate that there was a significant decrease in flat K values after one month of wearing ortho-k lenses. This reduction remained consistent over the course of 37 months of lens wear (p < 0.0001). The difference in flat K values between the baseline and the 37-month time point was 0.56D, while the difference at the 36-month time point was 2.30D. Similarly, steep K exhibited a similar changing trend as flat K (p < 0.0001). The difference in steep K values between the baseline and the 36-month time point was 2.23D, while the difference at the 37-month time point was 0.34D. It is noteworthy to mention that neither the flat K nor the steep K values exhibited significant recovery after the cessation of lens wear for one month (flat K: p < 0.0001; steep K: p = 0.008), although the values at that time point were closed to the baseline level. Furthermore, the values of CA showed a trend of increase compared to the baseline value, but these changes were not statistically significant (.).
The significant Both Eyes × Times interactions of AL and AL elongation per month were not observed (AL: Wald’s χ2 = 6.46, p = 0.60; AL elongation per month: Wald’s χ2 = 6.35, p = 0.50). presents the mean differences in AL between the baseline and subsequent time points. The results indicate a significant increase in AL among participants after wearing ortho-k lenses, which remained stable at the 36-month mark and the 37-month follow-up, occurring one month after lens cessation. Specifically, the AL elongation after 36 months of lens wearing was measured at 0.55 mm, while it reached 0.62 mm at the 37-month follow-up, both compared to the baseline. Furthermore, the AL elongation between the measurement taken after 36 months and the 1-month lens cessation was found to be 0.068 mm.
Table 3. The estimates and differences between the baseline measurement and each subsequent follow-up time point of the axial length in participants during the 37 months follow-up period.
The changes in AL and the monthly elongation of AL in the context of the AL elongation trends were visually represented in . Following a period of 36 months of lens wear, the cumulative AL elongation amounted to 0.55 mm, with an average annual AL elongation of 0.183 mm over the course of 3 years. Specifically, the AL elongation during the initial month was measured at 0.026 mm, which subsequently decreased to 0.015 and 0.017 mm per month at the 36-month and 37-month intervals of lens wear, respectively. In comparison to the monthly AL elongation at 1 month, the values observed at the subsequent time points within the sequence did not exhibit statistical significance (p > 0.9). Nevertheless, a notable distinction was observed between the 36- and 37-month time points, with a mean difference of 0.001D/month (p = 0.007).
Figure 2. The change in axial length and the axial length elongation per month in both eyes of participants in the follow-up time, including the 37-month time point following 1 month of lens cessation. Bars represent the mean value; error bars represent the standard deviations (SD) of the mean.
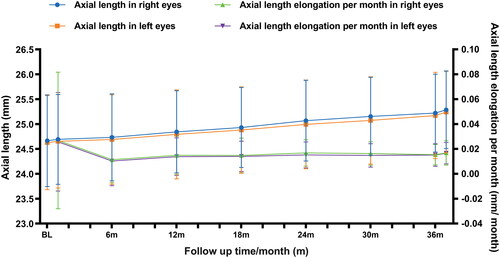
The binocular values of AL elongation per month in each year, relative to the previous year, are presented in . Specifically, the monthly AL elongation at the 12-month mark compared to baseline was 0.014 mm/month, at the 24-month mark compared to the 12-month mark was 0.018 mm/month, at the 36-month mark compared to the 24-month mark was 0.014 mm/month and at the 1-month lens cessation compared to the 36-month mark was 0.068 mm/month. Notably, the differences between the value at the 37-month time point and the 12-, 24-, and 36-months lens wearing were found to be statistically significant (p12-month = 0.001; p24-month = 0.003; p36-month = 0.001).
Figure 3. Ocular axial length elongation per month in each year compared with the previous year during the 37-month follow-up period. Bars represent the mean value; error bars represent the standard deviations (SD) of the mean.
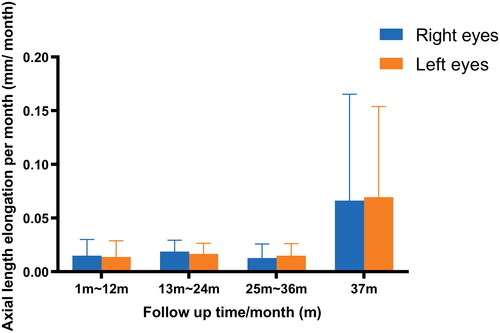
shows the changes in IOP and ACD of the lens wearers during the 37-month follow-up period. The Both Eyes × Times interactions of these parameters did not reach significances (IOP: Wald’s χ2 = 8.21, p = 0.41; ACD: Wald’s χ2 = 5.08, p = 0.75). The alterations in the IOP of the participants exhibited a slight level of significance, with the mean value at the 36-month time point demonstrating a significant deviation from the baseline data (p < 0.0001). Conversely, no significant differences were observed between the 37-month time point and baseline, as well as between the 36-month time point and baseline (p > 0.99). The mean ACD displayed an increase of 0.061 and 0.023 mm at the 36- and 37-month time points, respectively, in comparison to the baseline measurement. However, these changes did not reach statistical significance. Furthermore, the ACD exhibited a notable reduction of 0.038 mm when comparing the measurement obtained at the 37-month time point to that of the 36-month time point (p = 0.032).
Discussion
In China, it is a customary practice for optometrists to advise long-term lens wearers to abstain from using overnight ortho-k lenses for a duration of 30–40 days prior to transitioning to a new pair of lenses. This recommendation aims to facilitate a more accurate fitting effect on the progression of the eyeball and enhance the effectiveness of myopia control. Given the established safety of long-term overnight lens wear [Citation10,Citation12,Citation24], it is prevalent for lens wearers to prolong their usage of such lenses. In order to adequately assess the reversibility of binocular biometric parameters, it is crucial to carefully manage the changes and reversibility of these parameters during the cessation of lens wear for a duration of one month. This research study presents the alterations and reversibility of AL, flat K, steep K, CA, ACD, and IOP throughout a 37-month follow-up period, followed by a one-month period of lens cessation.
The average AL elongation per year in this study (0.18 mm/year) was found to be lower than the findings of a Japanese study involving participants aged 8-12 years [Citation25] and a Spanish study involving participants aged 6-12 years (0.23 mm/year) [Citation26]. Conversely, it was higher than the reported results of a meta-analysis summarizing eight studies from various ethnic groups (0.135 mm/year) [Citation24] and in a Denmark study involving participants aged 6–12 years (0.137 mm/year) [Citation27]. These findings from the current study indicate that the elongation of AL after ortho-k varies among different ethnic groups; however, the underlying reasons for this variability remain unclear. The current study discovered that there was no significance in AL elongation per month at the 36-month follow-up. However, it was observed that the AL elongation per month at the 37-month time point was higher than the average of the preceding 36 months, suggesting the possibility of a ‘rebound’ effect following the discontinuation of Ortho-k lens usage [Citation28–30]. This finding holds significant implications for the extended clinical application of ortho-k as a means of managing myopia in children and adolescents, particularly regarding the duration of ortho-k lens wear. In light of the concerns voiced by both lens wearers and their parents regarding the extensive time commitment and intricate lens care involved with ortho-k lenses, particularly among Chinese adolescents aged 15 to 18 who need to allocate additional study time for the Chinese College Entrance Examination, it is customary for both adolescents and their parents to prioritize the use of spectacle glasses or alternative approaches that demand less time and effort for maintenance. The findings of our study indicate that wearing ortho-k lenses at least for a duration of 36 months is insufficient for effectively managing stable AL elongation. Nevertheless, further investigation is required to determine the ideal length of time for lens wear and to evaluate the effectiveness of alternative approaches to myopia control in achieving stabilization and mitigating rebound effects.
In the present study, it was observed that there were no statistically significant alterations in the ACD of the participants following the discontinuation of long-term ortho-k lenses. Previous studies have indicated that the ACD of individuals who engage in long-term ortho-k lens wear may undergo changes, albeit not of significant magnitude [Citation31–33]. This phenomenon can be attributed to the elongation in AL and vitreous chamber depth, resulting in a reduction in lens thickness and an increase in ACD. Notably, this effect is more pronounced in myopic individuals when compared to hyperopic and emmetropic individuals [Citation34–39]. In this study, the observed alterations in ACD were insignificant. This implies that ortho-k may potentially exert an influence on the internal ocular structure, as evidenced by the observed increase in AL following prolonged ortho-k lens usage, while ACD remained unchanged [Citation33]. Nonetheless, the precise mechanisms underlying these phenomena mechanisms have yet to be fully elucidated.
As previously demonstrated, the reversal of corneal topography following the cessation of ortho-k lens cessation has been established [Citation15–17,Citation20,Citation21,Citation30,Citation40]. Nevertheless, there is currently no reported data from a 37-month prospective study regarding the recovery of corneal keratometry in ortho-k lens wearers after 36 months and the subsequent 1-month lens cessation. The current study reveals that significant changes in flat K occurred within the first month of lens wear, persisting for 3 months from the baseline measurement and maintaining stability thereafter until 36 months mark. A similar trend of changes in steep K was observed throughout the 36-month follow-up period. This phenomenon implies that the effect of ortho-k on corneal topography gradually stabilizes after 3 months of lens usage, offering guidance for determining suitable time intervals for clinical assessment of these ocular parameters.
It is noteworthy to mention that following the discontinuation of the 1-month lens, the flat and steep K values remained significantly different from the baseline measurements. This finding contradicts the study conducted by Soni et al. [Citation16], where they utilized horizontal and vertical corneal curvature as the index instead of flat K and steep K. Additionally, the duration of lens wear in their study was shorter than that in the present study, and there were variations in the degrees of myopia between these studies. Previous studies demonstrated a significant correlation between keratometry measurements taken 1 week to 1 month after lens cessation and baseline measurements [Citation17,Citation32,Citation41–44]. Notably, these studies have provided clinical evidence indicating that flat K values tend to be flatter after the lens cessation compared to baseline measurement. The extent of recovery may be influenced by factors such as lens-wear duration [Citation41], lens decentration [Citation17] or the corneal biomechanics [Citation45]. Furthermore, it has been reported that changes in corneal keratometry may serve as a potential predictor for AL elongation in individuals wearing ortho-k lenses [Citation46].
However, these conjectures are founded upon varying study methodologies, such as retrospective studies, necessitating further inquiries to substantiate the comparative impact. Throughout the entire duration of the follow-up, corneal astigmatism exhibited insignificant changes, although certain studies documented contradictory findings [Citation17,Citation41]. The dissimilar outcomes may be attributed to variations in participant ages and degrees of myopia, as well as the critical factor of lens wear duration. Hence, the present study has observed that the restoration of both flat and steep K values after a one-month cessation period was inadequate in comparison to the baseline values. This underscores the need for further study to ascertain whether a prolonged cessation of ortho-k lens usage can lead to a comprehensive restoration of corneal topography in a distinct group of adult individuals who wear ortho-k lenses. Subjecting myopic children to greater increases in axial length without continuing ortho-k is not feasible for practical clinical application.
The preceding study documented a higher IOP in individuals with myopia compared to those with emmetropia [Citation47]. Given the association between IOP and both the ciliary body and ACD, which can potentially impact accommodation function, it is plausible that further associations exist between IOP and the progression of myopia [Citation47,Citation48]. This study demonstrates a slight decrease in IOP over the course of 36 months of lens wear, which aligns with previous research findings [Citation49, Citation50], and the observed decrease in IOP may be attributed to changes in central corneal thickness [Citation49]. Additionally, the study reveals that the IOP at the 37-month mark did not significantly differ from the baseline, indicating a recovery of IOP after 1 month of lens cessation. These findings further support the impact of ortho-k IOP changes. However, the exact mechanism by which ortho-k influences IOP remains unknown and requires further investigation.
The exact timeframe for the complete restoration of binocular biometric parameters remains uncertain. A prior investigation indicated that in adults, these parameters can recover to the baseline level after 72 h [Citation14], 1 week [Citation15] or 2 weeks [Citation16] of ortho-k lens wear. Nevertheless, disparities exist between adults and adolescents, as other studies have reported differing durations of lens discontinuation required for the full recovery of binocular biometry. Furthermore, it is imperative to emphasize the significant contribution of parents in determining the overall effectiveness of the fitting and lens wearing procedure. Additionally, future research should incorporate a systematic analysis to investigate the concerns and awareness of parents regarding the impact of ortho-k and other methods of myopic control when discontinuation becomes inevitable.
The current study is subject to several notable limitations. Firstly, the sample size employed in this investigation was relatively small. However, it is important to note that the GEE model was utilized to analyse the data obtained from repeated measurements of binocular biometric parameters throughout the follow-up period. This approach facilitated the inclusion of data from both study eyes of each participant, thereby enhancing the comprehensiveness of the analysis.
Furthermore, it is imperative to enhance the representativeness of the study. To achieve this, a larger sample size and international comparison studies should be conducted in the future. These measures would serve to validate the findings in a comprehensive manner, thereby augmenting their utility and applicability.
In conclusion, the study determined that AL elongation does exhibit alterations during short-term lens cessation. The ACD, however, remained stable throughout the 37-month follow-up period. Additionally, the IOP demonstrated a minor decline over the course of 36 months of lens usage, followed by a recovery to the baseline value after 1 month of lens cessation. The present study further demonstrates that the impact of ortho-k on corneal topography gradually stabilizes after 3 months of lens usage. Additionally, even after discontinuing lens wear for 1 month, both the flat and steep keratometry measurements remained significantly different from the baseline measurements.
The aforementioned conclusions have the potential to offer clinicians and ophthalmologists with valuable reference and evaluation of ocular biometric parameters for estimating ortho-k lens fitting parameters. Additionally, it is crucial for them to comprehend the impact of discontinuing ortho-k lenses on other ocular biometric parameters when considering changes in ortho-k lenses.
Authorship contribution statement
XC and LL contributed to the conception and design of the study. XC, BY, XW, and WM collected the samples and organized the database. XC performed the statistical analysis. XC wrote the first draft of the manuscript. LL was responsible for the data administration and supervised, guided this study. All authors contributed to manuscript revision, read, and approved the submitted version.
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data statement
The data that support the findings of this study are available from the corresponding author, Longqian Liu, upon reasonable request.
Additional information
Funding
References
- Burton MJ, Ramke J, Marques AP, et al. The lancet global health commission on global eye health: vision beyond 2020. Lancet Glob Health. 2021;9(4):1–10. doi: 10.1016/S2214-109X(20)30488-5.
- Sankaridurg P, Tahhan N, Kandel H, et al. IMI impact of myopia. Invest Ophthalmol Vis Sci. 2021;62(5):2. doi: 10.1167/iovs.62.5.2.
- Biswas S, Biswas P. Longitudinal evaluation of the structural and functional changes associated with glaucoma in myopia. Optom Vis Sci. 2020;97(6):448–456. doi: 10.1097/OPX.0000000000001519.
- Gabriel M, Großpötzl M, Wallisch F, et al. In-depth analysis of risk factors for pseudophakic retinal detachments and retinal breaks. Acta Ophthalmol. 2022;100:e694–e700.
- Khatwani N, Makhija S, Ahuja A. Clinical profile and distribution of peripheral retinal changes in myopic population in a hospital-based study in North India. Indian J Ophthalmol. 2022;70(4):1280–1285. doi:10.4103/ijo.IJO_946_21.
- Sun MT, Tran M, Singh K, et al. Glaucoma and myopia: diagnostic challenges. Biomolecules. 2023;13(3):562. doi: 10.3390/biom13030562.
- Chong RS, Li H, Cheong AJY, et al. Mendelian randomization implicates bidirectional association between myopia and primary Open-Angle glaucoma or intraocular pressure. Ophthalmology. 2023;130(4):394–403. doi: 10.1016/j.ophtha.2022.11.030.
- Wolffsohn JS, Flitcroft DI, Gifford KL, et al. IMI - Myopia control reports overview and introduction. Invest Ophthalmol Vis Sci. 2019;60(3):M1–M19. doi: 10.1167/iovs.18-25980.
- Lanca C, Pang CP, Grzybowski A. Effectiveness of myopia control interventions: a systematic review of 12 randomized control trials published between 2019 and 2021. Front Public Health. 2023;11:1125000. doi: 10.3389/fpubh.2023.1125000.
- Bullimore MA, Johnson LA. Overnight orthokeratology. Cont Lens Anterior Eye. 2020;43(4):322–332. doi: 10.1016/j.clae.2020.03.018.
- Zhu Z, Chen Y, Tan Z, et al. Interventions recommended for myopia prevention and control among children and adolescents in China: a systematic review. Br J Ophthalmol. 2023;107(2):160–166. doi: 10.1136/bjophthalmol-2021-319306.
- Hiraoka T, Sekine Y, Okamoto F, et al. Safety and efficacy following 10-years of overnight orthokeratology for myopia control. Ophthalmic Physiol Opt. 2018;38(3):281–289. doi: 10.1111/opo.12460.
- Ma L, Xu M, Wang J, et al. Analysis of the reasons for the discontinuation of orthokeratology lens use: a 4-Year retrospective study. Eye Contact Lens. 2022;48(8):335–339. doi: 10.1097/ICL.0000000000000910.
- Barr JT, Rah MJ, Meyers W, et al. Recovery of refractive error after corneal refractive therapy. Eye Contact Lens. 2004;30(4):247–251. discussion 63-4. doi: 10.1097/01.icl.0000140234.85617.88.
- Hiraoka T, Okamoto C, Ishii Y, et al. Recovery of corneal irregular astigmatism, ocular higher-order aberrations, and contrast sensitivity after discontinuation of overnight orthokeratology. Br J Ophthalmol. 2009;93(2):203–208. doi: 10.1136/bjo.2007.136655.
- Soni PS, Nguyen TT, Bonanno JA. Overnight orthokeratology: refractive and corneal recovery after discontinuation of reverse-geometry lenses. Eye Contact Lens. 2004;30(4):254–262. discussion 63-4. doi: 10.1097/01.icl.0000140637.58027.9b.
- Chen Z, Zhou J, Xue F, et al. Increased corneal toricity after Long-Term orthokeratology lens wear. J Ophthalmol. 2018;2018:7106028. doi: 10.1155/2018/7106028.
- Kobayashi Y, Yanai R, Chikamoto N, et al. Reversibility of effects of orthokeratology on visual acuity, refractive error, corneal topography, and contrast sensitivity. Eye Contact Lens. 2008;34(4):224–228. doi: 10.1097/ICL.0b013e318165d501.
- Wan K, Yau HT, Cheung SW, et al. Corneal thickness changes in myopic children during and after short-term orthokeratology lens wear. Ophthalmic Physiol Opt. 2021;41(4):757–767. doi: 10.1111/opo.12824.
- Zhao L, Jing L, Li J, et al. Changes in corneal densitometry after long-term orthokeratology for myopia and short-term discontinuation. PLoS One. 2022;17(2):e0263121. doi: 10.1371/journal.pone.0263121.
- Kang P, Swarbrick H. Discontinuation of long term orthokeratology lens wear and subsequent refractive surgery outcome. Cont Lens Anterior Eye. 2017;40(6):436–439. doi: 10.1016/j.clae.2017.07.001.
- Li Z, Hu Y, Cui D, et al. Change in subfoveal choroidal thickness secondary to orthokeratology and its cessation: a predictor for the change in axial length. Acta Ophthalmol. 2019;97:e454–e9.
- Chen X, Xiong Y, Liu F, et al. Factors determining the myopia control effect of an orthokeratology lens: a two-year multi-level model. Ophthalmic Physiol Opt. 2022;42(4):786–796. doi: 10.1111/opo.12990.
- Prousali E, Haidich AB, Fontalis A, et al. Efficacy and safety of interventions to control myopia progression in children: an overview of systematic reviews and meta-analyses. BMC Ophthalmol. 2019;19(1):106. doi: 10.1186/s12886-019-1112-3.
- Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53(7):3913–3919. doi: 10.1167/iovs.11-8453.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53(8):5060–5065. doi: 10.1167/iovs.11-8005.
- Jakobsen TM, Møller F. Control of myopia using orthokeratology lenses in scandinavian children aged 6 to 12 years. Eighteen-month data from the Danish randomized study: clinical study of near-sightedness; treatment with orthokeratology lenses (CONTROL study). Acta Ophthalmol. 2022;100(2):175–182. doi: 10.1111/aos.14911.
- Swarbrick HA, Alharbi A, Watt K, et al. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology. 2015;122(3):620–630. doi: 10.1016/j.ophtha.2014.09.028.
- Sankaridurg P, Conrad F, Tran H, et al. Controlling progression of myopia: optical and pharmaceutical strategies. Asia Pac J Ophthalmol (Phila). 2018;7:405–414.
- Cho P, Cheung SW. Discontinuation of orthokeratology on eyeball elongation (DOEE). Cont Lens Anterior Eye. 2017;40(2):82–87. doi: 10.1016/j.clae.2016.12.002.
- Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93(9):1181–1185. doi: 10.1136/bjo.2008.151365.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Short-term changes in ocular biometry and refraction after discontinuation of long-term orthokeratology. Eye Contact Lens. 2014;40(2):84–90. doi: 10.1097/ICL.0000000000000014.
- Cheung SW, Cho P. Long-term effect of orthokeratology on the anterior segment length. Cont Lens Anterior Eye. 2016;39(4):262–265. doi: 10.1016/j.clae.2016.02.003.
- Tong L, Saw SM, Siak JK, et al. Corneal thickness determination and correlates in singaporean schoolchildren. Invest Ophthalmol Vis Sci. 2004;45(11):4004–4009. doi: 10.1167/iovs.04-0121.
- Jones LA, Mitchell GL, Mutti DO, et al. Comparison of ocular component growth curves among refractive error groups in children. Invest Ophthalmol Vis Sci. 2005;46(7):2317–2327. doi: 10.1167/iovs.04-0945.
- Ojaimi E, Rose KA, Morgan IG, et al. Distribution of ocular biometric parameters and refraction in a population-based study of Australian children. Invest Ophthalmol Vis Sci. 2005;46(8):2748–2754. doi: 10.1167/iovs.04-1324.
- Ip JM, Huynh SC, Kifley A, et al. Variation of the contribution from axial length and other oculometric parameters to refraction by age and ethnicity. Invest Ophthalmol Vis Sci. 2007;48(10):4846–4853. doi: 10.1167/iovs.07-0101.
- Shih YF, Chiang TH, Lin LL. Lens thickness changes among schoolchildren in Taiwan. Invest Ophthalmol Vis Sci. 2009;50(6):2637–2644. doi: 10.1167/iovs.08-3090.
- Wong HB, Machin D, Tan SB, et al. Ocular component growth curves among singaporean children with different refractive error status. Invest Ophthalmol Vis Sci. 2010;51(3):1341–1347. doi: 10.1167/iovs.09-3431.
- Lian RR, Sella R, Chen S, et al. Changes in corneal tomography following corneal refractive therapy discontinuation in a patient with history of long-term use. Am J Ophthalmol Case Rep. 2022;26:101450. doi: 10.1016/j.ajoc.2022.101450.
- Wu R, Stapleton F, Swarbrick HA. Residual corneal flattening after discontinuation of long-term orthokeratology lens wear in Asian children. Eye Contact Lens. 2009;35(6):333–337. doi: 10.1097/ICL.0b013e3181bdc41f.
- Nieto-Bona A, Gonzalez-Mesa A, Nieto-Bona MP, et al. Long-term changes in corneal morphology induced by overnight orthokeratology. Curr Eye Res. 2011;36(10):895–904. doi: 10.3109/02713683.2011.593723.
- Kerns RL. Research in orthokeratology. J Am Optom Assoc. 1977;48(3):345–359.
- Polse KA, Brand RJ, Schwalbe JS, et al. The Berkeley orthokeratology study, part II: efficacy and duration. Am J Optom Physiol Opt. 1983;60(3):187–198. doi: 10.1097/00006324-198303000-00006.
- Xu Y, Ye Y, Chong IT, et al. A novel indentation assessment to measure corneal biomechanical properties in glaucoma and ocular hypertension. Transl Vis Sci Technol. 2021;10(9):36. doi: 10.1167/tvst.10.9.36.
- Zhang Z, Chen Z, Chen Z, et al. Change in corneal power distribution in orthokeratology: a predictor for the change in axial length. Transl Vis Sci Technol. 2022;11(2):18. doi: 10.1167/tvst.11.2.18.
- Giloyan A, Harutyunyan T, Petrosyan V. Risk factors for developing myopia among schoolchildren in Yerevan and Gegharkunik province, Armenia. Ophthalmic Epidemiol. 2017;24(2):97–103. doi: 10.1080/09286586.2016.1257028.
- Greene PR. Mechanical considerations in myopia: relative effects of accommodation, convergence, intraocular pressure, and the extraocular muscles. Am J Optom Physiol Opt. 1980;57(12):902–914.
- Ishida Y, Yanai R, Sagara T, et al. Decrease in intraocular pressure following orthokeratology measured with a noncontact tonometer. Jpn J Ophthalmol. 2011;55(3):190–195. doi: 10.1007/s10384-011-0018-2.
- Chang CJ, Yang HH, Chang CA, et al. The influence of orthokeratology on intraocular pressure measurements. Semin Ophthalmol. 2013;28(4):210–215. doi: 10.3109/08820538.2013.768679.