Abstract
Aim: The lumen-apposing metal stent (LAMS) is a new device that expands the scope of gastrointestinal intervention under endoscopy. LAMS was initially used for the treatment of pancreatic fluid collections (PFCs), but is increasingly being used off-label. The electrocautery system simplifies the deployment of LAMS, making it more suitable for off-label situations. The short-term results of electrocautery-enhanced lumen-apposing metal stents (ECE-LAMS) are satisfactory; however, the long-term follow-up results must be evaluated. The aim of this article is to review the expanded clinical application of ECE-LAMS, the clinical value of on-label and off-label use, and follow-up results.
Methods: After searching in PubMed and Web of Science databases using ‘electrocautery-enhanced lumen-apposing metal stents’ and ‘endoscopic ultrasonography (EUS) -guided interventions’ as keywords, studies related were compiled and examined.
Results: ECE-LAMS are widely used for on-label and off-label situations. The short-term and long-term results of ECE-LAMS are satisfactory, but there are still some studies that do not agree with this viewpoint.
Conclusion: The clinical application of ECE-LAMS is relatively safe and reliable but more well-designed randomized trials and prospective studies are needed to evaluate the impact of this technology on therapeutic EUS, to improve the safety and success rate of EUS-guided LAMS implantation, and to expand its application in other indications.
1. Introduction
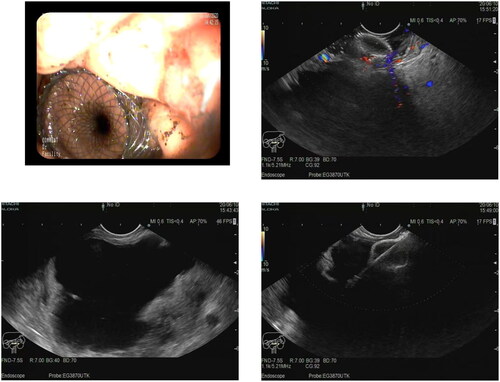
Lumen-apposing metal stents (LAMS) have been rapidly applied in clinical practice since they were approved by the Food and Drug Administration for the treatment of pancreatic fluid collections (PFCs) in 2013. The stents have large inner diameters, allowing PFCs to be fully drained between the two chambers of the stent [Citation1]. The structural characteristics of LAMS such as double flanges and dumbbell structures make them difficult to shift, minimizing the risk of leakage, perforation, and displacement. LAMS is a fully covered, self-expandable metal stent, which has advantages that traditional, commonly-used stents do not have. Although plastic double pigtail stents (DPs) have a structure to prevent stent displacement, their lumens are small, which easily lead to stent blockage. The diameter of the fully covered metal stent is larger, which can effectively prevent the lumen from being blocked, but the tubular structure is prone to displacement, which leads to leakage. Compared with traditional stents, LAMS has a wider range of applications due to its dumbbell-like structure and large internal cavity diameter. Although the United States has not yet approved LAMS for EUS-gallbladder drainage (EUS-GBD), Shayan et al. [Citation2] strictly followed the FDA approved protocol to evaluate the application of LAMS in patients who require EUS-GBD. LAMS has increasingly been applied in off-label indications, such as endoscopic ultrasound (EUS)-gastroenterostomy (EUS-GE), EUS-choledochoduodenostomy (EUS-CD), and endoscopic retrograde cholangiopancreatography/EUS-directed transgastric ERCP (ERCP/EDGE) for patients with anatomical changes and gastrointestinal stenosis () [Citation3]. Currently, many studies describe the use of electocautery-enhanced (ECE-LAMS), and preliminary research data also support that the incidence of early adverse events in the application of ECE-LAMS is satisfactory (early adverse events are defined as adverse events that occur within the first 7 days, including peritoneal collection, hemorrhage, misdeployment, stent obstruction, pneumoperitoneum; late adverse events are defined as adverse events that occur 7 days after stent implantation, including delayed migration, stent infection, stent entrapment, recurrence) [Citation4,Citation5]. This review summarizes the expanded application of ECE-LAMS in the gastrointestinal tract and its long-term results.
Table 1. Summary of the applications of lumen-apposing metal stents (LAMS).
2. Types of LAMS
Currently, two types of LAMS are widely used: Axios stents (Axios-EC, Boston Scientific, Marlborough, USA) and Spaxus stents (Taewoong Medical, Gyeonggi-do, Korea). Both types of stents can be used in combination with electrocautery-enhanced delivery systems. The main advantage of the ECE-LAMS application is that it simplifies the steps of the entire process without using guidewire expansion. Therefore, in recent years, for various gastrointestinal interventions guided by EUS, gastroenterologists have gradually turned to the use of ‘Hot LAMS’ (). There are differences between the two types of stents in terms of deployment methods: Axios stents use the dual locking principle to promote the placement of conduits and stents, while the deployment of Spaxus stents is similar to that of traditional self-expanding metal stents (SEMS), which can recapture stents during stent placement. Although many studies support the use of ‘Hot Axios’ stents, the data on the use of ‘Hot Spaxus’ is also increasing [Citation6].
Table 2. Performance comparison between LAMS and ECE LAMS.
3. Multiple clinical applications of LAMS
3.1. Application of ECE-LAMS in PFCs
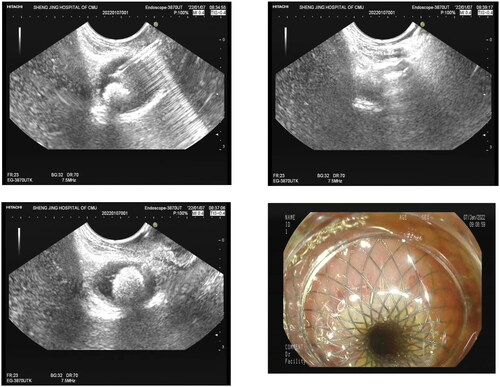
PFCs are complications related to acute and chronic pancreatitis, abdominal trauma, or surgery. EUS can accurately evaluate PFCs and peripheral vessels and directly conduct transmural drainage. The success rate of this method is high and the incidence of adverse events is low. At present, ECE-LAMS are one of the most commonly used topical stents for EUS-guided drainage (). Some retrospective studies showed that the stent had a high technical and clinical success rate for drainage of PFCs with a very low incidence of adverse events [Citation7–9]. The safety and effectiveness of ECE-LAMS in the drainage of various types of PFCs was confirmed in a retrospective and prospective clinical study with a large sample from multiple centers, with a technical success rate of 97.1% and a clinical success rate of 88.8% [Citation10]. At the same time, meta-analysis has confirmed that LAMS is not inferior to DPs in terms of success rate [Citation11–13]. ECE-LAMS can also simplify fluoroscopy during PFCs drainage, which shortens the operation time [Citation14,Citation15]. A 15-mm internal diameter and 10-mm long stent was used in patients with necrotic content, a 10 mm × 10 mm stent in patients with medium size infected lesions, and a 6 mm × 8 mm stent in patients with small abscesses mostly [Citation7,Citation8].
ECE-LAMS in EUS-guided PFCs drainage is satisfactory in the short and medium terms, but delayed adverse events have been reported [Citation16–18]. A multicenter clinical study involved delayed adverse events of PFCs drained by ECE-LAMS including stent displacement (7.4%), stent obstruction and infection (7.9%), massive hemorrhage (2%), ECE-LAMS incarceration (1%), and PFCs recurrence (9.2%) [Citation10]. Bang et al. [Citation19] reported a trial in which the incidence of adverse events was higher in patients with PFCs who were randomly assigned into a LAMS group compared to a DPs group. Among patients in the LAMS group (n = 12), 50% had stent-related adverse events, including delayed bleeding, stent insertion, and stent-induced biliary stenosis, while the DPs group had no related adverse events. Boxhoorn et al. [Citation20] concluded that the incidence of adverse events in the LAMS and DPs groups was similar, with no statistical difference. Another study showed that the failure rate of drainage from walled-off pancreatic necrosis (WON) with ECE-LAMS is very high, because this stent placement does not go through the guidewire expansion step like traditional stent placement, slowing stent expansion and drainage of necrotic fragments. Even the drainage effect of large-diameter non electrocautery enhanced LAMS in WON is not as ideal as imagined [Citation20]. Vanek et al. [Citation21] conducted a double central prospective study finding that adding coaxial DPs to LAMS can ensure smooth stent drainage while significantly reducing the incidence of stent- related adverse events.
Another important factor to consider is the cost of LAMS. A single center randomized controlled trial conducted by Bang et al. [Citation22] showed that for patients with WON, the LAMS group had a higher cost than that of plastic stent group ($12155 vs $6609, p < 0.001). However, the multicenter prospective cohort study conducted by Boxhoorn et al. [Citation23] suggested that even though LAMS devices are more expensive, the higher cost of LAMS may only account for a small portion of the total treatment cost for patients with necrotizing pancreatitis. Ultimately, the medical expenses for the LAMS group and the DPs group are roughly similar. The inconsistency between these two conclusions requires more prospective studies with larger sample sizes in the future.
3.2. Application of ECE-LAMS in EUS-GBD
EUS-GBD is an increasingly recognized method for the treatment of acute cholecystitis and cholecystolithiasis. The use of LAMS thoroughly removes cholecystolithiasis and facilitates subsequent examination and treatment of the gallbladder [Citation24,Citation25]. It probably should be avoided in patients that will subsequently go on to cholecystectomy, as the presence of the LAMS can make that surgery more complex. EUS-GBD combined with LAMS has a high technical success rate (95%–98%) and clinical success rate (95%) [Citation26], and has become a safe and effective alternative to percutaneous gallbladder drainage (PTBD) and endoscopic papillary gallbladder drainage (ERC-GBD).
Cho et al. [Citation27] found no difference in the technical success rate, clinical success rate, surgery-related adverse events, stent-related late adverse events, and cholecystitis recurrence rate of EUS-GBD between anti-migration tubular SEMS (ATSEMS) and LAMS. However, deployment of LAMS with an electrocautery-enhanced delivery system greatly reduces the risk of bile leakage and stent displacement. The lumen adhesion force of LAMS is high, which makes it difficult to displace, but it may also contribute to stent-induced adverse events. The use of an electrocautery-enhanced delivery system reduces the lumen adhesion force of the stent [Citation15]. The feasibility of ECE-LAMS has been confirmed in animal experiments. ECE-LAMS is not only successfully placed and removed in animals, but also forms a mature fistula for gastroscope insertion [Citation28]. Because ECE-LAMS electric cautery devices make it easier to puncture the gallbladder wall, the implementation of ECE-LAMS can further improve the technical success rate. This result has been confirmed in humans [Citation29]; a multicenter retrospective study has proven the safety and effectiveness of ECE-LAMS in EUS-GBD (clinical success rate, 98.7%; technical success rate, 95.9%; and adverse event rate, 10.7%) [Citation17]. In this study, a 10x10mm stent was placed in 65 cases (86.7%), a 15x10mm in 7 patients (9.3%), an 8 × 8 mm in 2 patients (2.7%), and a 6 × 8 mm in the remaining 1 (1.3%).Concern over whether the electric cautery head of ECE-LAMS will cause damage to the intestine is allayed by few reports of related adverse events.
In addition, the incidence of late adverse events in patients with LAMS is low. A review showed that the incidence of late adverse events in LAMS is similar to that in SEMS, but the incidence of stent displacement in the former is lower [Citation30]. However, although the incidence of adverse events of LAMS was very low, the incidence in the late stage was higher than that in the early stage (8.3% vs. 6.5%) [Citation31]. There are relatively few data studies on long-term follow-up of patients treated with ECE-LAMS, and more multicenter, large-sample studies are needed.
Anderloni et al. [Citation32] reported that ECE-LAMS was used in emergency EUS-GBD of patients with acute cholecystitis who were at risk of surgery due to prolonged elevated International Normalized Ratio (INR) and/or anticoagulant use. All stents were successfully placed, and there was no intraoperative or postoperative bleeding. This report showed that EUS-GBD combined with ECE-LAMS is feasible in patients with high surgical risk and prolonged INR and/or anticoagulation, without significantly increasing the risk of bleeding. EUS-GBD combined with ECE-LAMS is safe and effective in patients with malignant causes, which can postpone subsequent surgical treatment or chemotherapy and can be used for hospice care [Citation33].
3.3. Application of ECE-LAMS in EUS-CD
EUS-CD is a technical method that can replace PTBD when ERCP fails. Although increasing evidence shows that EUS-CD is superior to PTBD, only a few endoscopic centers routinely perform the former because this technology is challenging—it involves multiple steps and may cause potential surgical complications such as stent displacement [Citation34]. However, as ECE-LAMS is clinically applied and assisted by EUS-CD (), this integrated device is convenient and safe [Citation35]. Studies have confirmed that ECE-LAMS is safe and effective for the drainage of benign and malignant bile duct obstruction, with a high technical and clinical success rate, especially in cases of ERCP failure [Citation35–39]. However, EUS-CD should also be performed cautiously in patients with ERCP failure. Zulli et al. [Citation40] reported the case of a patient who underwent LAMS for EUS-CD after ERCP failure. Severe stent displacement occurred 5 weeks after surgery.
Iwashita et al. [Citation41] reported a 94% technical success rate and a 19% early adverse event rate after reviewing 300 EUS-CD cases using LAMS. A retrospective multicenter study from six international centers reported that the overall technical success and procedure-related adverse event rates of EUS-CD using LAMS were 84.3% and 32.6%, respectively [Citation42]. In one study, during the 205-day follow-up period, the overall incidence of adverse events in LAMS was 36.8% (7/19); however, these adverse events were mild [Citation43].
To reduce the incidence of adverse events, some research centers placed an axial stent in the ECE-LAMS lumen to ensure non-perpendicularity between the ECE-LAMS axis and the bile duct axis, in this study, a 10 mm-diameter stent was used and concluded that this method reduced the reobstruction rate [Citation37]. However, Garcia et al. [Citation44] evaluated the effectiveness of placing coaxial plastic stents in 41 patients with distal malignant biliary obstruction using LAMS for EUS-CD. Compared with a previous multicenter study, there was no difference in the recurrence rate of biliary obstruction between the LAMS and LAMS + plastic stent groups (13.6% vs. 23.5%). However, a 6 mm-diameter and 8 mm-diameter stent were used in this study. Subsequently, Garcia et al. [Citation45] conducted a multicenter randomized controlled study to compare the two groups, and ultimately concluded that the technical strategy of placing axial DPs in LAMS can reduce the reobstruction rate, but it will increase surgical time and bring related adverse events. Another way to reduce the reobstruction rate is to expand the lumen diameter of the LAMS; however, stents with larger diameters require a longer distance to fully expand, which can easily lead to stent displacement [Citation46].
A systematic review and meta-analysis of 31 studies, including 820 patients, concluded that the performance of LAMS in EUS-CD seems comparable to that of traditional SEMS, and there was no difference between the two groups in terms of technical success (94.8% vs. 92.7%), clinical success (93.6% vs. 91.7%), adverse event incidence (17.1% vs. 18.3%), and reintervention rate (10.9% vs. 13.9%) [Citation47]. In conclusion, EUS-CD using ECE-LAMS is a safe and effective palliative treatment for patients with biliary obstruction. However, there are relatively few studies on late adverse events and LAMS involving an electrocautery-enhanced delivery system [Citation48]. Further research is needed to determine the optimal stent type (ECE-LAMS vs. SEMS), stent size, whether coaxial stents should be placed through ECE-LAMS, and the incidence of adverse events in the long-term.
3.4. Application of ECE-LAMS in EUS-GE
EUS-GE is a new treatment method for gastric outlet obstruction (GOO). If the patient is in general condition and has a good anatomical structure, the clinical success rate is very high. In a retrospective study comparing 30 patients treated with EUS-GE with 52 patients treated with intestinal stents, although there was no difference in the technical and clinical success rates between the two methods, the recurrence and reintervention rates in the EUS-GE group were significantly lower (4.0% vs 28.6%; p = 0.015); In multivariable analysis of control variables, the reintervention rate in the intestinal stent group was 12.8 times higher than that in the EUS-GE group [Citation49]. Wanrooij et al. [Citation50] and Vanella et al. [Citation51] also confirmed that EUS-GE has an advantage over the placement of enteral stenting(ES).In a comparative study, 30 patients treated with EUS-GE for malignant GOO and 60 patients treated with surgical gastrojejunostomy (SGJ) were compared. Although the technical success rate of the SGJ group was significantly higher than that of the EUS-GE group and the incidence of adverse events in the EUS-GE group was not significantly reduced, there was no difference in the clinical success rate, recurrence rate, reintervention time, and average hospital stay between the two groups [Citation52]. However, two recent large retrospective studies show that EUS-GE has more advantages than conventional surgery [Citation53]. Similarly, two systematic reviews reported that the total mortality within 30 days after LAMS placement in patients with malignant gastric outlet obstruction (1.6%) was lower than that in the SGJ and SEMS groups (10–20%) [Citation54,Citation55].
A meta-analysis of 760 patients and 31 studies showed that there was no difference in the technical success rate of LAMS, SEMS, and biodegradable stents in EUS-GE, but the clinical success rate of LAMS was far higher, indicating that LAMS has a better clinical effect in the treatment of gastrointestinal stenosis. The incidence of short-term adverse events was relatively low (16%) during a follow-up of 25 patients who underwent LAMS implantation [Citation56,Citation57].
Most experts have reached a consensus that the ECE-LAMS procedure limits the number of tool exchanges, thus improving the technical success rate and shortening operation time [Citation15]. The preliminary results of EUS-GE using ECE-LAMS are promising: a multicenter prospective international study showed that 26 GOO patients (17 malignant, 9 benign) were treated with EUS-GJ using LAMS. The technical and clinical success rates were 92% and 85%, respectively. Three patients (11.5%) had adverse events such as bleeding, peritonitis, and the need for further surgery. However, because only 35% of the patients in this study were treated with ECE-LAMS, the stent type used was inconsistent [Citation58]. Itoi et al. reported on 20 patients with malignant GOO who underwent EUS-GJ treatment using ECE-LAMS with a technical success rate of 90%, and after 100 days of follow-up, no stent displacement or occlusion was observed [Citation59]. Kenjiro et al. [Citation60] also reported the clinical relief and effective treatment of input loop syndrome after gastrojejunostomy with ECE-LAMS. Although ECE-LAMS demonstrates relatively successful short-term results with EUS-GE treatment of GOO, long-term results require further study.
3.5. Application of LAMS in benign intestinal stenosis
Benign gastrointestinal stenosis can occur in any part of the gastrointestinal tract, usually in the esophagus, pylorus, and anastomotic stoma, and are typically treated by SEMS. However, existing data show that its clinical efficacy is disappointing. In a large-sample retrospective multicenter study, only 33% of patients with benign and refractory stenosis and 23% of patients with anastomotic stenosis were relieved, and 58% and 92% of patients with these two types of stenosis, respectively, required reduction [Citation61]. In a systematic review of 12 studies, the technical success rate of LAMS for benign gastrointestinal stenosis was 98.6% (69/70), and the clinical success rate was 79.7% (55/69). Most stenoses were short (≤ 1 cm); however, similar technical and clinical success rates were observed in cases of isolated long stenoses with two overlapping LAMS, while the failure rate was 21.5% (14/69) in the entire study population [Citation62]. A multicenter prospective study analyzed 21 patients with benign gastrointestinal stenosis treated by LAMS: all patients achieved technical success, 90.5% achieved short-term clinical success, and 66.7% achieved long-term clinical success. This study once again confirmed that LAMS is technically feasible and safe in the treatment of benign stenosis [Citation63]. However, some studies have shown that the reintervention rate after LAMS removal is very high, and many stenoses cannot be resolved by prolonging the stent placement time [Citation64]. A recent large sample retrospective study also confirmed this view [Citation65]. In a subgroup analysis of patients treated with LAMS with different diameters, stent displacement and pain were the most common adverse events of the 15 mm and the 20 mm LAMS, respectively. Compared with smaller-diameter LAMS, larger-diameter LAMS may have lower stent mobility [Citation46].
Nader et al. [Citation66] reported a case of perforation in a patient who had been placed with a 15 × 10 mm LAMS for 3 weeks after the treatment of ileum and sigmoidal anastomosis stenosis. Although the short-term therapeutic effect of LAMS is relatively satisfactory, its long-term therapeutic effect still needs to be determined. At present, most LAMS are deployed using non-electrocautery delivery systems. There are few studies on ECE-LAMS for benign gastrointestinal stenosis, which requires more attention in the future.
3.6. Application of LAMS in EDGE of RYGB patients
Roux-en-Y gastric bypass (RYGB) is a common weight-loss surgery; however, the anatomical route of the RYGB makes it difficult for the examination instrument to enter the biliary tract. It is estimated that 36% of patients receiving RYGB treatment develop gallstones, of which 5.3% require ERCP treatment [Citation67]. EDGE was first described in 2014 as a method of ERCP for patients with RYGB-dissection. This technique involves placing a LAMS between the excluded stomach and the jejunum or the remaining stomach under EUS guidance and then conducting routine ERCP through LAMS [Citation68]. Current research shows that EDGE is a safe and effective method for the treatment of pancreaticobiliary diseases in patients who do not require emergency endoscopic treatment. One study showed that the technical success rate of EDGE in RYGB patients was 100% [Citation69], and other studies have reached the same conclusion [Citation70,Citation71]. However, many clinicians are concerned about persistent fistula formation after stent removal. Theodore et al. [Citation70] found that in some cases, when argon plasma coagulation (APC) was not applied to the fistula after stent removal, the upper gastrointestinal fistula persisted, and the persistent fistula was related to weight gain. For fistulas that cannot close spontaneously, APC may indeed be helpful.
Chronic stenosis after RYGB is a difficult complication, with a high incidence rate. In a study of 421 patients who underwent RYGB, 14 patients (3.3%) had stenosis and underwent EUS-guided LAMS implantation. No intraoperative adverse events were observed in any of the patients and 12 showed complete remission of stenosis. Although the mobility rate was 19%, reoperation was not required for migration-related problems [Citation71]. Gianfranco [Citation72] and others reported a case of gastrojejunal anastomosis rupture in EUS guided gastric intervention therapy (EDGI). It can be seen that attention should also be paid to its possible adverse events.
3.7. Application of ECE-LAMS in special causes
2.7.1 ECE-LAMS can effectively drain intraperitoneal collections. Some retrospective studies and case reports have proven the feasibility and safety of EUS guiding pelvic abscess drainage [Citation73–75]. Laurent et al. [Citation76] reported a case of a large pelvic abscess with an anorectal fistula that was successfully drained with ECE-LAMS without recurrence. More prospective studies are needed to confirm this application and to determine the location of pelvic effusion drainage under EUS guidance.
2.7.2 Drainage treatment of liver abscess after hepatectomy using ECE-LAMS is also successful and efficient [Citation77]. Fabia et al. [Citation78] reported a case of an abscess between the right hepatic lobe and stomach after left hepatectomy. They placed a ‘Hot Axios’ stent under EUS guidance to drain pus without complications. After 4 weeks, the stent was removed and the abscess completely subsided. This case shows that ECE-LAMS is safe, easy to use, efficient and should be considered when detecting EUS-palpable intra-abdominal abscesses. There should be more and larger-sample studies in the future to confirm this view.
4. ECE-LAMS insertion process learning curve
EDGE has the same technical success and adverse event rates as laparoscopic surgery, with the advantage of greatly reducing the operation time and hospital stay [Citation79]. However, the implementation of EDGE requires proficiency in EUS application and ECE-LAMS deployment. In a study of 19 patients who underwent EDGE, including three patients who were implanted with ECE-LAMS, performed by a single operator, the median operative time was 54.5 min. The operator reached the average operative time by the ninth operation. After that, except for two abnormal values, the duration of the procedure was further shortened, indicating that the operator was able to master the procedures after 25–35 operations [Citation80]. Amy et al. summarized the learning curve of the gastrointestinal anastomosis process of ECE-LAMS implantation, indicating that the operator had reached the average level in the seventh operation and continued to improve thereafter. More large-scale research is needed to understand the learning curve of different operations and to verify existing curves [Citation81].
5. Conclusion
Although the development of LAMS is a major progress in therapeutic EUS, further technical improvements are needed, especially for further study of the electrocautery enhanced delivery system for stent deployment. At present, there are relatively few relevant studies, and more well-designed randomized trials and prospective studies are needed to evaluate the impact of this technology on therapeutic EUS, to improve the safety and success rate of EUS-guided LAMS implantation, and to expand its application in other indications.
Authors’ contributions
Yumo She and Nan Ge were responsible for the conception; Yumo She was responsible for the acquisition of the literature for the manuscript. Yumo She wrote the original draft of the manuscript. Yumo She and Nan Ge reviewed and edited. Nan Ge supervised the paper. Nan Ge revised the paper critically for intellectual content. All authors have read and agreed to the published version of the manuscript.
Acknowledgments
The authors thank all the participants in this study. We are also grateful to the hospital staff who provided perspective and advice during the preparation of this manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Additional information
Funding
References
- Law RJ, Chandrasekhara V, Bhatt A, et al. Lumen-apposing metal stents (with videos). Gastrointest Endosc. 2021;94(3):1–11. doi:10.1016/j.gie.2021.05.020.
- Irani SS, Sharma NR, Storm AC, et al. Endoscopic ultrasound-guided transluminal gallbladder drainage in patients with acute cholecystitis: a prospective multicenter trial. Ann Surg. 2023;278(3):e556–e562. doi:10.1097/SLA.0000000000005784.
- Ramai D, Facciorusso A, DeLuca M, et al. Adverse events associated with AXIOS stents: insights from the manufacturer and user facility device experience database. Endosc Ultrasound. 2022;11(3):231–236. doi:10.4103/EUS-D-21-00096.
- da Silva RRR, Facanali Junior MR, Brunaldi VO, et al. EUS-guided choledochoduodenostomy for malignant biliary obstruction: a multicenter comparative study between plastic and metallic stents. Endosc Ultrasound. 2023;12(1):120–127. doi:10.4103/EUS-D-21-00221.
- Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71(3):446–454. doi:10.1016/j.gie.2009.10.027.
- Mangiavillano B, Moon JH, Crinò SF, et al. Safety and efficacy of a novel electrocautery-enhanced lumen-apposing metal stent in interventional EUS procedures (with video). Gastrointest Endosc. 2022;95(1):115–122. doi:10.1016/j.gie.2021.07.021.
- Rinninella E, Kunda R, Dollhopf M, et al. EUS-guided drainage of pancreatic fluid collections using a novel lumen-apposing metal stent on an electrocautery-enhanced delivery system: a large retrospective study (with video). Gastrointest Endosc. 2015;82(6):1039–1046. doi:10.1016/j.gie.2015.04.006.
- Anderloni A, Orellana F, Jovani M, et al. Endoscopic ultrasound-guided drainage of a pancreatic pseudocyst with a novel lumen-apposing metal stent on an electrocautery-enhanced delivery system. Dig Liver Dis. 2015;47(10):e17. doi:10.1016/j.dld.2015.05.010.
- Shamah SP, Sahakian AB, Chapman CG, et al. Double pigtail stent placement as an adjunct to lumen-apposing metal stentsfor drainage of pancreatic fluid collections may not affect outcomes: a multicenter experience. Endosc Ultrasound. 2022;11(1):53–58. doi:10.4103/EUS-D-21-00030.
- Khan S, Chandran S, Chin J, et al. Drainage of pancreatic fluid collections using a lumen-apposing metal stent with an electrocautery-enhanced delivery system. J Gastroenterol Hepatol. 2021;36(12):3395–3401. doi:10.1111/jgh.15658.
- Guzmán-Calderón E, Chacaltana A, Díaz R, et al. Head-to-head comparison between endoscopic ultrasound guided lumen apposing metal stent and plastic stents for the treatment of pancreatic fluid collections: a systematic review and meta-analysis. J Hepatobiliary Pancreat Sci. 2022;29(2):198–211. doi:10.1002/jhbp.1008.
- Vanella G, Bronswijk M, Arcidiacono PG, et al. Current landscape of therapeutic EUS: changing paradigms in gastroenterology practice. Endosc Ultrasound. 2023;12(1):16–28. doi:10.4103/EUS-D-21-00177.
- Chandrasekhara V, Barthet M, Devière J, et al. Safety and efficacy of lumen-apposing metal stents versus plastic stents to treat walled-off pancreatic necrosis: systematic review and meta-analysis. Endosc Int Open. 2020;8(11):E1639–e1653. doi:10.1055/a-1243-0092.
- Olaiya B, Mekaroonkamol P, Li BW, et al. Outcomes of a single-step endoscopic ultrasound-guided drainage of pancreatic-fluid collections using an electrocautery-enhanced coaxial lumen-apposing, self-expanding metal stent with and without fluoroscopy. Gastroenterol Rep (Oxf). 2020;8(6):425–430. doi:10.1093/gastro/goaa020.
- Zhang K, Ge N, Guo J, et al. Ex vivo comparison of electrocautery-enhanced delivery of lumen-apposing metal stents matching electrosurgical workstations during EUS-guided gallbladder drainage. Endosc Ultrasound. 2022;11(5):377–382. doi:10.4103/EUS-D-21-00240.
- Tarantino I, Peralta M, Ligresti D, et al. Endoscopic ultrasound-guided biliary drainage of malignant stenosis, not treatable with endoscopic retrograde cholangiopancreatography: a single-center, prospective observational study. Endosc Int Open. 2021;9(2):E110–e115. doi:10.1055/a-1313-6850.
- Dollhopf M, Larghi A, Will U, et al. EUS-guided gallbladder drainage in patients with acute cholecystitis and high surgical risk using an electrocautery-enhanced lumen-apposing metal stent device. Gastrointest Endosc. 2017;86(4):636–643. doi:10.1016/j.gie.2017.02.027.
- Manta R, Torrisi S, Castellani D, et al. Endoscopic ultrasonography-guided biliary drainage for malignant jaundice by using electrocautery-enhanced lumen-apposing metal stents (Hot-SPAXUS stent). Ann Gastroenterol. 2022;35(6):663–667. doi:10.20524/aog.2022.0743.
- Bang JY, Hasan M, Navaneethan U, et al. Lumen-apposing metal stents (LAMS) for pancreatic fluid collection (PFC) drainage: may not be business as usual. Gut. 2017;66(12):2054–2056. doi:10.1136/gutjnl-2016-312812.
- Karstensen JG, Novovic S, Hansen EF, et al. EUS-guided drainage of large walled-off pancreatic necroses using plastic versus lumen-apposing metal stents: a single-Centre randomised controlled trial. Gut. 2023;72(6):1167–1173. doi:10.1136/gutjnl-2022-328225.
- Vanek P, Falt P, Vitek P, et al. EUS-guided transluminal drainage using lumen-apposing metal stents with or without coaxial plastic stents for treatment of walled-off necrotizing pancreatitis: a prospective bicentric randomized controlled trial. Gastrointest Endosc. 2023;97(6):1070–1080. doi:10.1016/j.gie.2022.12.026.
- Bang JY, Navaneethan U, Hasan MK, et al. Non-superiority of lumen-apposing metal stents over plastic stents for drainage of walled-off necrosis in a randomised trial. Gut. 2019;68(7):1200–1209. doi:10.1136/gutjnl-2017-315335.
- Boxhoorn L, Verdonk RC, Besselink MG, et al. Comparison of lumen-apposing metal stents versus double-pigtail plastic stents for infected necrotising pancreatitis. Gut. 2023;72(1):66–72. doi:10.1136/gutjnl-2021-325632.
- Vanella G, Dell’Anna G, Bronswijk M, et al. EUS-guided gallbladder drainage and subsequent peroral endoscopic cholecystolithotomy: a tool to reduce chemotherapy discontinuation in neoplastic patients? VideoGIE. 2022;7(3):120–127. doi:10.1016/j.vgie.2021.10.002.
- Higa JT, Sahar N, Kozarek RA, et al. EUS-guided gallbladder drainage with a lumen-apposing metal stent versus endoscopic transpapillary gallbladder drainage for the treatment of acute cholecystitis (with videos). Gastrointest Endosc. 2019;90(3):483–492. doi:10.1016/j.gie.2019.04.238.
- Saumoy M, Yang J, Bhatt A, et al. Endoscopic therapies for gallbladder drainage. Gastrointest Endosc. 2021;94(4):671–684. doi:10.1016/j.gie.2021.05.031.
- Cho SH, Oh D, Song TJ, et al. Comparison of the effectiveness and safety of lumen-apposing metal stents and anti-migrating tubular self-expandable metal stents for EUS-guided gallbladder drainage in high surgical risk patients with acute cholecystitis. Gastrointest Endosc. 2020;91(3):543–550. doi:10.1016/j.gie.2019.09.042.
- Mukai S, Itoi T, Tsuchiya T, et al. Experimental study of a physician-controlled electrocautery-enhanced delivery system incorporating a newly developed lumen-apposing metal stent for interventional endoscopic ultrasound (with videos). J Hepatobiliary Pancreat Sci. 2022;29(7):817–824. doi:10.1002/jhbp.1113.
- Jo SJ, Moon JH, Lee YN, et al. A novel bipolar electrocautery-enhanced delivery system with a lumen-apposing metal stent for EUS-guided drainage: a porcine study. J Hepatobiliary Pancreat Sci. 2022;30(2):263–268.
- Manta R, Mutignani M, Galloro G, et al. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis with a lumen-apposing metal stent: a systematic review of case series. Eur J Gastroenterol Hepatol. 2018;30(7):695–698. doi:10.1097/MEG.0000000000001112.
- Fabbri C, Coluccio C, Binda C, et al. Lumen-apposing metal stents: how far are we from standardization? An italian survey. Endosc Ultrasound. 2022;11(1):59–67. doi:10.4103/EUS-D-21-00015.
- Anderloni A, Attili F, Sferrazza A, et al. EUS-guided gallbladder drainage using a lumen-apposing self-expandable metal stent in patients with coagulopathy or anticoagulation therapy: a case series. Endosc Int Open. 2017;5(11):E1100–e1103. doi:10.1055/s-0043-118828.
- Chang JI, Dong E, Kwok KK. Endoscopic ultrasound-guided transmural gallbladder drainage in malignant obstruction using a novel lumen-apposing stent: a case series (with video). Endosc Int Open. 2019;7(5):E655–e661. doi:10.1055/a-0826-4309.
- Itonaga M, Hatamaru K, Kitano M. EUS-guided choledochoduodenostomy using an antimigration metal stent with a thin delivery system for tract dilatation (with video). Endosc Ultrasound. 2021;11(5):414–415.
- Jacques J, Privat J, Pinard F, et al. Endoscopic ultrasound-guided choledochoduodenostomy with electrocautery-enhanced lumen-apposing stents: a retrospective analysis. Endoscopy. 2019;51(6):540–547. doi:10.1055/a-0735-9137.
- Ginestet C, Sanglier F, Hummel V, et al. EUS-guided biliary drainage with electrocautery-enhanced lumen-apposing metal stent placement should replace PTBD after ERCP failure in patients with distal tumoral biliary obstruction: a large real-life study. Surg Endosc. 2022;36(5):3365–3373. doi:10.1007/s00464-021-08653-1.
- El Chafic AH, Shah JN, Hamerski C, et al. EUS-Guided choledochoduodenostomy for distal malignant biliary obstruction using Electrocautery-Enhanced Lumen-Apposing metal stents: first US, multicenter experience. Dig Dis Sci. 2019;64(11):3321–3327. doi:10.1007/s10620-019-05688-2.
- Fuentes-Valenzuela E, de la Serna Higuera C, Pérez-Miranda M. Endoscopic ultrasound-guided choledocoduodenostomy with electrocautery-enhanced lumen-apposing metal stent for benign biliary obstruction: when all other options fail. Dig Endosc. 2021;33(4):670–670. doi:10.1111/den.13958.
- Sawas T, Bailey NJ, Yeung K, et al. Comparison of EUS-guided choledochoduodenostomy and percutaneous drainage for distal biliary obstruction: a multicenter cohort study. Endosc Ultrasound. 2022;11(3):223–230. doi:10.4103/EUS-D-21-00031.
- Zulli C, Dumont JL, Cereatti F, et al. Rescue ERCP after delayed migration of a lumen-apposing metal stent following endoscopic ultrasound-guided choledochoduodenostomy. Endoscopy. 2020;52(6):E215–e216. doi:10.1055/a-1073-7317.
- Iwashita T, Doi S, Yasuda I. Endoscopic ultrasound-guided biliary drainage: a review. Clin J Gastroenterol. 2014;7(2):94–102. doi:10.1007/s12328-014-0467-5.
- Gupta K, Perez-Miranda M, Kahaleh M, InEBD STUDY GROUP., et al. Endoscopic ultrasound-assisted bile duct access and drainage: multicenter, long-term analysis of approach, outcomes, and complications of a technique in evolution. J Clin Gastroenterol. 2014;48(1):80–87. doi:10.1097/MCG.0b013e31828c6822.
- Tsuchiya T, Teoh AYB, Itoi T, et al. Long-term outcomes of EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction: a prospective multicenter study. Gastrointest Endosc. 2018;87(4):1138–1146. doi:10.1016/j.gie.2017.08.017.
- Garcia-Sumalla A, Loras C, Guarner-Argente C, et al. Is a coaxial plastic stent within a lumen-apposing metal stent useful for the management of distal malignant biliary obstruction? Surg Endosc. 2021;35(8):4873–4881. doi:10.1007/s00464-021-08435-9.
- Garcia-Sumalla A, Loras C, Sanchiz V, et al. Multicenter study of lumen-apposing metal stents with or without pigtail in endoscopic ultrasound-guided biliary drainage for malignant obstruction-BAMPI TRIAL: an open-label, randomized controlled trial protocol. Trials. 2022;23(1):181. doi:10.1186/s13063-022-06106-1.
- Mizrahi M, Fahmawi Y, Merritt L, et al. Luminal-apposing stents for benign intraluminal strictures: a large United States multicenter study of clinical outcomes. Ann Gastroenterol. 2021;34(1):33–38.
- Amato A, Sinagra E, Celsa C, et al. Efficacy of lumen-apposing metal stents or self-expandable metal stents for endoscopic ultrasound-guided choledochoduodenostomy: a systematic review and meta-analysis. Endoscopy. 2021;53(10):1037–1047. doi:10.1055/a-1324-7919.
- Nishiguchi K, Ogura T, Okuda A, et al. Endoscopic gallbladder drainage for acute cholecystitis with high-risk surgical patients between transduodenal and transpapillary stenting. Endosc Ultrasound. 2021;10(6):448–454. doi:10.4103/EUS-D-20-00130.
- Chen YI, Itoi T, Baron TH, et al. EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc. 2017;31(7):2946–2952. doi:10.1007/s00464-016-5311-1.
- van Wanrooij RLJ, Vanella G, Bronswijk M, et al. Endoscopic ultrasound-guided gastroenterostomy versus duodenal stenting for malignant gastric outlet obstruction: an international, multicenter, propensity score-matched comparison. Endoscopy. 2022;54(11):1023–1031. doi:10.1055/a-1782-7568.
- Vanella G, Dell’Anna G, Capurso G, et al. EUS-guided gastroenterostomy for management of malignant gastric outlet obstruction: a prospective cohort study with matched comparison with enteral stenting. Gastrointest Endosc. 2023;98(3):337–347.e335. doi:10.1016/j.gie.2023.04.2072.
- Khashab MA, Bukhari M, Baron TH, et al. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy versus surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open. 2017;5(4):E275–e281. doi:10.1055/s-0043-101695.
- Bronswijk M, Vanella G, van Malenstein H, et al. Laparoscopic versus EUS-guided gastroenterostomy for gastric outlet obstruction: an international multicenter propensity score-matched comparison (with video). Gastrointest Endosc. 2021;94(3):526–536.e522. doi:10.1016/j.gie.2021.04.006.
- Antonelli G, Kovacevic B, Karstensen JG, et al. Endoscopic ultrasound-guided gastro-enteric anastomosis: a systematic review and meta-analysis. Dig Liver Dis. 2020;52(11):1294–1301. doi:10.1016/j.dld.2020.04.021.
- Fabbri C, Binda C, Fugazzola P, et al. Hybrid gastroenterostomy using a lumen-apposing metal stent: a case report focusing on misdeployment and systematic review of the current literature. World J Emerg Surg. 2022;17(1):6. doi:10.1186/s13017-022-00409-z.
- Irani S, Jalaj S, Ross A, et al. Baron TH use of a lumen-apposing metal stent to treat GI strictures (with videos). Gastrointest Endosc. 2017;85(6):1285–1289. doi:10.1016/j.gie.2016.08.028.
- Tan S, Zhong C, Huang S, et al. Clinical outcomes of lumen-apposing metal stent in the management of benign gastrointestinal strictures: a systematic review and meta-analysis. Scand J Gastroenterol. 2019;54(7):811–821. doi:10.1080/00365521.2019.1638447.
- Tyberg A, Perez-Miranda M, Sanchez-Ocaña R, et al. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: a multicenter, international experience. Endosc Int Open. 2016;4(3):E276–281. doi:10.1055/s-0042-101789.
- Itoi T, Ishii K, Ikeuchi N, et al. Prospective evaluation of endoscopic ultrasonography-guided double-balloon-occluded gastrojejunostomy bypass (EPASS) for malignant gastric outlet obstruction. Gut. 2016;65(2):193–195. doi:10.1136/gutjnl-2015-310348.
- Yamamoto K, Tsuchiya T, Tanaka R, et al. Afferent loop syndrome treated by endoscopic ultrasound-guided gastrojejunostomy, using a lumen-apposing metal stent with an electrocautery-enhanced delivery system. Endoscopy. 2017;49(11):E270–e272. doi:10.1055/s-0043-115893.
- Suzuki T, Siddiqui A, Taylor LJ, et al. Clinical outcomes, efficacy, and adverse events in patients undergoing esophageal stent placement for benign indications: a large multicenter study. J Clin Gastroenterol. 2016;50(5):373–378. doi:10.1097/MCG.0000000000000500.
- Jain D, Patel U, Ali S, et al. Efficacy and safety of lumen-apposing metal stent for benign gastrointestinal stricture. Ann Gastroenterol. 2018;31(4):425–438. doi:10.20524/aog.2018.0272.
- Santos-Fernandez J, Paiji C, Shakhatreh M, et al. Lumen-apposing metal stents for benign gastrointestinal tract strictures: an international multicenter experience. World J Gastrointest Endosc. 2017;9(12):571–578. doi:10.4253/wjge.v9.i12.571.
- Bazerbachi F, Heffley JD, Abu Dayyeh BK, et al. Safety and efficacy of coaxial lumen-apposing metal stents in the management of refractory gastrointestinal luminal strictures: a multicenter study. Endosc Int Open. 2017;5(9):E861–e867. doi:10.1055/s-0043-114665.
- Mahmoud T, Beran A, Bazerbachi F, et al. Lumen-apposing metal stents for the treatment of benign gastrointestinal tract strictures: a single-center experience and proposed treatment algorithm. Surg Endosc. 2023;37(3):2133–2142. doi:10.1007/s00464-022-09715-8.
- Mekheal N, Aslanian H, Kesar V, et al. Ileosigmoid anastomotic perforation three weeks after placement of Lumen-Apposing metal stent (LAMS). Cureus. 2021;13(12):e20565. doi:10.7759/cureus.20565.
- Nagem RG, Lázaro-da-Silva A, de Oliveira RM, et al. Gallstone-related complications after roux-en-Y gastric bypass: a prospective study. Hepatobiliary Pancreat Dis Int. 2012;11(6):630–635. doi:10.1016/s1499-3872(12)60236-7.
- Barakat MT, Adler DG. EUS-directed transgastric ERCP: a first-line option for ERCP following roux-en-Y gastric bypass. Endosc Ultrasound. 2021;10(3):151–153. doi:10.4103/eus.eus_148_20.
- Tyberg A, Nieto J, Salgado S, et al. Endoscopic ultrasound (EUS)-directed transgastric endoscopic retrograde cholangiopancreatography or EUS: mid-Term analysis of an emerging procedure. Clin Endosc. 2017;50(2):185–190. doi:10.5946/ce.2016.030.
- James TW, Baron TH. Endoscopic Ultrasound-Directed transgastric ERCP (EDGE): a Single-Center US experience with follow-up data on fistula closure. Obes Surg. 2019;29(2):451–456. doi:10.1007/s11695-018-3531-2.
- Skidmore AP. Use of lumen-apposing metal stents (LAMS) in the management of gastro jejunostomy stricture following roux-en-Y gastric bypass for obesity: a prospective series. BMC Surg. 2021;21(1):314. doi:10.1186/s12893-021-01310-3.
- Donatelli G, Cereatti F, Daho F. EUS-guided anastomosis complication in a patient with roux-en-Y gastric bypass: dehiscence of the surgical anastomosis during endoscopic mucosal resection across EUS-guided jejunum-gastric anastomosis with lumen apposing metal stent. Obes Surg. 2021;31(7):3384–3385. doi:10.1007/s11695-021-05395-w.
- Lisotti A, Cominardi A, Bacchilega I, et al. EUS-guided transrectal drainage of pelvic fluid collections using electrocautery-enhanced lumen-apposing metal stents: a case series. VideoGIE. 2020;5(8):380–385. doi:10.1016/j.vgie.2020.04.014.
- Poincloux L, Caillol F, Allimant C, et al. Long-term outcome of endoscopic ultrasound-guided pelvic abscess drainage: a two-center series. Endoscopy. 2017;49(5):484–490. doi:10.1055/s-0042-122011.
- Gjeorgjievski M, Abdelqader A, Sarkar A, et al. EUS-guided drainage of liver abscesses: video demonstration of two novel endoscopic techniques (with video). Endosc Ultrasound. 2022;11(5):418–420. doi:10.4103/EUS-D-21-00162.
- Monino L, Piessevaux H, Denis MA, et al. Management of pelvic abscess complicating a rectoanal fistula using endoscopic ultrasound-guided drainage with an electrocautery-enhanced lumen-apposing metal stent. Endoscopy. 2021;53(11):E409–e410. doi:10.1055/a-1333-0653.
- Matsumata T, Yanaga K, Shimada M, et al. Occurrence of intraperitoneal septic complications after hepatic resections between 1985 and 1990. Surg Today. 1995;25(1):49–54. doi:10.1007/BF00309385.
- Attili F, Dang S, Rimbaș M, et al. Endoscopic ultrasound-guided drainage of a post-hepatectomy abscess using a lumen-apposing self-expandable metal stent with electrocautery-enhanced delivery system. Endoscopy. 2016;48 Suppl 1(Suppl 1):E222–223. doi:10.1055/s-0042-109051.
- Bahdi F, George R, Paneerselvam K, et al. Comparison of endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography outcomes using various technical approaches. Endosc Int Open. 2022;10(4):E459–e467. doi:10.1055/a-1783-9564.
- Tyberg A, Kedia P, Tawadros A, et al. EUS-Directed transgastric endoscopic retrograde cholangiopancreatography (EDGE): the first learning curve. J Clin Gastroenterol. 2020;54(6):569–572. doi:10.1097/MCG.0000000000001326.
- Tyberg A, Kats D, Choi A, et al. Endoscopic ultrasound guided gastroenterostomy: what is the learning curve? J Clin Gastroenterol. 2021;55(8):691–693. doi:10.1097/MCG.0000000000001400.