Abstract
Background
Stroke rehabilitation presents a complex challenge, necessitating innovative approaches to optimise functional recovery. Virtual Reality-Based Rehabilitation (VRBR) has emerged as a promising intervention that capitalises on immersive technology to engage stroke survivors in their recovery journey. This review aims to examine the efficacy of VRBR in stroke rehabilitation, focusing on its advantages and challenges.
Methods
A comprehensive search of relevant literature was conducted to gather evidence on the efficacy of VRBR in stroke survivors. Studies that investigated the impact of VRBR on patient engagement, functional recovery, and overall rehabilitation outcomes were included. The review also assessed the ability of VRBR to simulate real-life scenarios and facilitate essential daily activities for stroke survivors.
Results
The review highlights that VRBR offers a unique immersive experience that enhances patient engagement and motivation during rehabilitation. The immersive nature of VRBR fosters a sense of presence, which can positively impact treatment adherence and outcomes. Moreover, VRBR’s capacity to replicate real-world scenarios provides stroke survivors with opportunities to practice vital daily activities, promoting functional independence. In contrast, conventional rehabilitation methods lack the same level of engagement and real-world simulation.
Conclusion
VRBR holds promise as an efficacious intervention in stroke rehabilitation. Its immersive nature enhances patient engagement and motivation, potentially leading to better treatment adherence and outcomes. The ability of VRBR to simulate real-life scenarios offers a unique platform. However, challenges such as cost, equipment, patient suitability, data privacy, and acceptance must be addressed for successful integration into stroke rehabilitation practice.
Introduction
Stroke is a major global health concern, the second leading cause of death and the third most common cause of disability [Citation1]. The World Health Organization defines stroke as a sudden focal or global disturbance of cerebral function, lasting over 24 h or leading to death, with no apparent cause other than vascular origin [Citation2]. However, a new definition proposed by the American Stroke Association incorporates clinical and tissue criteria, broadening the scope of the stroke to include objective evidence of permanent brain, spinal cord, or retinal cell death with a vascular aetiology, with or without clinical symptoms [Citation3].
Ischemic stroke, caused by the interrupted blood supply to the brain, and hemorrhagic stroke, resulting from blood vessel rupture, are the two major types of strokes [Citation4]. Several risk factors contribute to stroke, including modifiable factors such as hypertension, diabetes mellitus, high blood cholesterol, cardiovascular diseases, sedentary lifestyle, atrial fibrillation, smoking, and alcohol consumption, as well as nonmodifiable factors like age and gender [Citation5–7]. INTERSTROKE’s study identified ten major stroke risk factors responsible for 90% of all strokes [Citation8]. Stroke management necessitates a multidisciplinary approach beyond hospital admission [Citation9,Citation10]. Proper blood pressure management is crucial for stroke prevention and acute treatment [Citation11]. Functional recovery in stroke survivors can occur through the resolution of impairments (reacquisition of premorbid movement patterns) and compensation (using alternative movements or effectors to achieve the same goal) [Citation12].
Motor dysfunction is a common and severe complication of stroke, significantly impacting the quality of life for patients [Citation13]. Upper limb motor function, particularly hand motor function, is challenging to predict in stroke survivors [Citation14,Citation15]. While the proportional recovery rule suggests that patients will regain approximately 70% of lost function, predicting outcomes for the most severe cases remains challenging [Citation16]. Motor-control regions in stroke patients show greater activation in the unaffected hemisphere and midline surface than healthy controls during simple motor tasks [Citation17]. This decline in motor control results in an impaired ability to produce precise and steady motor output with the affected limb [Citation18].
Stroke rehabilitation is a complex and evolving process that addresses the multifaceted impairments resulting from stroke, spanning the physical and cognitive domains [Citation19]. Besides physical and cognitive domains, the psychological domain is also essential to stroke rehabilitation [Citation19]. Early initiation of rehabilitation has been associated with significant benefits, facilitating functional recovery and improving long-term outcomes for stroke survivors [Citation20]. However, the brain’s remarkable ability to reorganise and adapt, known as neuroplasticity, also plays a pivotal role in driving recovery by establishing new neural connections and pathways [Citation21]. Despite significant advancements in stroke rehabilitation, there is still a need for a deeper understanding of stroke recovery mechanisms, particularly in the context of upper limb motor function [Citation22]. Identifying effective rehabilitation strategies tailored to individual patient needs is crucial in enhancing functional recovery and improving stroke survivors’ overall quality of life. Future research in this area will contribute to optimising stroke rehabilitation protocols and improving patient outcomes [Citation22].
Conventional rehabilitation techniques have effectively improved upper limb function in stroke survivors [Citation23]. However, these methods are resource-intensive and costly, often requiring access to specialised facilities that may be limited [Citation24]. Moreover, conventional upper limb rehabilitation typically demands 2–3 h of daily training for over six weeks, leading to monotony and draining the confidence and interest of patients while also placing significant strain on therapists [Citation25]. Physiotherapy, a common approach in stroke rehabilitation, is usually provided primarily in the early months after a stroke, but its effectiveness and appropriateness during the chronic phase are uncertain [Citation26]. Although physiotherapy has shown effectiveness in treating motor impairment and enhancing functional recovery following stroke, the intensity, frequency, and specificity of physiotherapy play pivotal roles in determining the extent of recovery [Citation23]. Rehabilitation is commonly delivered through a team-based approach involving various disciplines, such as physical therapy, occupational therapy, and speech and language therapy, tailored to address the specific nature and severity of the deficits [Citation27]. The rehabilitation setting can vary, including home-based outpatient therapy, home health therapy, inpatient rehabilitation facilities, or skilled nursing facilities [Citation28]. Despite the benefits of existing rehabilitation approaches, certain limitations hinder the optimal delivery of rehabilitation services to stroke survivors [Citation29]. The timing and duration of rehabilitation services are often determined by post-stroke duration or predetermined maximum utilisation rather than based on individual functional needs and recovery, as recommended by current evidence-based stroke rehabilitation guidelines [Citation29]. Furthermore, rehabilitation services are commonly discontinued after one year post-stroke in many rehabilitation centres, often without a proper transfer of care plan. This abrupt discontinuation of services may impede the ongoing recovery process for stroke survivors [Citation28]. In addition to timing and continuity issues, the lack of designated stroke rehabilitation wards and a shortage of trained rehabilitation professionals pose significant challenges in providing optimal rehabilitation services during the acute and recovery stages of stroke [Citation25]. These limitations in resources and infrastructure may compromise the effectiveness of stroke rehabilitation and hinder achieving maximum recovery potential for stroke survivors [Citation24].
Vvirtual Reality (VR) has become one of the most widely utilised advanced neurorehabilitation technologies for enhancing motor and cognitive abilities in stroke patients [Citation30]. VR employs computer-based technology to create interactive simulations that immerse users in multisensory, simulated environments, providing real-time feedback on their performance [Citation30]. It allows stroke patients to engage in activities that resemble real-world objects and events, offering a unique and immersive rehabilitation experience [Citation31]. The potential benefits of VR in neurorehabilitation have been recognised, particularly in stroke rehabilitation. VR methods hold promise for accelerating rehabilitation and enhancing the motivation of select groups of stroke patients [Citation32]. VR technologies initially garnered attention by providing engaging and motivating rehabilitation interventions as a potentially successful medium for enhancing stroke rehabilitation outcomes [Citation33]. By adapting to the user’s responses and incorporating feedback, VR facilitates a more dynamic and personalised rehabilitation experience [Citation34]. However, it is crucial to acknowledge that VR applications in stroke rehabilitation are diverse and encompass various technologies and interfaces [Citation35]. Systematic reviews have included various VR applications, such as 2D and 3D interactive environments, video-capture interfaces, keyboard- or mouse-based interactions, and recreational game systems viewed on monitors or through head-mounted displays (HMD) [Citation36,Citation37]. The diversity in VR environments may lead to different functional outcomes due to differences in viewing media and the tasks practised [Citation38].
The introduction of VR technology in stroke rehabilitation represents a significant advancement, as it allows stroke patients to work on self-care skills and real-life activities in a setting that may not be feasible within a traditional hospital environment [Citation39]. The ability to simulate real-life activities within VR provides stroke survivors with a unique opportunity to engage in self-care training that closely resembles day-to-day challenges [Citation40]. For VR to be effective in neurorehabilitation, the sense of presence and immersion is crucial [Citation41]. A sense of presence allows users to feel fully engaged in the virtual environment, making transferring acquired abilities and skills to real-world performance more feasible [Citation41]. Ensuring a successful VR neurorehabilitation setting involves creating an immersive and engaging experience that promotes active participation and supports the transfer of rehabilitation gains to real-life functional tasks [Citation40]. While preliminary research has shown promising results, the existing body of literature could be more extensive and often needs comprehensive analyses of VRBR’s impact on various aspects of stroke recovery [Citation42,Citation43]. Moreover, many studies have focused on specific patient populations, potentially limiting the generalizability of their findings to a broader stroke survivor population [Citation44,Citation45]. In particular, existing research on VRBR has predominantly emphasised its effects on motor function improvement, with limited attention paid to other critical domains, such as cognitive rehabilitation, emotional well-being, and social functioning [Citation46,Citation47]. Holistic stroke rehabilitation demands a more comprehensive understanding of how VRBR can address the diverse needs of stroke survivors and facilitate their reintegration into everyday life. Furthermore, the adaptability of VRBR in providing goal-oriented tasks tailored to individual patient needs is a critical aspect that requires further investigation. Understanding how VRBR can optimise brain reorganisation and enhance neuroplasticity is crucial in designing personalised VR interventions that cater to each stroke survivor’s unique challenges and potential. As such, this narrative review’s primary objective is to explore the efficacy of VRBR in stroke survivors. Through an in-depth analysis of the current literature, this review aims to investigate the impact of VRBR on various dimensions of stroke rehabilitation.
Methodology
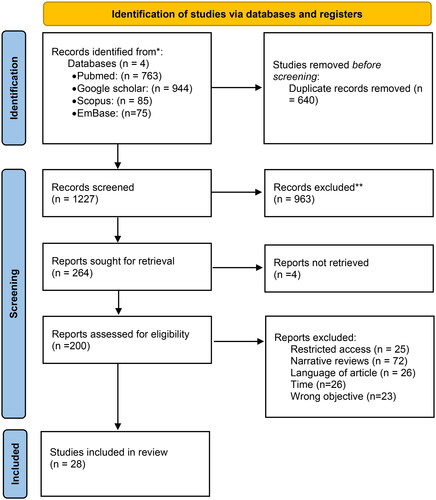
The review aims to provide a comprehensive overview of the efficacy of VRBR in stroke rehabilitation, focusing on its impact on various dimensions of recovery (). A comprehensive search strategy was employed to identify relevant studies published in peer-reviewed journals and academic databases. The search included terms related to stroke rehabilitation, virtual reality, and related synonyms, with Boolean operators used to refine the search. Key databases, such as PubMed, Embase, Scopus, and Google Scholar, were searched for eligible articles (see ).
Table 1. Methodology.
Studies were considered for inclusion if they met the following criteria:
Focus on stroke rehabilitation using Virtual Reality-Based interventions.
Involvement of adult stroke survivors (18 years or older) as the study population.
Publication in English.
Inclusion of outcome measures related to stroke rehabilitation’s physical, cognitive, emotional, communicative, or social aspects.
Clinical trials and randomised controlled trials (RCTs).
Not published more than five years from July 2023 to demonstrate the most recent evidence on the subject of review.
Studies will be excluded if they do not meet the specified criteria or are duplicate publications. The shortlisted articles underwent an extensive quality assessment. During this phase, two reviewers evaluated each article, considering its methodological rigour, relevance to the research question, and potential biases. Articles not meeting the predefined quality standards were excluded from the review. Once the quality assessment was completed, the data extraction process was initiated. The two independent reviewers systematically collected pertinent data from the selected articles. If discrepancies arose during this process, the two reviewers engaged in dialogues to resolve any differences in interpretation. Data extraction included information on the study design, sample characteristics, intervention details, outcome measures, and main findings related to stroke rehabilitation outcomes. The findings from individual studies were summarised qualitatively, and notable trends, themes, or patterns were identified.
Theoretical foundations of virtual reality-based rehabilitation
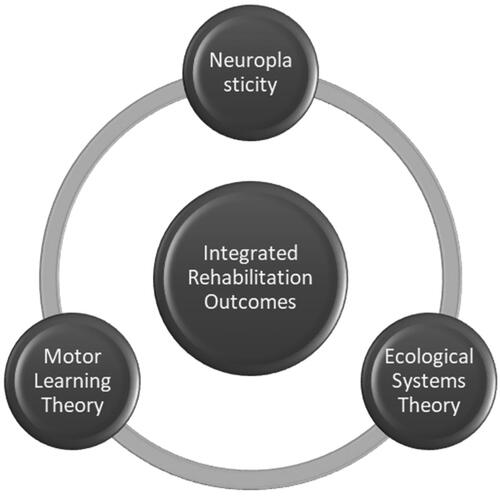
VRBR draws on motor learning, neuroplasticity, and ecological systems theory principles to create a holistic and effective approach to stroke rehabilitation ().
Motor learning
Motor learning theory forms the foundation of VRBR’s skill acquisition and refinement approach [Citation48]. Through repetitive and task-specific exercises, VRBR enables stroke patients to engage in a purposeful practice that targets the reacquisition of motor skills [Citation48]. The immersive and interactive nature of VR environments facilitates the repeated practice of functional movements, allowing patients to fine-tune their motor skills through feedback and error correction [Citation49]. By encouraging active participation in meaningful activities, VRBR fosters the development of motor skills required for daily living tasks, thus improving functional independence and quality of life for stroke survivors [Citation50].
Neuroplasticity
In stroke survivors, reorganising neural pathways is crucial for functional recovery [Citation51]. VRBR capitalises on neuroplasticity by creating stimulating and challenging virtual environments that activate specific brain regions involved in motor planning, execution, and sensory feedback [Citation52]. The real-time feedback VRBR provides enhances neuroplastic changes by promoting the strengthening of existing neural connections and the formation of new ones [Citation53]. This process of brain reorganisation supports the restoration of motor function in stroke survivors, enabling them to regain lost abilities and adapt to their new functional status [Citation53].
Ecological systems theory
VRBR’s approach aligns with ecological systems theory, recognising the interplay between individuals and their environments in shaping development and behaviour [Citation54]. VRBR achieves this by providing personalised and contextually relevant rehabilitation experiences [Citation54]. The virtual environments are tailored to the individual patient’s needs and goals, allowing stroke survivors to engage in activities that mirror real-life scenarios [Citation55]. By immersing patients in familiar and meaningful virtual environments, VRBR promotes functional transfer and generalisation of skills to everyday tasks [Citation56]. This contextualised approach enhances the likelihood of successfully integrating rehabilitative gains into the patient’s daily life, promoting greater functional independence and participation [Citation56].
Integrating motor learning, neuroplasticity, and ecological systems theory within VRBR creates a dynamic, patient-centred rehabilitation approach. The repetitive and task-specific exercises target motor skill acquisition and refinement, while immersive and interactive virtual environments stimulate the brain’s capacity for reorganisation and adaptation [Citation48,Citation51,Citation55]. The contextually relevant and personalised virtual experiences promote skills transfer to real-world settings, enabling stroke survivors to effectively apply their regained abilities in daily living [Citation57]. Moreover, VRBR’s flexibility allows for the design of varied and engaging rehabilitation tasks catering to stroke patients’ diverse needs and goals [Citation58]. This adaptability ensures that therapy remains challenging and motivating, encouraging active participation and commitment to rehabilitation [Citation58]. Furthermore, VRBR’s ability to track and provide immediate feedback on performance enhances stroke patients’ sense of agency and control over their rehabilitation journey [Citation59]. This real-time feedback fosters a positive learning experience, reinforcing successful movements and guiding patients toward error correction, thereby accelerating recovery [Citation60]. By incorporating these theoretical principles into the design and implementation of VRBR, rehabilitation practitioners can offer stroke survivors an innovative and effective approach to recovery [Citation60]. As technology evolves, VRBR holds immense promise in transforming stroke rehabilitation, unlocking new possibilities for functional recovery and improved quality of life for stroke survivors.
VRBR has emerged as a powerful tool in stroke rehabilitation, offering several features that enhance motor learning and neuroplasticity. These elements contribute to its effectiveness in facilitating functional recovery and improving the overall outcomes for stroke survivors. VRBR capitalises on task-specific training, where stroke patients perform exercises closely simulating real-life activities [Citation61]. The virtual environments are designed to replicate everyday tasks, such as reaching for objects, pouring a drink, or dressing, within a safe and controlled setting [Citation62]. This approach enables stroke survivors to focus on refining specific motor skills essential for performing activities of daily living independently [Citation63]. By practising functional movements in the virtual context, patients can work towards regaining lost abilities and improving their functional capacity [Citation63].
Repetition is a fundamental principle of motor learning, as it facilitates the consolidation of motor skills and the establishment of new neural pathways [Citation64]. VRBR allows stroke patients to engage in high-intensity and repetitive practice of targeted movements [Citation65]. Virtual environments’ immersive and interactive nature encourages patients to perform exercises repeatedly, promoting the refinement and automatisation of motor skills [Citation66]. As stroke survivors repeat tasks in the virtual setting, their brain becomes more adept at forming and strengthening neural connections, improving motor control and precision [Citation67].
One of the key advantages of VRBR is its ability to provide real-time and customisable feedback on a patient’s performance. As stroke survivors interact with virtual environments, the system can offer immediate feedback on their movements and actions [Citation68]. Depending on the specific VR system, this feedback may include visual cues, auditory prompts, or haptic responses [Citation68]. Customisable feedback allows therapists to tailor interventions to each patient’s needs, providing targeted cues for improvement and error correction [Citation69]. By receiving instant feedback, stroke survivors can adjust their movements and techniques, facilitating motor learning and enhancing the efficiency of the rehabilitation process [Citation69].
RBR can adapt to exercise challenges based on a patient’s progress and performance [Citation70]. Therapists can adjust the difficulty level of exercises in real time, ensuring that the tasks remain challenging yet attainable for each individual [Citation70]. By gradually increasing the complexity of exercises as patients improve their skills, VRBR promotes continual learning and growth [Citation70]. The adaptive challenges VRBR provides foster neural plasticity, as stroke survivors are encouraged to continually push their boundaries, enhancing brain reorganisation and motor recovery [Citation71].
Motivation and engagement are crucial in stroke rehabilitation, as they significantly influence a patient’s adherence to therapy and overall outcomes [Citation32]. VRBR introduces several elements that enhance motivation and engagement during the rehabilitation process [Citation72]. VR environments’ immersive and interactive nature offers stroke patients a novel and enjoyable experience [Citation73]. Engaging in rehabilitation through VR introduces an element of playfulness, making therapy sessions more enjoyable and encouraging patients to stay committed to their rehabilitation goals [Citation74].
VRBR allows for the customisation of virtual environments to suit individual patient preferences and goals [Citation75]. Participating in activities that resonate with their interests and needs makes stroke survivors more likely to feel a sense of ownership and engagement in their rehabilitation process [Citation76].
Current evidence on the effectiveness of virtual reality-based rehabilitation
Virtual reality (VR) and game-based therapy for stroke rehabilitation
In recent years, VR and Game-Based Therapy have garnered attention as promising strategies in stroke rehabilitation, offering innovative avenues to engage patients in interactive and enjoyable rehabilitation activities [Citation74]. A considerable body of research has been dedicated to examining the effectiveness of these interventions in promoting upper extremity recovery among individuals recovering from strokes [Citation77] ().
Table 2. Study characteristics.
Choi and Paik’s seminal study conducted in 2018 delved into the realm of mobile game-based VR upper extremity rehabilitation, producing compelling evidence that highlights the intervention’s notable efficacy in fostering substantial upper extremity recovery among stroke patients [Citation91]. By strategically leveraging the immersive and interactive features intrinsic to VR technology, synergistically complemented with engaging game-based elements, this therapeutic approach adeptly facilitated patient engagement, catering to rehabilitative objectives and recreational enjoyment. The intersection of these elements carries significant implications, with the potential to enhance patient engagement and adherence through integrating mobile gaming within the VR framework. The tangible success observed in enhancing upper extremity functionality through this modality holds promise for the formulation of future stroke rehabilitation protocols, judiciously exploiting the manifold advantages afforded by VR technology.
Norouzi-Gheidari et al. explored the feasibility and safety of using VRT with an exergame system (Jintronix) as an adjunct to traditional therapy [Citation95]. The study found that VRT using the Jintronixexergame system is feasible and safe. Additionally, the results suggest that this combination therapy may benefit upper extremity functional recovery. This finding holds promise for stroke rehabilitation as it introduces a gamified and engaging approach to therapy. Using exergames in VRT allows patients to perform exercises in a motivating and enjoyable virtual environment, potentially increasing their adherence to rehabilitation programs. The feasibility and safety of incorporating VR technology with traditional therapy offer a flexible and adaptable approach to rehabilitation, catering to the unique needs of stroke patients and promoting more effective recovery outcomes.
In a pioneering inquiry by IkbaliAfsar and colleagues in 2018, the synergy between the Microsoft Xbox 360 Kinect video game system and conventional therapy within stroke rehabilitation was explored [Citation94]. Notably, the study unveiled an intriguing proposition, suggesting that incorporating this gaming system could confer incremental advantages to individuals undergoing post-stroke rehabilitation. The Kinect system’s inherent capacity to facilitate patient interaction with virtual environments through physical movements introduced a dynamic and engaging dimension to the rehabilitative process [Citation97]. This insightful revelation resonates significantly, underlining the potential of gaming technology to augment established conventional rehabilitation strategies. Fusing the Kinect system with established therapeutic protocols brings about a multifaceted spectrum of patient engagement, potentially stimulating heightened patient interest and consequently augmenting adherence, thereby fostering more favourable overall outcomes.
Effectiveness of virtual reality therapy
Virtual reality therapy (VRT) has garnered considerable interest as a novel approach to stroke rehabilitation. Gueye et al. investigated the effectiveness of VRT using the Armeo Spring® upper limb exoskeleton compared to conventional physiotherapy [Citation93]. Their study revealed that VRT with the Armeo Spring® exoskeleton improved upper extremity motor performance more effectively than conventional physiotherapy. The positive outcomes observed in this study demonstrate the potential of combining VR technology with a physical exoskeleton for upper limb rehabilitation. The ability of VRT to engage patients in personalised and immersive exercises, coupled with the assistance provided by the exoskeleton, seems to contribute to superior motor performance outcomes. Furthermore, the finding that the effectiveness of VRT does not diminish with patient age is particularly significant. This suggests that VRT can benefit a broad range of stroke patients, including older individuals, which has important implications for tailoring stroke rehabilitation programs to suit diverse patient populations.
Kiper et al.’s study in 2018 embarked on a discerning exploration of Reinforced Feedback in Virtual Environment (RFVE) therapy, seamlessly integrated with conventional rehabilitation, focusing on restoring upper limb functionality [Citation92]. The study yielded compelling evidence, demonstrating that the amalgamation of RFVE therapy with conventional rehabilitation led to superior outcomes compared to solitary conventional rehabilitation, irrespective of the underlying stroke’s origin. This finding is significant, unveiling the latent potential of reinforced feedback within virtual environments as a dynamic catalyst for accentuating the rehabilitative trajectory. This pivotal achievement is rooted in the astute utilisation of VR technology’s visual and auditory cues, creating an environment conducive to optimal motor learning, ultimately culminating in a more potentiated and efficacious rehabilitative milieu.
On the other hand, de Rooij et al. investigated the effect of VRT compared to non-VRT in improving participation in community-living people after stroke [Citation96]. Surprisingly, their study did not find a statistically significant difference in the effect of VRT on participation compared to non-VRT interventions. The study highlights the need to explore further and refine VRT interventions targeting participation outcomes in community-living stroke patients. It raises questions about the optimal design of VRT interventions and the importance of tailoring them to address individual participation needs, challenges, and preferences.
Virtual reality and dual-task performance
The study by Kayabinar et al. explores the effects of VR-augmented robot-assisted gait training (RAGT) on dual-task performance in chronic stroke patients [Citation98]. The research focuses on the intriguing concept of dual-tasking, which involves performing two tasks simultaneously, a common challenge for stroke survivors during daily activities. In their investigation, the researchers assessed the impact of VR-augmented RAGT on dual-task gait speeds and dual-task performance of chronic stroke patients. Integrating VR technology into RAGT introduces an immersive and interactive element to the rehabilitation process, potentially enhancing the engagement and motivation of patients during therapy. The study’s findings are promising, indicating that VR-augmented RAGT improved dual-task gait speeds and dual-task performance in chronic stroke patients. This suggests that adding virtual reality elements to traditional RAGT positively affects the patient’s ability to manage two tasks simultaneously. The benefits of VR technology in this context could be attributed to its ability to create a stimulating and engaging environment, encouraging patients to focus on both gait training and secondary cognitive tasks simultaneously.
The implications of this study are noteworthy for stroke rehabilitation. Dual-task performance is crucial for individuals to regain functional independence in real-world scenarios [Citation99]. Many daily activities require simultaneous attention to movement and cognitive processing. Therefore, improving dual-task performance can enhance a stroke patient’s ability to perform routine activities with increased efficiency and safety. By demonstrating the positive impact of VR-augmented RAGT on dual-task performance, this study contributes to the growing evidence supporting the use of Virtual Reality in stroke rehabilitation. Incorporating VR technology into traditional therapies holds promise for creating more comprehensive and effective rehabilitation programs tailored to the specific needs of stroke patients. Despite the promising results, it is important to recognise that this is a single study, and further research is needed to corroborate the findings and explore the long-term effects of VR-augmented RAGT on dual-task performance in a larger and more diverse patient population. Nevertheless, the study highlights the potential of VR technology in addressing the complex challenges stroke survivors face during their recovery journey, offering new avenues for enhancing motor and cognitive rehabilitation simultaneously. As technology advances, integrating VR into rehabilitation practices may become a pivotal tool in optimising stroke recovery outcomes and improving stroke survivors’ overall quality of life.
Virtual reality training and serum biomarkers
The studies conducted by Huang et al. explore the impact of VR training on serum biomarkers and motor function in chronic stroke patients, offering valuable insights into the potential benefits of incorporating VR technology into stroke rehabilitation [Citation90]. Huang et al. conducted a study focusing on the effects of immersive VR training on inflammation, oxidative stress, neuroplasticity, and upper limb motor function in chronic stroke patients [Citation90]. By immersing patients in a virtual environment, the researchers aimed to create an engaging and interactive platform to facilitate motor recovery and explore its impact on various serum biomarkers associated with stroke recovery. Huang et al. demonstrated that immersive VR training improved upper limb motor function in chronic stroke patients. Additionally, the study reported positive changes in serum biomarkers, including reduced inflammation and oxidative stress levels and enhanced neuroplasticity in response to VR-based rehabilitation. These findings suggest that VR training may contribute to motor recovery and have potential neuroprotective and reparative effects in the chronic phase of stroke.
The implications of this study are significant for stroke rehabilitation. Virtual Reality offers a novel and engaging approach to rehabilitation, providing a motivating environment for patients to participate in therapy actively. These studies’ positive effects on motor function and serum biomarkers suggest that VR-based interventions can promote physical and neurobiological recovery in chronic stroke patients. By tapping into the principles of neuroplasticity and functional recovery, VR technology may enhance the brain’s ability to rewire and adapt, leading to improved motor outcomes. Additionally, the reduction in inflammation and oxidative stress seen in the studies may indicate a potential neuroprotective effect of VR training in stroke patients, which could have broader implications for stroke management and recovery. However, it is essential to acknowledge that this study is part of a growing body of research on VR training for stroke rehabilitation, and more investigations are warranted to establish its long-term effects and compare its efficacy with traditional rehabilitation approaches.
Other approaches to virtual reality and stroke rehabilitation
Recently, there has been a growing interest in integrating other VR modalities into stroke rehabilitation, including action observation (AO) and the Augmented Reality Rehabilitation System (AR Rehab). These innovative approaches have spurred fresh research on enhancing motor functions, balance, and cognitive abilities among stroke patients. For instance, Errante et al. investigated using AO combined with standard VR to enhance motor functions in adult stroke patients and children with cerebral palsy [Citation84]. By leveraging the concept of mirror neurons through AO therapy, the study aimed to improve motor skills and functional abilities in these populations. The findings suggest that this combined approach holds promise as a novel and potentially effective method to promote motor recovery and rehabilitation in stroke patients and children with cerebral palsy. Traditional modalities, such as the neurological physiotherapy-based approach, were combined with a VR-based program by Peláez-Vélez et al. to investigate the effectiveness of improving motor and balance measures in stroke patients [Citation85]. There were statistically significant improvements in motor function, suggesting that VR-based interventions can augment conventional therapy and yield better outcomes for stroke patients.
Yang et al. explored the feasibility of using AR Rehab for virtual training delivery [Citation86]. They demonstrated that the human-machine integrated mode effectively reduced the burden on rehabilitation professionals while achieving training goals and minimising contact rates during the pandemic, making it a valuable approach to stroke rehabilitation during challenging circumstances. Similarly, Kostenko et al. demonstrated the effectiveness and safety of using a rehabilitation glove (RG) with VR and biofeedback (BFB) to recover hand function in patients during the late recovery period after the first hemispheric ischemic stroke [Citation87]. The results suggest that this combination of VR and BFB technology can effectively enhance hand function recovery in stroke patients, particularly in the later stages of stroke rehabilitation.
Robot-assisted gait training (Lokomat) effectiveness on balance and spatiotemporal parameters of gait in stroke survivors was investigated by Akıncı et al. [Citation88]. The study revealed varying effects on balance and walking, highlighting the potential to tailor VR interventions based on individual patient needs and goals. In a similar study, Kuo et al. evaluated a wearable sensor-based virtual reality game (PABLO system) for improving upper-extremity function in stroke patients [Citation89]. The technology was effective in enhancing hand function and shoulder and elbow movements. It elicitedmore enjoyment from study participants than traditional treatment, suggesting its potential as an engaging and effective tool for stroke rehabilitation. El-Kafy et al. also studied robot-mediated virtual reality gaming to modulate spasticity and improve motor functions in chronic stroke patients [Citation79]. Their findings underline the effectiveness of this approach in enhancing motor recovery and function in the affected upper limbs, emphasising the potential of robotics and VR technology.
Anwar et al. demonstrated the potential of VR-based interventions, as they found virtual reality training to be more effective than conventional physical therapy in restoring balance and lower extremity function [Citation78]. This unique benefit for lower extremity recovery is a promising development in the field. Similarly, Lee et al. examined the potential of a low-cost Kinect-based virtual rehabilitation system for upper limb recovery in subacute stroke patients [Citation83]. While the system did not outperform the sham VR, it did induce more arm motion than the control group, suggesting it could be a valuable supplementary therapy during inpatient stroke rehabilitation.
Meanwhile, Rogers et al. evaluated the Elements virtual rehabilitation system’s efficacy in addressing motor and cognitive recovery post-stroke. The outcomes revealed improvements in upper-limb function and general intellectual status, affirming this system’s comprehensive support to stroke patients [Citation32]. Lee et al. explored the RAPAEL smart glove, a novel tool for targeting upper extremity and cognitive function in chronic hemiparetic stroke survivors [Citation80]. Their study highlighted the beneficial effects of this technology, further suggesting its potential as an innovative tool in stroke rehabilitation.
In pursuing a well-rounded approach, Long et al. delved into additional VR training focusing on self-efficacy and daily living activities in stroke patients [Citation81]. While not superior in upper limb function and occupational performance, VR training positively impacted self-efficacy and daily living activities, positioning it as a valuable complement to conventional therapy. Schuster-Amft et al. compared virtual reality-based training to conventional therapy in stroke rehabilitation [Citation100]. Despite the study population having moderate to severe motor impairments, both groups demonstrated similar effects, with most improvements occurring within the initial two weeks. This indicates the potential of virtual reality-based training, especially for patients with less severe impairments. Ögün et al. explored the effectiveness of immersive VR rehabilitation in enhancing upper extremity function and self-care skills in patients with ischemic stroke [Citation82]. Their study demonstrated the power of immersive VR in augmenting upper extremity function and self-care skills, suggesting it as a valuable tool in stroke rehabilitation.
Comparison with conventional rehabilitation approaches
The distinctions in patient experience between VRBR and conventional rehabilitation methodologies significantly influence the ultimate treatment outcomes. VRBR, with its immersive and interactive attributes, has the potential to engender a profound sense of presence, wherein patients feel fully engrossed and connected to the virtual milieu [Citation101]. This elevated sense of presence can amplify motivation and compliance with therapy, as stroke survivors are more likely to engage in their rehabilitative journey actively. In stark contrast, conventional rehabilitation often falls short in comparable engagement and novelty, consequently leading to waning interest and diminished adherence to prescribed regimens of exercises [Citation102].
A noteworthy advantage of VRBR is its capacity to offer a simulated real-life environment, allowing stroke survivors to practice functional activities within a secure and controlled realm [Citation103]. This aspect holds particular significance when addressing Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs), which bear substantial importance in achieving independence and enhancing the overall quality of life. Through immersion in these virtual contexts, stroke survivors can hone specific motor skills and cognitive capacities requisite for functional autonomy. Contrarily, while conventional rehabilitation may enhance mobility and strength, it may not consistently offer the level of real-life simulation and task-specific training that VRBR provides [Citation38].
Adaptability and progression represent another compelling facet wherein VRBR takes the lead. VR systems can be meticulously tailored to each patient’s capacities and exigencies, enabling therapists to calibrate exercise difficulty levels in real-time [Citation34]. As stroke survivors progress, the virtual environment can be seamlessly customised to incorporate more challenging tasks, ensuring a continued trajectory of improvement and optimising the benefits of neuroplasticity. In contrast, conventional rehabilitation modalities might adhere to predefined protocols, possibly failing to account for the nuanced variations in recovery pace among individuals, potentially resulting in either underutilisation or overloading of patients during therapy sessions [Citation34].
It is imperative, however, to acknowledge the contextual caveat that VRBR does not represent a universally applicable solution. Certain stroke survivors might encounter cognitive or physical limitations that could hamper their effective engagement with virtual environments [Citation104]. Traditional approaches and hands-on techniques inherent to conventional rehabilitation continue to wield substantial efficacy, especially among patients who may not be well-acquainted with or possess access to VR technology. Consequently, a judicious and individualised approach is warranted, delineating the suitability of VRBR to specific patient profiles based on their unique requirements and circumstances.
While the discourse on VRBR within stroke rehabilitation progresses, a critical need surfaces for well-structured comparative studies that directly juxtapose the efficacy of VRBR against conventional rehabilitation methodologies. These studies should encompass a spectrum of outcome measures encompassing functional enhancements, quality-of-life improvements, cost-effectiveness, and patient satisfaction. Furthermore, identifying the patient subgroups that reap the most benefits from VRBR is pivotal, as this understanding will guide the targeted and efficacious integration of VRBR into clinical practice.
The merits of VRBR loom prominently, positioning it as a potent and pioneering avenue within the ambit of stroke rehabilitation. A salient facet among these merits lies in the heightened engagement and motivation it bestows upon stroke survivors [Citation73,Citation105]. The immersive and interactive characteristics of VR environments render therapy enjoyable and captivating, thereby fostering active participation on the part of patients in their rehabilitative journey [Citation106]. This heightened engagement proves particularly advantageous for stroke survivors, offsetting the monotony and lacklustre response often associated with conventional rehabilitation modalities [Citation107]. Through this heightened involvement, patients are more likely to adhere rigorously to their prescribed therapy regimens, ultimately culminating in favourable treatment outcomes [Citation108].
A pivotal advantage of VRBR lies in its emphasis on task specificity. The virtual realm empowers therapists to design exercises and activities that closely mimic real-life scenarios [Citation109]. By honing functional movements and daily living activities within this virtual framework, stroke survivors can fine-tune specific motor and cognitive proficiencies requisite for real-world functionality. This feature substantially enhances the transference of acquired skills to day-to-day tasks, fostering augmented functional autonomy and an enriched quality of life. The real-life simulation facet of VRBR proves particularly invaluable when addressing ADLs and IADLs [Citation110]. Herein, stroke survivors can rehearse these tasks within a secure and controlled milieu, thus augmenting their confidence and competence before attempting them. Through this practice mode, VRBR imparts the skillset necessary for independent living and self-care, consequently lending a robust impetus to their overall rehabilitative trajectory.
Personalisation is a cardinal feature distinguishing VRBR from conventional therapeutic modalities [Citation111]. VR systems can be meticulously tailored to cater to individual patient exigencies and capacities, allowing therapists to adjust task intricacies, intensity, and complexities in alignment with each patient’s progression. This tailored approach ensures that therapy perpetually offers an optimal blend of challenge and feasibility, thereby fueling an ongoing trajectory of improvement and capitalising on the potential of neuroplasticity. Moreover, VRBR offers the convenience of remote accessibility, enabling stroke survivors to pursue therapy within the comforts of their abodes [Citation112]. This attribute is particularly advantageous for individuals grappling with limited mobility or those in remote areas, thereby mitigating the necessity for frequent hospital visits and alleviating the burden on healthcare resources.
However, with its manifold advantages, VRBR confronts several limitations that necessitate careful consideration to optimise its integration within stroke rehabilitation protocols. The issues of cost and equipment requisites, encompassing elements such as head-mounted displays and motion-tracking sensors, might present formidable barriers to universal adoption, especially within resource-constrained healthcare setups [Citation113]. Specialised training for therapists is also a prerequisite to effectively harness and tailor VR technology in consonance with each patient’s therapeutic objectives [Citation114]. Furthermore, the learning curve associated with VR technology could pose challenges, particularly for older adults with severe motor deficits [Citation115]. Ethical concerns about patient privacy, data security, and potential overreliance on technology must also be meticulously addressed.
Moreover, the inherent individual variability in stroke patients’ impairments and recovery trajectories mandates a personalised approach to optimise the therapeutic impact [Citation116]. Each patient’s idiosyncratic requisites and goals must be considered when formulating VRBR programs to realise the most efficacious outcomes. Notwithstanding these challenges, the integration of VRBR within stroke rehabilitation holds substantive promise in enriching functional outcomes and elevating the quality of life for stroke survivors. By addressing the limitations and infusing patient-centric approaches, healthcare practitioners can maximise the potency and adoption of VRBR within stroke rehabilitation paradigms. With the evolution of technology, VR-based rehabilitation is poised to play an increasingly pivotal role in elevating the rehabilitative odyssey and overall well-being of stroke survivors.
Clinical implications and future directions
The findings of this review have several important implications for stroke rehabilitation practice. VRBR shows promise as a valuable adjunct to traditional rehabilitation techniques. The high engagement and motivation levels observed in VRBR can lead to improved patient compliance and better treatment outcomes. Stroke rehabilitation practitioners should consider incorporating VRBR into their treatment protocols to enhance patient participation and promote functional recovery. Furthermore, the task specificity and real-life simulation offered by VRBR can facilitate better transfer of skills to daily living activities. By designing exercises that closely resemble real-world scenarios, therapists can help stroke survivors regain independence in their daily lives more effectively. VRBR’s ability to provide personalised and adaptive challenges is also noteworthy, as it allows therapists to tailor interventions to individual patient needs and progress.
Moreover, VRBR’s potential to enhance neuroplasticity and brain reorganisation can significantly impact stroke recovery. Therapists can promote neural rewiring by engaging stroke survivors in challenging and stimulating virtual environments and improving motor and cognitive functions.
While the current evidence supports the efficacy of VRBR in stroke rehabilitation, there are still some research gaps and areas that warrant further investigation. One key research gap is the need for more rigorous comparative studies between VRBR and conventional rehabilitation methods. Comparative effectiveness research can provide a more comprehensive understanding of the added benefits and cost-effectiveness of VRBR, helping healthcare practitioners make informed decisions regarding its integration into clinical practice. Another area for future investigation is the long-term impact of VRBR on stroke survivors’ functional outcomes and quality of life. Longitudinal studies assessing the sustainability of treatment effects over time can shed light on the durability of VRBR interventions and their potential for promoting lasting improvements in stroke survivors’ well-being. Additionally, more research is needed to explore the optimal dosage and frequency of VRBR interventions for different stroke populations. Determining the most effective treatment intensity and duration can help streamline rehabilitation protocols and maximise treatment outcomes.
To successfully integrate VRBR into clinical settings, several recommendations should be considered. Healthcare institutions should invest in VR equipment and technology to ensure accessibility and availability for stroke rehabilitation programs. While initial costs may be a barrier, long-term cost savings and improved patient outcomes may justify the investment [Citation117]. Also, stroke rehabilitation practitioners should receive comprehensive training in using VRBR technology and designing patient-specific interventions. Ongoing technical support and guidance are essential to ensure therapists can effectively navigate and adapt VRBR systems to meet individual patient needs. Moreover, collaborative efforts between researchers, clinicians, and technology developers can facilitate the development of evidence-based and user-friendly VRBR interventions. Continued research into the usability and effectiveness of VRBR can inform the design of user-friendly and patient-centred virtual environments. Healthcare institutions should prioritise patient education and engagement when introducing VRBR into clinical practice. Informing patients about the potential benefits and risks of VRBR and addressing any concerns or hesitations can increase acceptance and compliance with the technology.
Limitations and strengths of study
This narrative review on the efficacy of VRBR in stroke survivors has several limitations that warrant consideration. One area for improvement is excluding non-English language articles from the analysis, which may have resulted in the omission of relevant studies conducted in languages other than English. This could introduce a language bias and limit the comprehensiveness of the review. Another limitation is the temporal scope of the included studies, which is restricted to those published within the past five years. While this timeframe ensures the incorporation of recent evidence, it may have excluded earlier studies that could have provided valuable insights or established a historical context for the evolution of VRBR approaches. Notwithstanding these limitations, this narrative review presents an up-to-date and comprehensive synthesis of the existing literature, delving into a diverse array of VR applications in stroke rehabilitation.
Conclusion
The exploration of VRBR as a novel approach for stroke survivors reveals a promising and dynamic landscape for enhancing rehabilitation outcomes. Through an in-depth analysis of current evidence, this narrative review underscores the transformative potential of VRBR in addressing the complex challenges of stroke rehabilitation. The synthesis of various studies demonstrates that VRBR’s immersive and interactive nature offers a unique platform for engaging patients in their recovery process. The heightened sense of presence and task-specific simulations create an environment conducive to motivation and active participation. This engagement, often lacking in conventional rehabilitation, has the potential to alleviate the monotony and disinterest that can hinder recovery progress. Moreover, VRBR’s adaptability stands out as a hallmark advantage. The technology’s capacity to tailor exercises to individual patient needs facilitates a personalised and progressive approach to rehabilitation. This adaptability fosters continued improvement and aligns with the diverse recovery trajectories stroke survivors experience.
However, this review also acknowledges the challenges inherent in integrating VRBR into clinical practice. Cost considerations, patient suitability, data security, and the learning curve for healthcare professionals and patients require careful attention. The limitations underscored in the review serve as guidelines for refining the implementation of VRBR and maximising its benefits. While VRBR offers an innovative and exciting path forward, it is not a panacea. Its successful integration depends on a holistic understanding of patient needs, a thoughtful assessment of available resources, and a patient-centred approach. As technology advances and research evolves, collaboration between healthcare professionals, researchers, and patients will be pivotal in optimising VRBR’s application and impact.
Authors contributions
NA and GO conceived the idea for the review and conducted the literature search. Before submission, two independent reviewers were invited to vet the articles included in this review for relevance and accuracy, and their feedback was incorporated into the final version of the manuscript. NA and M0A extracted and analyzed the data. MOA and GA provided critical feedback on the manuscript. NA drafted the initial manuscript. All authors contributed to interpreting the findings, revised the manuscript critically, and approved the final version. NA is the corresponding author and takes full responsibility for the integrity of the work as a whole, from inception to publication.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the reviews.
Additional information
Funding
References
- Singh DK. Stroke management: an overview. IJN. 2023;8(4):1–18. doi: 10.18231/j.ijn.2022.046.
- Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century. Stroke. 2013;44(7):2064–2089. doi: 10.1161/STR.0b013e318296aeca.
- Donkor ES. Stroke in the 21st century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018;2018:3238165–3238110. doi: 10.1155/2018/3238165.
- Matuja SS, Mlay G, Kalokola F, et al. Predictors of 30-day mortality among patients with stroke admitted at a tertiary teaching hospital in northwestern Tanzania: a prospective cohort study. Front Neurol. 2022;13:1100477. doi: 10.3389/fneur.2022.1100477.
- Bamford J, Sandercock P, Dennis M, et al. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337(8756):1521–1526. http://www.thelancet.com/article/014067369193206O/fulltext doi: 10.1016/0140-6736(91)93206-O.
- O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376(9735):112–123. doi: 10.1016/S0140-6736(10)60834-3.
- Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. http://www.thelancet.com/article/S0140673606687709/fulltext doi: 10.1016/S0140-6736(06)68770-9.
- O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–775. from http://www.thelancet.com/article/S0140673616305062/fulltext doi: 10.1016/S0140-6736(16)30506-2.
- Herpich F, Rincon F. Management of acute ischemic stroke. Crit Care Med. 2020;48(11):1654–1663. doi: 10.1097/CCM.0000000000004597.
- Gorelick PB, Whelton PK, Sorond F, et al. Blood pressure management in stroke. Hypertension. 2020;76(6):1688–1695. doi: 10.1161/HYPERTENSIONAHA.120.14653.
- Kitago T, Krakauer JW. Motor learning principles for neurorehabilitation. HandbClin Neurol. 2013;110:93–103.
- Chen X, Liu F, Yan Z, et al. Therapeutic effects of sensory input training on motor function rehabilitation after stroke. Medicine. 2018;97(48):e13387. doi: 10.1097/MD.0000000000013387.
- Grau-Sánchez J, Segura E, Sanchez-Pinsach D, et al. Enriched music-supported therapy for chronic stroke patients: a study protocol of a randomised controlled trial. BMC Neurol. 2021;21(1):19. doi: 10.1186/s12883-020-02019-1.
- Brauer SG, Hayward KS, Carson RG, et al. The efficacy of SMART arm training early after stroke for stroke survivors with severe upper limb disability: a protocol for a randomised controlled trial. BMC Neurol. 2013;13(1):71. https://bmcneurol.biomedcentral.com/articles/10.1186/1471-2377-13-71 doi: 10.1186/1471-2377-13-71.
- Lawrence ES, Coshall C, Dundas R, et al. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke. 2001;32(6):1279–1284. doi: 10.1161/01.str.32.6.1279.
- Rosso C, Lamy JC. Does resting motor threshold predict motor hand recovery after stroke? Front Neurol. 2018;9:1020. doi: 10.3389/fneur.2018.01020.
- Yu Z, Prado R, Quinlan EB, et al. Understanding the impact of stroke on brain motor function: a hierarchical Bayesian approach. J Am Stat Assoc. 2016;111(514):549–563. doi: 10.1080/01621459.2015.1133425.
- Naik SK, Patten C, Lodha N, et al. Force control deficits in chronic stroke: grip formation and release phases. Exp Brain Res. 2011;211(1):1–15. https://link.springer.com/article/10.1007/s00221-011-2637-8 doi: 10.1007/s00221-011-2637-8.
- Belagaje SR. Stroke rehabilitation. Continuum. 2017;23(1):238–253. doi: 10.1212/CON.0000000000000423.
- Coleman ER, Moudgal R, Lang K, et al. Early rehabilitation after stroke: a narrative review. Curr Atheroscler Rep. 2017;19(12):59. doi: 10.1007/s11883-017-0686-6.
- Puderbaugh M, Emmady PD. 2023). Neuroplasticity. In: StatPearls. St. Petersburg (FL): StatPearls Publishing.
- Cirstea MC, Levin MF. Compensatory strategies for reaching in stroke. Brain. 2000;123(5):940–953. doi: 10.1093/brain/123.5.940.
- Saposnik G, Cohen LG. Efficacy and safety of non-immersive virtual reality exercising in stroke rehabilitation (EVREST): a randomised, multicentre, single-blind, controlled trial. Lancet Neurol. 2016;15(10):1019–1027. https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(16)30121-1/fulltext
- Teasell R, Meyer MJ, McClure A, et al. Stroke rehabilitation: an international perspective. Top Stroke Rehabil. 2009;16(1):44–56. doi: 10.1310/tsr1601-44.
- Huang Q, Wu W, Chen X, et al. Evaluating the effect and mechanism of upper limb motor function recovery induced by immersive virtual-reality-based rehabilitation for subacute stroke subjects: study protocol for a randomized controlled trial. Trials. 2019;20(1):104. doi: 10.1186/s13063-019-3177-y.
- Ferrarello F, Baccini M, Rinaldi LA, et al. Efficacy of physiotherapy interventions late after stroke: a meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82(2):136–143. doi: 10.1136/jnnp.2009.196428.
- Pollock A, Farmer SE, Brady MC, et al. Interventions for improving upper limb function after stroke. Cochrane Database Syst Rev. 2014;2014(11):CD010820. 12doi: 10.1002/14651858.CD010820.pub2.
- Bonnyaud C, Gallien P, Decavel P, et al. Effects of a 6-month self-rehabilitation programme in addition to botulinum toxin injections and conventional physiotherapy on limitations of patients with spastic hemiparesis following stroke (ADJU-TOX): protocol study for a randomised controlled, investigator blinded study. BMJ Open. 2018;8(8):e020915. Aug 1doi: 10.1136/bmjopen-2017-020915.
- Nik Ramli NN, Asokan A, Mayakrishnan D, et al. Exploring stroke rehabilitation in Malaysia: are robots better than humans for stroke recuperation? Malays J Med Sci. 2021;28(4):14–23. doi: 10.21315/mjms2021.28.4.3.
- Arcuri F, Porcaro C, Ciancarelli I, et al. Electrophysiological correlates of virtual-reality applications in the rehabilitation setting: new perspectives for stroke patients. Electronics. 2021;10(7):836. doi: 10.3390/electronics10070836.
- Selzer M, Clarke S, Cohen L, et al. Textbook of neural repair and rehabilitation [Internet]. 2014 cited 2023 Aug 2]. Available from: https://books.google.com/books?hl=en&lr=&id=EjA4AwAAQBAJ&oi=fnd&pg=PR13&ots=19wpIzHPUS&sig=RTXwXC5jP_qObsefaIxOToBYqXI.
- Rogers JM, Duckworth J, Middleton S, et al. Elements virtual rehabilitation improves motor, cognitive, and functional outcomes in adult stroke: evidence from a randomized controlled pilot study. J Neuroeng Rehabil. 2019;16(1):56.
- Sramka M, Lacko J, Ruzicky E, et al. Combined methods of rehabilitation of patients after stroke: virtual reality and traditional approach. Neuro Endocrinol Lett. 2020;41(3):123–133.
- Proffitt R, Lange B. Considerations in the efficacy and effectiveness of virtual reality interventions for stroke rehabilitation: moving the field forward. Phys Ther. 2015; 95(3):441–448. doi: 10.2522/ptj.20130571.
- Connelly L, Jia Y, Toro M, et al. A pneumatic glove and immersive virtual reality environment for hand rehabilitative training after stroke. IEEE Trans Neural Syst Rehabil Eng. 2010;18(5):551–559.
- Da M, Cameirão S, Bermúdez I, et al. Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: a randomized controlled pilot study in the acute phase of stroke. PFMJ Verschure Restor Neurol Neurosci. 2011;29:287–298.
- Cameirão MS, Badia SBI, Duarte E, et al. The combined impact of virtual reality neurorehabilitation and its interfaces on upper extremity functional recovery in patients with chronic stroke. Stroke. 2012;43(10):2720–2728. Octdoi: 10.1161/STROKEAHA.112.653196.
- Levin MF, Snir O, Liebermann DG, et al. Virtual reality versus conventional treatment of reaching ability in chronic stroke: clinical feasibility study. NeurolTher. 2012;1(1):1–15.
- Skip A, Rizzo, Kim GJ. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence. 2005;14(2):119–146. https://ieeexplore.ieee.org/abstract/document/6788776/
- Laver KE, Lange B, George S, et al. Virtual reality for stroke rehabilitation. Cochrane Database of Systematic Reviews. 2017;2018(1):CD008349. 20doi: 10.1002/14651858.CD008349.pub4.
- Weiss PL, Kizony R, Feintuch U, et al. Virtual reality applications in neurorehabilitation. Textbook of neural repair and rehabilitation [Internet]. 2023. p. 198–218. [cited 2014 Jun 9]. Available from: https://www.cambridge.org/core/books/textbook-of-neural-repair-and-rehabilitation/virtual-reality-applications-in-neurorehabilitation/DFDDECA59C7113FAA09A87FA39A34E33
- Yetisgin A. Clinical characteristics affecting motor recovery and ambulation in stroke patients. J Phys Ther Sci. 2017;29(2):216–220. doi: 10.1589/jpts.29.216.
- Pervane Vural S, Nakipoglu Yuzer GF, Sezgin Ozcan D, et al. Effects of mirror therapy in stroke patients with complex regional pain syndrome type 1: a randomized controlled study. Arch Phys Med Rehabil. 2016;97(4):575–581. doi: 10.1016/j.apmr.2015.12.008.
- Samuelkamaleshkumar S, Reethajanetsureka S, Pauljebaraj P, et al. Mirror therapy enhances motor performance in the paretic upper limb after stroke: a pilot randomized controlled trial. Arch Phys Med Rehabil. 2014;95(11):2000–2005. doi: 10.1016/j.apmr.2014.06.020.
- LaPiana N, Duong A, Lee A, et al. Acceptability of a mobile phone-based augmented reality game for rehabilitation of patients with upper limb deficits from stroke: case study. JMIR Rehabil Assist Technol. 2020;7(2):e17822. doi: 10.2196/17822.
- Høeg ER, Povlsen TM, Ram J, et al. System immersion in virtual reality-based rehabilitation of motor function in older adults: a systematic review and meta-analysis. Front Virtual Real. 2021;2:647993. doi: 10.3389/frvir.2021.647993.
- Dong Y, Liu X, Tang M, et al. A haptic-feedback virtual reality system to improve the box and block test (BBT) for upper extremity motor function assessment. Virtual Reality. 2023;27(2):1199–1219. doi: 10.1007/s10055-022-00727-2.
- Kleynen M, Beurskens A, Olijve H, et al. Application of motor learning in neurorehabilitation: a framework for health-care professionals. Physiother Theory Pract. 2020;36(1):1–20. doi: 10.1080/09593985.2018.1483987.
- Mazza M, Kammler-Sücker K, Leménager T, et al. Virtual reality: a powerful technology to provide novel insight into treatment mechanisms of addiction. Transl Psychiatry. 2021;11(1):617. doi: 10.1038/s41398-021-01739-3.
- Şahin S, Köse B, Aran OT, et al. The effects of virtual reality on motor functions and daily life activities in unilateral spastic cerebral palsy: a single-blind randomized controlled trial. Games Health J. 2020;9(1):45–52. doi: 10.1089/g4h.2019.0020.
- Balkaya M, Cho S. Optimizing functional outcome endpoints for stroke recovery studies. J Cereb Blood Flow Metab. 2019;39(12):2323–2342. doi: 10.1177/0271678X19875212.
- Hao J, Xie H, Harp K, et al. Effects of virtual reality intervention on neural plasticity in stroke rehabilitation: a systematic review. Arch Phys Med Rehabil. 2022;103(3):523–541. doi: 10.1016/j.apmr.2021.06.024.
- Zhang B, Li D, Liu Y, et al. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: a systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3255–3273. doi: 10.1111/jan.14800.
- Domínguez-Téllez P, Moral-Muñoz JA, Salazar A, et al. Game-based virtual reality interventions to improve upper limb motor function and quality of life after stroke: systematic review and meta-analysis. Games Health J. 2020;9(1):1–10. doi: 10.1089/g4h.2019.0043.
- Huygelier H, Mattheus E, Abeele VV, et al. The use of the term virtual reality in post-stroke rehabilitation: a scoping review and commentary. Psychol Belg. 2021;61(1):145–162. doi: 10.5334/pb.1033.
- Parsons TD. Ethical challenges of using virtual environments in the assessment and treatment of psychopathological disorders. J Clin Med. 2021;10(3):378. doi: 10.3390/jcm10030378.
- Brassel S, Power E, Campbell A, et al. Recommendations for the design and implementation of virtual reality for acquired brain injury rehabilitation: systematic review. J Med Internet Res. 2021;23(7):e26344. doi: 10.2196/26344.
- Aida J, Chau B, Dunn J. Immersive virtual reality in traumatic brain injury rehabilitation: a literature review. NeuroRehabilitation. 2018;42(4):441–448. doi: 10.3233/NRE-172361.
- Szczepańska-Gieracha J, Cieślik B, Rutkowski S, et al. What can virtual reality offer to stroke patients? A narrative review of the literature. NeuroRehabilitation. 2020;47(2):109–120. doi: 10.3233/NRE-203209.
- de Rooij IJM, van de Port IGL, Visser-Meily JMA, et al. Virtual reality gait training versus non-virtual reality gait training for improving participation in subacute stroke survivors: study protocol of the ViRTAS randomized controlled trial. Trials. 2019;20(1):89. doi: 10.1186/s13063-018-3165-7.
- El Amki M, Baumgartner P, Bracko O, et al. Task-specific motor rehabilitation therapy after stroke improves performance in a different motor task: translational evidence. Transl Stroke Res. 2017;8(4):347–350. doi: 10.1007/s12975-016-0519-x.
- Morrison-Smith S, Ruiz J. Challenges and barriers in virtual teams: a literature review. SN Appl Sci. 2020;2(6):1096. doi: 10.1007/s42452-020-2801-5.
- Lokka IE, Çöltekin A, Wiener J, et al. Virtual environments as memory training devices in navigational tasks for older adults. Sci Rep. 2018;8(1):10809. doi: 10.1038/s41598-018-29029-x.
- Kimura T, Nakano W. Repetition of a cognitive task promotes motor learning. Hum Mov Sci. 2019;66:109–116. doi: 10.1016/j.humov.2019.04.005.
- Bui J, Luauté J, Farnè A. Enhancing upper limb rehabilitation of stroke patients with virtual reality: a mini review. Front Virtual Real. 2021;2:595771. doi: 10.3389/frvir.2021.595771.
- Matamala-Gomez M, Slater M, Sanchez-Vives MV. Impact of virtual embodiment and exercises on functional ability and range of motion in orthopedic rehabilitation. Sci Rep. 2022;12(1):5046. doi: 10.1038/s41598-022-08917-3.
- Khan A, Podlasek A, Somaa F. Virtual reality in post-stroke neurorehabilitation - a systematic review and meta-analysis. Top Stroke Rehabil. 2023;30(1):53–72. doi: 10.1080/10749357.2021.1990468.
- Wang P, Wu P, Wang J, et al. A critical review of the use of virtual reality in construction engineering education and training. Int J Environ Res Public Health. 2018;15(6):1204. doi: 10.3390/ijerph15061204.
- Fulvio JM, Rokers B. Use of cues in virtual reality depends on visual feedback. Sci Rep. 2017;7(1):16009. doi: 10.1038/s41598-017-16161-3.
- Qian J, McDonough DJ, Gao Z. The effectiveness of virtual reality exercise on individual’s physiological, psychological and rehabilitative outcomes: a systematic review. Int J Environ Res Public Health. 2020;17(11):4133. doi: 10.3390/ijerph17114133.
- Verrienti G, Raccagni C, Lombardozzi G, et al. Motivation as a measurable outcome in stroke rehabilitation: a systematic review of the literature. Int J Environ Res Public Health. 2023;20(5):4187. doi: 10.3390/ijerph20054187.
- Fregna G, Schincaglia N, Baroni A, et al. A novel immersive virtual reality environment for the motor rehabilitation of stroke patients: a feasibility study. Front Robot AI. 2022;9:906424. doi: 10.3389/frobt.2022.906424.
- Laver KE, Lange B, George S, et al. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017;11(11):CD008349. doi: 10.1002/14651858.CD008349.pub4.
- Gustavsson M, Kjörk EK, Erhardsson M, et al. Virtual reality gaming in rehabilitation after stroke - user experiences and perceptions. Disabil Rehabil. 2022;44(22):6759–6765. doi: 10.1080/09638288.2021.1972351.
- Rose T, Nam CS, Chen KB. Immersion of virtual reality for rehabilitation - review. Appl Ergon. 2018;69:153–161. doi: 10.1016/j.apergo.2018.01.009.
- Norlander A, Iwarsson S, Jönsson AC, et al. Participation in social and leisure activities while re-constructing the self: understanding strategies used by stroke survivors from a long-term perspective. Disabil Rehabil. 2022;44(16):4284–4292. doi: 10.1080/09638288.2021.1900418.
- Erhardsson M, Alt Murphy M, Sunnerhagen KS. Commercial head-mounted display virtual reality for upper extremity rehabilitation in chronic stroke: a single-case design study. J Neuroeng Rehabil. 2020;17(1):154. doi: 10.1186/s12984-020-00788-x.
- Anwar N, Karimi H, Ahmad A, et al. A novel virtual reality training strategy for poststroke patients: a randomized clinical trial. J Healthc Eng. 2021;2021:6598726–6598726. doi: 10.1155/2021/6598726.
- Abd El-Kafy EM, Alshehri MA, El-Fiky AA, et al. The effect of robot-mediated virtual reality gaming on upper limb spasticity poststroke: a randomized-controlled trial. Games Health J. 2022;11(2):93–103. doi: 10.1089/g4h.2021.0197.
- Lee HS, Lim JH, Jeon BH, et al. Non-immersive virtual reality rehabilitation applied to a task-oriented approach for stroke patients: a randomized controlled trial. Restor Neurol Neurosci. 2020;38(2):165–172. doi: 10.3233/RNN-190975.
- Long Y, Ouyang R, Zhang J. Effects of virtual reality training on occupational performance and self-efficacy of patients with stroke: a randomized controlled trial. J NeuroEngineeringRehabil. 2020;17:150. doi: 10.1186/s12984-020-00783-2.
- Ögün MN, Kurul R, Yaşar MF, et al. Effect of leap motion-based 3D immersive virtual reality usage on upper extremity function in ischemic stroke patients. Arq Neuropsiquiatr. 2019;77(10):681–688. doi: 10.1590/0004-282X20190129.
- Lee SH, Lee JY, Kim MY, et al. Virtual reality rehabilitation with functional electrical stimulation improves upper extremity function in patients with chronic stroke: a pilot randomized controlled study. Arch Phys Med Rehabil. 2018;99(8):1447–1453.e1. doi: 10.1016/j.apmr.2018.01.030.
- Errante A, Saviola D, Cantoni M, et al. Effectiveness of action observation therapy based on virtual reality technology in the motor rehabilitation of paretic stroke patients: a randomized clinical trial. BMC Neurol. 2022;22(1):109. doi: 10.1186/s12883-022-02640-2.
- Peláez-Vélez FJ, Eckert M, Gacto-Sánchez M, et al. Use of virtual reality and videogames in the physiotherapy treatment of stroke patients: a pilot randomized controlled trial. Int J Environ Res Public Health. 2023;20(6):4747. doi: 10.3390/ijerph20064747.
- Yang ZQ, Du D, Wei XY, et al. Augmented reality for stroke rehabilitation during COVID-19. J NeuroEngineeringRehabil. 2022;19:136. doi: 10.1186/s12984-022-01100-9.
- Kostenko EV, Petrova LV, Martynov MY, et al. Effektivnost’ reabilitatsii s virtual’noireal’nost’yuibiologicheskoiobratnoisvyaz’yu v vosstanovleniifunktsiikistiposleinsul’ta [Effectiveness of rehabilitation with virtual reality and biofeedback in recovery of hand function after stroke]. Zh Nevrol Psikhiatr Im S S Korsakova. 2023;123(3. Vyp. 2):68–75. doi: 10.17116/jnevro202312303268.
- Akıncı M, Burak M, Yaşar E, et al. The effects of robot-assisted gait training and virtual reality on balance and gait in stroke survivors: a randomized controlled trial. Gait Posture. 2023;103:215–222. doi: 10.1016/j.gaitpost.2023.05.013.
- Kuo FL, Lee HC, Kuo TY, et al. Effects of a wearable sensor-based virtual reality game on upper-extremity function in patients with stroke. Clin Biomech. 2023;104:105944. doi: 10.1016/j.clinbiomech.2023.105944.
- Huang CY, Chiang WC, Yeh YC, et al. Effects of virtual reality-based motor control training on inflammation, oxidative stress, neuroplasticity and upper limb motor function in patients with chronic stroke: a randomized controlled trial. BMC Neurol. 2022;22(1):21. doi: 10.1186/s12883-021-02547-4.
- Choi H, Paik J. Mobile game-based virtual reality program for upper extremity stroke rehabilitation. J Vis Exp. 2018;133:56241. doi: 10.3791/56241.
- Kiper P, Szczudlik A, Agostini M, et al. Virtual reality for upper limb rehabilitation in subacute and chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2018;99(5):834–842.e4. doi: 10.1016/j.apmr.2018.01.023.
- Gueye T, Dedkova M, Rogalewicz V, et al. Early post-stroke rehabilitation for upper limb motor function using virtual reality and exoskeleton: equally efficient in older patients. Neurol Neurochir Pol. 2021;55(1):91–96. doi: 10.5603/PJNNS.a2020.0096.
- Ikbali Afsar S, Mirzayev I, Umit Yemisci O, et al. Virtual reality in upper extremity rehabilitation of stroke patients: a randomized controlled trial. J Stroke Cerebrovasc Dis. 2018;27(12):3473–3478. doi: 10.1016/j.jstrokecerebrovasdis.2018.08.007.
- Norouzi-Gheidari N, Hernandez A, Archambault PS, et al. Feasibility, safety and efficacy of a virtual reality exergame system to supplement upper extremity rehabilitation post-stroke: a pilot randomized clinical trial and proof of principle. Int J Environ Res Public Health. 2019;17(1):113. doi: 10.3390/ijerph17010113.
- de Rooij IJM, van de Port IGL, Punt M, et al. Effect of virtual reality gait training on participation in survivors of subacute stroke: a randomized controlled trial. Phys Ther. 2021;101(5):pzab051. doi: 10.1093/ptj/pzab051.
- Ding WL, Zheng YZ, Su YP, et al. Kinect-based virtual rehabilitation and evaluation system for upper limb disorders: a case study. J Back Musculoskelet Rehabil. 2018;31(4):611–621. doi: 10.3233/BMR-140203.
- Kayabinar B, Alemdaroğlu-Gürbüz İ, Yilmaz Ö. The effects of virtual reality augmented robot-assisted gait training on dual-task performance and functional measures in chronic stroke: a randomized controlled single-blind trial. Eur J Phys Rehabil Med. 2021;57(2):227–237. doi: 10.23736/S1973-9087.21.06441-8.
- San Martín Valenzuela C, Moscardó LD, López-Pascual J, et al. Effects of dual-task group training on gait, cognitive executive function, and quality of life in people with Parkinson disease: results of randomized controlled DUALGAIT trial. Arch Phys Med Rehabil. 2020;101(11):1849–1856.e1. doi: 10.1016/j.apmr.2020.07.008.
- Schuster-Amft C, Eng K, Suica Z, et al. Effect of a four-week virtual reality-based training versus conventional therapy on upper limb motor function after stroke: a multicenter parallel group randomized trial. PLoS One. 2018;13(10):e0204455. doi: 10.1371/journal.pone.0204455.
- Xiong J, Hsiang EL, He Z, et al. Augmented reality and virtual reality displays: emerging technologies and future perspectives. Light SciAppl. 2021;10:216. doi: 10.1038/s41377-021-00658-8.
- Forgea MC, Lyons AG, Lorenz RA. Barriers and facilitators to engagement in rehabilitation among stroke survivors: an integrative review. Rehabil Nurs. 2021;46(6):340–347. doi: 10.1097/RNJ.0000000000000340.
- Hamad A, Jia B. How virtual reality technology has changed our lives: an overview of the current and potential applications and limitations. Int J Environ Res Public Health. 2022;19(18):11278. doi: 10.3390/ijerph191811278.
- Trombetta M, Bazzanello Henrique PP, Brum MR, et al. Motion rehab AVE 3D: a VR-based exergame for post-stroke rehabilitation. Comput Methods Programs Biomed. 2017;151:15–20. doi: 10.1016/j.cmpb.2017.08.008.S0169-2607(17)30113-X.
- Langhorne P, Wagenaar R, Partridge C. Physiotherapy after stroke: more is better? Physiother Res Int. 1996;1(2):75–88. doi: 10.1002/pri.6120010204.
- Hacmun I, Regev D, Salomon R. The principles of art therapy in virtual reality. Front Psychol. 2018;9:2082. doi: 10.3389/fpsyg.2018.02082.
- Eisapour M, Cao S, Boger J. Participatory design and evaluation of virtual reality games to promote engagement in physical activity for people living with dementia. J Rehabil Assist Technol Eng. 2020;7:2055668320913770. doi: 10.1177/2055668320913770.
- Agbangla NF, Séba MP, Bunlon F. SnacktivityTM, giant games and immersive virtual reality exercises: a rapid narrative review of these new physical activity practices among older people living in nursing homes and long-term care facilities. Healthcare. 2022;10(10):1897. doi: 10.3390/healthcare10101897.
- Muñoz J, Mehrabi S, Li Y, et al. Immersive virtual reality exergames for persons living with dementia: user-Centered design study as a multistakeholder team during the COVID-19 pandemic. JMIR Serious Games. 2022;10(1):e29987. doi: 10.2196/29987.
- Al-Jundi HA, Tanbour EY. A framework for fidelity evaluation of immersive virtual reality systems. Virtual Reality. 2022;26(3):1103–1122. doi: 10.1007/s10055-021-00618-y.
- Charles D, Holmes D, Charles T, et al. 2020). Virtual reality design for stroke rehabilitation. In: Rea P, editor. Biomedical visualisation. Advances in experimental medicine and biology. Vol. 1235. Cham: Springer. doi: 10.1007/978-3-030-37639-0_4.
- Thielbar K, Spencer N, Tsoupikova D, et al. Utilizing multi-user virtual reality to bring clinical therapy into stroke survivors’ homes. J Hand Ther. 2020;33(2):246–253. doi: 10.1016/j.jht.2020.01.006.
- Triandafilou KM, Tsoupikova D, Barry AJ, et al. Development of a 3D, networked multi-user virtual reality environment for home therapy after stroke. J Neuroeng Rehabil. 2018;15(1):88. doi: 10.1186/s12984-018-0429-0.
- Baniasadi T, Ayyoubzadeh SM, Mohammadzadeh N. Challenges and practical considerations in applying virtual reality in medical education and treatment. Oman Med J. 2020;35(3):e125–e125. doi: 10.5001/omj.2020.43.
- Rutkowski S, Kiper P, Cacciante L, et al. Use of virtual reality-based training in different fields of rehabilitation: a systematic review and meta-analysis. J Rehabil Med. 2020;52(11):jrm00121. doi: 10.2340/16501977-2755.
- Iachini T, Maffei L, Masullo M, et al. The experience of virtual reality: are individual differences in mental imagery associated with sense of presence? Cogn Process. 2019;20(3):291–298. doi: 10.1007/s10339-018-0897-y.
- Islam MK, Brunner I. Cost-analysis of virtual reality training based on the virtual reality for upper extremity in subacute stroke (VIRTUES) trial. Int J Technol Assess Health Care. 2019;35(5):373–378. doi: 10.1017/S026646231900059X.