?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
To observe the effect of Danzhi Jiangtang capsule (DJC) on the clinical indexes and vascular endothelial function indexes in patients with impaired glucose tolerance (IGT).
Methods
A total of 106 patients were enrolled and randomly assigned to the treatment group and control group following a four-week washout period. The patients in the control group received a general lifestyle intervention, while those in the treatment group received DJC (2.0 g 3× a day) in conjunction with the intervention given to the control group patients. The physiological and biochemical levels, vascular endothelial function indices, and traditional Chinese medicine (TCM) syndrome ratings of the patients in the two groups were compared after 12 weeks of therapy.
Results
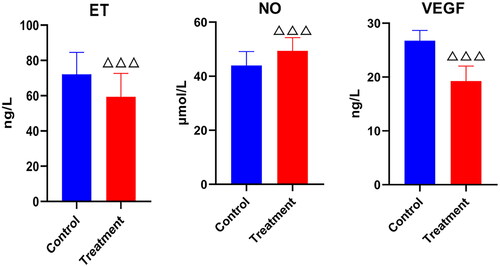
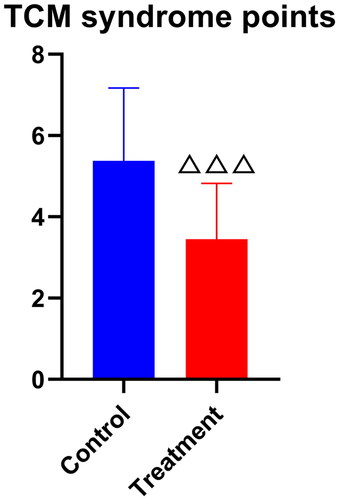
In the control group, the diastolic blood pressure (DBP) was significantly improved compared with those before treatment (83.31 ± 6.47 vs. 79.21 ± 6.17, p < .01) (CI: 1.45, 6.73; Cohen’s d: 10.51), as was the case with the nitric oxide (NO) levels and TCM syndrome points (35.71 ± 4.58 vs. 43.96 ± 5.17, 9.57 ± 2.63 vs. 5.38 ± 1.79, p < .001) (CI: –10.28, –6.24; 3.12, 5.18; Cohen’s d: 0.90). In the treatment group, the levels of fasting blood glucose, endothelin and vascular endothelial growth factor were significantly improved compared with control group (4.92 ± 0.21 vs. 5.59 ± 0.31, 59.37 ± 13.25 vs. 72.13 ± 12.37, 19.25 ± 2.80 vs. 26.76 ± 1.88, p < .001) (CI: 0.55, 0.78; 7.40, 18.13; 6.52, 8.50; Cohen’s d: 4.94, 0.41, 1.32), as was the case with 2-h post-load plasma glucose and total cholesterol (TC) (8.33 ± 0.62 vs. 8.89 ± 1.55, 4.61 ± 1.05 vs. 5.22 ± 1.12, p < .05) (CI: 0.07, 1.07; 0.15, 1.06; Cohen’s d: 0.40, 0.51).
Conclusions
Treatment with DJC could significantly improve the physiological and biochemical indicators, vascular endothelial function, and TCM syndrome points of IGT patients, indicating that DJC could be a potential drug to treat patients with IGT of Qi–Yin deficiency type.
1. Introduction
Diabetes mellitus (DM) is one of the most prevalent chronic diseases among human beings [Citation1]. Prediabetes is regarded as the stage at which a patient’s blood glucose level exceeds the normal range; however, the pertinent diagnostic data do not fulfil the diagnostic criteria for DM [Citation2]. Impaired glucose tolerance (IGT) and impaired fasting glucose (IFG), which can develop alone or together, are both stages of the disease, with IGT being more severe than IFG. According to previous studies, vascular disease affects a significant proportion of both IGT and IFG patients and does not only affect individuals with diabetes [Citation3]. Studies have also demonstrated that approximately 5–10% of patients with prediabetes progress to diabetes each year [Citation4]. However, prediabetes is bi-directional in nature and this stage is completely reversible, and it is feasible to reduce the probability of developing diabetes with intensive intervention to improve the attendant pathological changes.
The DJC compound is composed of Prince’s ginseng (Pseudostellaria paniculate), Rehmannia glutinosa, peony skin, Cuscuta, Alisma orientale and Hirudo. It enters the kidney and bladder meridians and clears the heat and removes the turbidity. In Pharmacognosy Fu, Lei Gong states ‘Alisma orientale is a diuretic and a laxative … while tonifying Yin deficiency’ [Citation5]. The whole formula has the function of tonifying, supporting the positive and eliminating the evil at the same time, tonifying the Qi and nourishing the yin, invigorating the blood, and opening up the ligaments.
Recent research has indicated that DJC contains a variety of effective chemical components, which can effectively enhance the body’s material metabolism. Tansy polysaccharide can reduce the triglyceride (TG) and total cholesterol (TC) levels, exert an antioxidant function, and protect the cardiovascular function [Citation6], while tannin is the main active ingredient of herbal tannin, which has been proven to improve the blood viscosity, vascular endothelial function and anti-platelet aggregation in diabetic rats [Citation7]. Meanwhile, the phenylethanols, flavonoids, violetone, triterpenoids and alkene-terpenoids contained in Rehmannia glutinosa can regulate the blood sugar and lipid levels, while the compound also has significant therapeutic effects on cardiovascular diseases [Citation8]. Finally, leechin has the effects of improving the blood rheology, regulating the lipid metabolism, protecting the vascular endothelial function, and correcting any chronic inflammation of diabetic vascular lesions [Citation9].
The aim of the current study is to observe the impact of Danzhi Jiangtang capsule (DJC) treatment on the enhancement of the vascular endothelial function and the associated clinical indices in IGT patients with Qi and Yin deficiency, to accurately assess the clinical efficacy of the treatment, and to provide a basis for the pharmaceutical prevention and treatment of prediabetes in view of reducing the conversion rate of this condition to diabetes.
2. Materials and methods
2.1. Diagnostic criteria
The diagnostic criteria for IGT were based on the 1999 WHO Diabetes Diagnosis and Typing Criteria [Citation10]: fasting blood glucose (FPG) ≤7.0 mmol/L and 7.8 mmol/L ≤ oral glucose tolerance test (OGTT) 2-h post-load plasma glucose (2hPG) ≤11.1 mmol/L. The diagnostic criteria for traditional Chinese medicine (TCM) symptoms were based on the national standard definition of Qi–Yin deficiency [Citation11]. The main symptoms include fatigue, hypoxia and fewer words, thirst and dry tongue, hot flashes, and night sweats, while the secondary symptoms include emaciation, less urine, constipation, red tongue, teeth marks on the edge of the tongue, thin and dry tongue coating, thin and weak pulse or weak count. Any individual who has two of the main symptoms and three of the secondary symptoms can be diagnosed as having Qi–Yin deficiency. According to the ‘Guidelines for the Prevention and Treatment of Diabetes Mellitus in Chinese Medicine’ [Citation12], the quantitative criteria for grading symptoms in TCM assess the severity of each symptom of Qi–Yin deficit. The major symptoms are given 0, 2, 4 and 6 points for absence of symptoms, mild symptoms, moderate symptoms and severe symptoms, respectively, while the secondary symptoms are given 0, 1, 2 and 3 points for absence of symptoms, mild symptoms, moderate symptoms and severe symptoms, respectively.
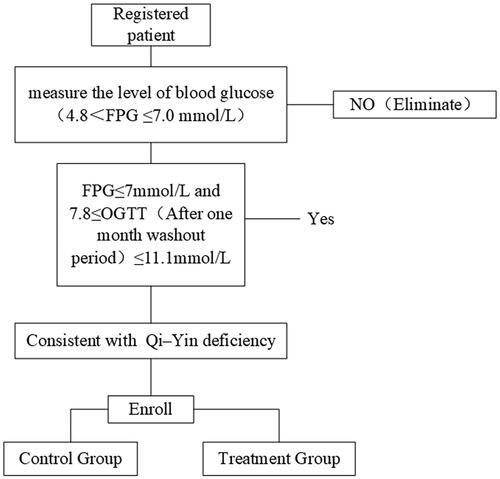
2.2. Inclusion and exclusion criteria
The following inclusion criteria applied: (1) patients meeting the diagnostic criteria; (2) patients diagnosed with IGT after a one-month elution period; (3) patients aged 18–65; (4) patients who had not participated in other drug clinical trials within three months; and (5) patients who voluntarily signed the informed consent.
The exclusion criteria were as follows: (1) patients experiencing acute cardiovascular and cerebrovascular events within six months; (2) patients with severe liver and kidney dysfunction; (3) patients with malignant tumours or psychiatric diseases; (4) pregnant or lactating women; and (5) patients combined with other endocrine diseases or other serious primary diseases.
The inclusion process is shown in .
2.3. General information
The enrolled patients were IGT patients admitted to the outpatient clinic of the Department of Endocrinology at Anhui University of Traditional Chinese Medicine’s First Affiliated Hospital between August 2021 and January 2022. Using a Roche blood glucose meter, the terminal blood sugar levels of 1756 high-risk diabetic patients were assessed before 517 cases that met the IGT diagnostic criteria were initially selected. An OGTT was conducted after three days of a light diet, and a total of 128 patients were found to meet the diagnostic criteria. Four weeks later, the test was repeated, and a total of 106 patients satisfied the inclusion criteria. These patients were then divided into the control group (n = 53) and the treatment group (n = 53) using a totally randomized design procedure.
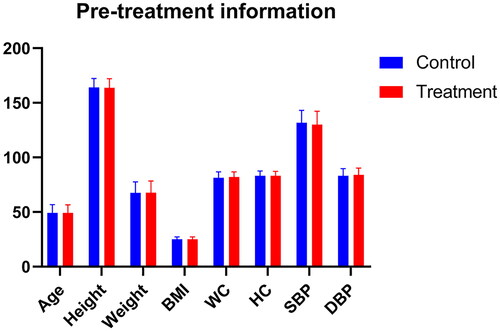
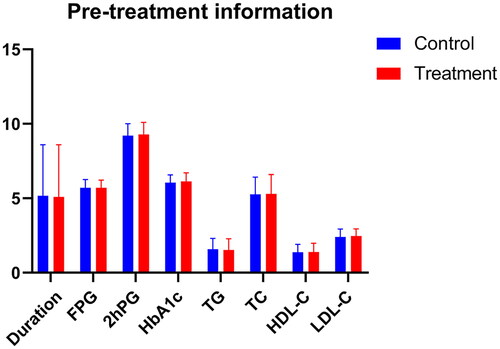
As shown in and and , there were no statistically significant differences between the two groups in terms of age, gender, illness duration, height, weight, body mass index (BMI), waist circumference (WC), hip circumference (HC), low-density lipoprotein cholesterol (LDL-C), FPG, high-density lipoprotein cholesterol (HDL-C), 2hPG, haemoglobin (Hb)A1c, TG, TC, systolic blood pressure (SBP), diastolic blood pressure (DBP).
Table 1. Comparison of general information between the two groups of patients (x ± s).
2.4. Study method
In this clinical trial, we chose a single-blind approach, the control patients took the compound simulated capsule, the treatment group took DJC, but they did not know. In the control group, general lifestyle interventions were administered, which were formulated with reference to the ‘Chinese Guidelines for the Prevention and Treatment of Type 2 Diabetes’ [Citation13] and ‘Evidence-based Clinical Practice Guidelines for Chinese Medicine in Prediabetes Mellitus’ [Citation2], and included diabetes health education, dietary control and Baduanjin exercise. In the treatment group, DJC (Anhui Pharmaceutical Preparation Z20090006, Patent No. ZL200310112845.1) was added to the interventions in the control group and taken orally (2.0 g 3× daily). The elution period was four weeks, while the observation period was 12 weeks.
2.5. Observation indexes and methods
The clinical symptoms, signs and tongue and pulse characteristics of the patients in TCM were recorded. The FPG, 2hPG, glycated haemoglobin (HbA1c), TG, TC, HDL-C and LDL-C were measured via macro-biochemistry, while the endothelin (ET), nitric oxide (NO) and vascular endothelial growth factor (VEGF) were measured using an ELISA® (Shanghai Keshun Science and Technology Co., Ltd., Shanghai, China; KS11995, KS12350, KS10470) kit. The experimental methods were carried out according to the instructions. The safety observation indexes included general physical examination items and blood and urine routine, liver and kidney function, and electrocardiogram assessments.
2.6. Efficacy criteria
2.6.1. Main efficacy criteria
Based on the changes in the laboratory test results, the American Diabetes Association (ADA) ‘Prediabetes Consensus’ [Citation14] was adopted as the standard. The following criteria were used: obvious effective = FPG <7.0 mmol/L, 2hPG <7.8 mmol/L; effective = FPG <7.0 mmol/L, 2hPG ≥7.8 mmol/L and <11.1 mmol/L; ineffective = FPG ≥7.0 mmol/L, or 2hPG ≥11.1 mmol/L after treatment.
2.6.2. Secondary efficacy criteria
(1) In terms of the TCM single symptoms, the efficacy was determined with reference to the ‘Guidelines for the Prevention and Treatment of Diabetes Mellitus in Chinese Medicine’ [Citation7] as follows: an obvious effect means the original symptoms disappeared, or the original symptoms were improved by two levels; the treatment was effective if the symptoms improved by one level but did not disappear; the treatment was ineffective if there was no change in the symptoms. Effective rate (%) = (obvious effect + effective)/total number of cases × 100%.
(2) The criteria for determining the efficacy in terms of TCM symptoms were formulated as follows, again with reference to the ‘Guidelines for the Prevention and Treatment of Diabetes Mellitus in Chinese Medicine’ [Citation15]: Clinical cure = overall disappearance of the TCM clinical symptoms and signs, and reduction in symptom score of >90%; obvious effect = the clinical symptoms and signs improved significantly, with a 70% ≤symptom score reduction <90%; effective = the clinical symptoms and signs were improved, 30% ≤symptom score reduction <70%; ineffective = the clinical symptoms and signs were not significantly improved, or were even worsened, and the reduction in symptom score was <30%. Effective rate (%) = (clinical cure + obvious effect + effective)/total number of cases × 100%. TCM syndrome points is an independent evaluation system for TCM syndromes. The decrease of TCM syndrome points means the clinical improvement of TCM syndromes. These ratios are determined by the evaluation criteria of TCM syndromes.
2.7. Statistical methods
The data were analysed using SPSS 24.0 statistical software (SPSS Inc., Chicago, IL), which we had obtained a copyright license. Any non-normally distributed data were subjected to logarithmic transformation to achieve near normal distribution, with the normally distributed data expressed as . Differences within groups were compared using paired t-test, and differences between groups were compared using single sample t-test. The software automatically generates 95% confidence intervals. The effect size formula of the paired sample t-test was Cohen’s d = Cohen’s d = t/√(n – 1), and the effect size formula of the independent sample t-test was Cohen’s d = (M1 – M2)/√Pooled Variance.
3. Results
3.1. Shedding situation
All patient information was used at the time of enrolment, and patients who did not come to us at the end of the examination did not provide us with additional information. At the end of the study, seven patients in the control group and nine patients in the treatment group were excluded from the study due to poor compliance, an inability to continue contact, or adverse events. The data shedding rate was 13.21% in the control group and 13.98% in the treatment group.
3.2. Comparison of the main clinical symptoms of the patients in the two groups
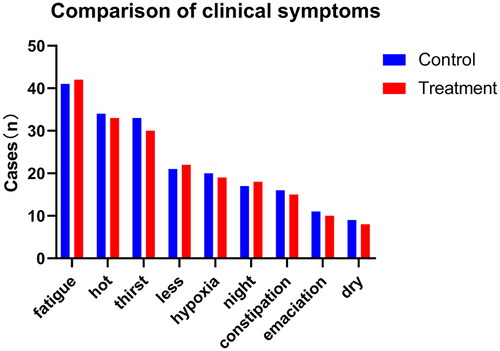
Among the 106 patients with IGT of Qi–Yin deficiency type, fatigue appeared most frequently, followed by hot flashes, while dry tongue appeared the least frequently (, ).
Table 2. Comparison of the main clinical symptoms between the two groups (case (%)).
3.3. Comparison of physiological and biochemical indexes and vascular endothelial function indexes in the two groups
Among the physiological and biochemical indexes, the DBP exhibited significant improvement in the control group after treatment (p < .01), while the FPG, 2hPG, weight, BMI, WC, TG, TC, LDL-C and DBP exhibited significant improvement in the treatment group following the treatment (p < .05). Here, the improvement in FPG, 2hPG and TC was more significant in the treatment group than in the control group (p < .05) ( and , and ).
Figure 5. Comparison of physiological data after treatment. △p < .05 compared with the control group.
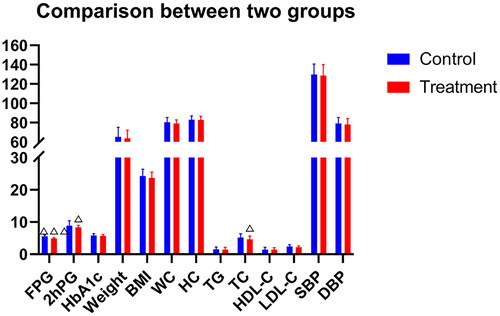
Table 3. Comparison of physiological and biochemical indexes between the two groups ().
Table 4. Comparison of vascular endothelial function indexes between two groups (x ± s).
In terms of the vascular endothelial function factors, the control group exhibited significant improvement in NO levels following treatment (p < .001), while the treatment group exhibited significant improvement in ET, NO and VEGF levels following treatment (p < .05), with the degree of improvement significantly higher than that in the control group (p < .001).
3.4. Efficacy in terms of traditional Chinese medicine syndrome
3.4.1. Comparison of syndrome points between the two groups
Prior to treatment, the difference between the two groups was not statistically significant (p > .05); following treatment, the TCM syndrome points of both groups were lower than those before treatment (p < .001), with the degree of improvement higher in the treatment group than in the control group (p < .001) ( and ).
Table 5. Comparison of the TCM syndrome points (x ± s).
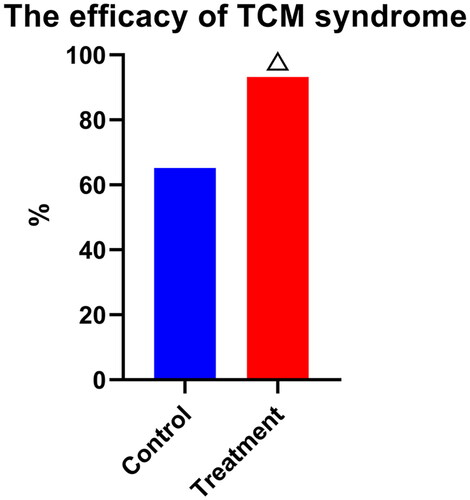
3.4.2. Comparison of the efficacy between the two groups
Following treatment, the total effective rate of the treatment group was higher than that of the control group (p < .01) ( and ).
Table 6. Comparison of the efficacy of TCM syndrome.
3.5. Comparison of treatment safety and shedding rate between the two groups
Following treatment, three cases of adverse events occurred, all of which involved gastrointestinal symptoms. There was one case of adverse events in the control group (1.89%) and two cases in the treatment group (3.77%), and the difference was not statistically significant between the two groups (p > .05). There was no significant effect on the blood and urine routine, liver and kidney function, and electrocardiogram assessments before and after treatment in either group.
4. Discussion
Prediabetes is a high-risk factor for cardiovascular diseases, diabetes, tumours and other diseases. A national epidemiological survey study on diabetes conducted by the Chinese Medical Association Diabetes Branch in 2007–2008 indicated that the prevalence of prediabetes in China’s adult population was 15.5% [Citation13]. In contrast, a Chinese epidemiological study of diabetes conducted in 2020 indicated that the prevalence of prediabetes among the adult population in China was 35.2% [Citation16]. While the difference in diagnostic criteria led to a large difference in the data obtained by the two surveys, the findings clearly indicate that the population of prediabetes patients in China is huge, with the burden of prediabetes prevention and treatment correspondingly massive.
While there remains some controversy in mainstream evidence-based medicine regarding whether pharmacological interventions should be carried out in terms of prediabetes [Citation15], the value of the theory of ‘treating the untreated’ in TCM as a complementary therapy for mainstream evidence-based medicine is evident in clinical practice. The Chinese DaQing study indicated that lifestyle interventions for IGT are the key to the primary prevention of diabetes, and that the main measures for preventing and treating IGT are not only lifestyle changes, but also include pharmacological treatment for reducing the risk of DM, often using drugs such as acarbose and metformin.
The results of previous studies suggest that the diagnosis and treatment of IGT patients should be based on the improvement in FPG and a significant improvement in postprandial blood glucose, since IGT patients mainly have impaired islet beta-cell function and increased skeletal muscle insulin resistance. However, in 2010, the ADA also set the HbA1c level at 5.7–6.4% as one of the diagnostic criteria for prediabetes [Citation17], which reduced the incidence of cardiorenal injury in patients to a certain extent.
Based on previous clinical studies on prediabetes, the current study explored the intervention effect of DJC on IGT patients, and aimed to identify intervention methods based on TCM in view of reducing the prevalence of IGT, reducing the probability of prediabetes developing into diabetes, and providing a theoretical and clinical basis for the prevention and treatment of diabetes.
A total of 1756 patients at high risk of diabetes were initially screened, and 106 patients with IGT were finally included for clinical observation. After three months of intervention, the results indicated that the clinical symptoms of IGT could be significantly improved and the TCM syndrome points reduced with the use of DJC. In fact, DJC could improve the clinical physiological and biochemical indexes while improving the levels of factors related to vascular endothelial function, which could protect this function and delay the onset and development of vascular injury in IGT patients. DJC is a complex formulation composed of six traditional Chinese medicinal herbs: Prince’s ginseng, Rehmannia glutinosa, peony skin, Cuscuta, Alisma orientale and Hirudo. Each herb contributes its unique pharmacological effects, synergistically exerting a comprehensive regulatory influence on prediabetes. The actions of Prince’s ginseng and Rehmannia glutinosa may correlate with the enhancement of energy metabolism and the modulation of insulin signalling pathways, which are crucial in the regulation of insulin sensitivity and islet beta-cell function. Prince’s ginseng is posited to augment the body’s overall energy metabolism, thereby improving insulin sensitivity and countering insulin resistance [Citation18,Citation19]. Rehmannia glutinosa, with its polysaccharides and saponins, is hypothesized to confer protective effects on islet beta cells, potentially decelerating their functional decline [Citation20]. The anti-inflammatory properties of the DJC represent another pivotal mechanism by which it may influence prediabetic states. Active compounds such as hirudin, found in Hirudo, are recognized for their anticoagulant and anti-inflammatory effects and may mitigate islet inflammation by dampening inflammatory pathways [Citation21]. Peony skin, rich in paeoniflorin, could attenuate low-grade systemic inflammation through the reduction in the synthesis and release of inflammatory mediators, a process of particular importance for the preservation of islet beta-cell function in the context of prediabetes [Citation22]. Oxidative stress attenuation is facilitated by the antioxidant constituents within the DJC, notably the antioxidants present in Cuscuta. These components may shield islet cells from oxidative damage by diminishing the generation of reactive oxygen species and bolstering the activity of the antioxidative enzyme systems. This protective role is vital for the prevention and delay of islet beta-cell dysfunction in prediabetes. Furthermore, the blood-activating and stasis-resolving effects of Alisma orientale and Hirudo may enhance islet blood supply and counteract microvascular complications by improving microcirculation and reducing blood viscosity [Citation23]. This not only aids in maintaining islet beta-cell functionality but may also decrease cardiovascular risks associated with prediabetes.
The TCM mechanism of the above effects may relate to the effect of nourishing the Qi and Yin [Citation24], improving the body’s healthy Qi and removing the evil of turbidity and stasis. At the same time, the short-term therapeutic effect on glycaemic control and reversal in the treatment group suggests that DJC may play a role in reversing the adverse glycaemic levels in IGT patients, thereby reducing the probability of progression from prediabetes to diabetes.
This clinical observation trial involved the limitations of a short observation period and a lack of long-term efficacy data. As such, whether the combined treatment can fundamentally delay or reverse the progression of IGT to diabetes remains inconclusive. In subsequent studies, the intervention effect of DJC on patients with prediabetes will be further analysed, and a more detailed and scientific basis and further clinical evidence will be provided for drug-based evaluations of DJC in view of enriching the basis and clinical evidence for the efficacy of TCM interventions in the treatment of prediabetes.
Author contributions
Conception and design of the research: Zhaohui Fang, Jindong Zhao and Ruimin Lu. Acquisition of data: Zheng Bi, Di Wu and Yixuan Lin. Analysis and interpretation of the data: Jindong Zhao, Yixuan Lin, and Sihai Wang. Statistical analysis: Sihai Wang, Ruimin Lu, and Zheng Bi. Obtaining financing: Zhaohui Fang. Writing of the manuscript: Zhaohui Fang and Zheng Bi. Critical revision of the manuscript for intellectual content: Zheng Bi and Jindong Zhao. All authors read and approved the final draft.
Ethical approval
This study was conducted with approval from the Ethics Committee of The First Affiliated Hospital of Anhui University of Traditional Chinese Medicine (2015AH-32(Z)). This study was conducted in accordance with the Declaration of Helsinki.
Consent form
Written informed consent was obtained from all participants.
Supplemental Material
Download Zip (174.7 KB)Acknowledgements
The registration number: ChiCTR2100049613.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- American Diabetes Association Professional Practice Committee. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl. 1):1–9. doi: 10.2337/dc22-S002.
- Fang Z, Tong X, Duan J, et al. Evidence-based clinical practice guidelines for Chinese medicine in prediabetes mellitus. J Tradit Chin Med. 2017;58(3):268–272.
- Liu H, Ni Y, Wang H, et al. Effect of Danzhi Jiangtang capsule on vascular endothelial function in diabetic patients. Chin Tradit Chin Med Emerg. 2008;17(12):1670–1671.
- Chinese Experts Consensus of clinical intervention for pre-diabetes (draft for comments). Drug Eval. 2019;16(7):3–12.
- Wang S, Fang Z, Ni Y, et al. Effects of Danzhi Jiangtang capsules on renal TGF-β1/Smad3 signaling pathway and AGEs/RAGE level in diabetic nephropathy rats. Chin J Tradit Chin Med. 2021;36(4):2019–2024.
- Fu Y, Zhang H, An Z, et al. Effects of Pseudostellaria heterophylla fibrous root powder and the polysaccharide on immune function of spleen deficiency rats. J Chin Vet Med. 2021;40(4):12–15.
- Bai Q. Influence of endothelial function and blood rheology in diabetic rats by paeonol and tanshinol. Chin J Exp Formul. 2015;21(3):110–113.
- Chen J, Zhang K, Liu Y, et al. Research progress on chemical constituents and pharmacological actions of Rehmannia glutinosa. Chin Herb Med. 2021;52(6):1772–1784.
- Huang Y, Wang J, Wang Y, et al. Pharmacological mechanism and clinical study of qiming granules in treating diabetic retinopathy based on network pharmacology and literature review. J Ethnopharmacol. 2023;302(Pt A):115861. doi: 10.1016/j.jep.2022.115861.
- World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Geneva: World Health Organization, Department of Noncommunicable Disease Surveillance; 1999. p. 4–7.
- National Standardization Administration Committee. Chinese medicine clinical diagnosis and treatment terminology. Part 2: evidence: GB/T 16751.2-2021. Beijing: China Standard Publishing House; 2021. p. 238.
- Chinese Society of Traditional Chinese Medicine. Guidelines for the prevention and treatment of diabetes mellitus in Chinese medicine. Beijing: China Chinese Medicine Press; 2007. p. 1–3.
- Chinese Medical Association, Diabetes Branch. Chinese guidelines for the prevention and treatment of type 2 diabetes mellitus (2020 edition). Int J Endocrinol Metab. 2021;41(5):482–548.
- American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2007;30(1):4–41.
- You L, Yu D, Fang Z, et al. Exploration of clinical research on prediabetes based on evidence-based Chinese medicine. Chin J Tradit Chin Med. 2020;35(3):1343–1346.
- Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–959. doi: 10.1001/jama.2013.168118.
- American Diabetes Association. Standards of medical care in diabetes – 2010. Diabetes Care. 2010;33(Suppl. 1):S11–S61. Erratum in: Diabetes Care. 2010;33(3):692. doi: 10.2337/dc10-S011.
- Da J, Wang Q, Wang Y, et al. Quantitative analysis of eight ginsenosides in red ginseng using ginsenoside Rg1 as single reference standard. World J Tradit Chin Med. 2021;7(1):1–5. doi: 10.4103/wjtcm.wjtcm_82_20.
- Fang Z, Hu X, Chen Z, et al. Radix pseudostellariae of Danzhi Jiangtang capsule relieves oxidative stress of vascular endothelium in diabetic macroangiopathy. Saudi Pharm J. 2020;28(6):683–691. doi: 10.1016/j.jsps.2020.04.009.
- Liu Y, Zhu R, Liu B, et al. Antidiabetic effect of Rehmanniae Radix based on regulation of TRPV1 and SCD1. Front Pharmacol. 2022;13:875014. doi: 10.3389/fphar.2022.875014.
- Huang H, Lei R, Li Y, et al. Hirudo (Leech) for proliferative vitreous retinopathy: a protocol for systemic review and meta-analysis. Medicine. 2021;100(3):e24412. doi: 10.1097/MD.0000000000024412.
- Min C, Liu H, Zhan F, et al. Effect of cortex moutan on PGI2, TXA2, ET and NO in diabetic rats. Tradit Chin Med Mater. 2007;30(6):687–690.
- Ma JX, Wang B, Li HS, et al. Uncovering the mechanisms of leech and centipede granules in the treatment of diabetes mellitus-induced erectile dysfunction utilising network pharmacology. J Ethnopharmacol. 2021;265:113358. doi: 10.1016/j.jep.2020.113358.
- Cheng S, Fang Z. DJC in the treatment of type 2 diabetes vascular lesions mechanism study. J Liaoning Tradit Chin Med J. 2013;40(5):861–864.