Abstract
Background
Rapid Cycle Deliberate Practice (RCDP) has gained prominence in recent years as an innovative teaching method in simulation-based training for adult and pediatric emergency medical skills. However, its application in the training of forceps delivery skills among obstetrics and gynecology residents remains unexplored. This study aimed to assess the impact of RCDP in this domain.
Methods
Conducted in March 2021, this randomized controlled study involved 60 second-year obstetrics and gynecology residents undergoing standardized training. Participants were randomly assigned to the RCDP group or the traditional teaching method (TTM) group, each comprising 30 residents. The RCDP group followed the RCDP practice mode, while the TTM group adhered to conventional simulation teaching. Post-training assessment of operational proficiency was conducted immediately and after one year. Independent operational confidence and training satisfaction were evaluated through questionnaire surveys and the Satisfaction with Simulation Experience (SSE) scale. Data analysis utilized SPSS 23.0.
Results
The RCDP group displayed significantly higher immediate post-training forceps operation scores compared to the TTM group (92.00 [range: 90.00–94.00] vs. 88.00 [range: 86.75–92.00]; z = 3.79; p < .001). However, no significant difference emerged in forceps operation scores after one year (86.00 [range: 85.00–88.00] vs. 85.50 [range: 84.00–88.25]; z = 0.54; p = .59). The RCDP group exhibited notable performance improvement over the TTM group (z = 3.49; p < .001). Independent operation confidence showed no significant discrepancy (p > .05). Importantly, the RCDP group reported higher satisfaction scores, particularly in the Debriefing and Reflection subscale (44.00 [range: 43.00–45.00] vs. 41.00 [range: 41.50–43.00]; z = 5.24; p < .001), contributing to an overall superior SSE score (z = 4.74; p < .001).
Conclusions
RCDP exhibits immediate efficacy in elevating forceps delivery skills among residents. However, sustained skill enhancement necessitates innovative approaches, while RCDP’s value lies in tailored feedback and reflection for enriched medical education.
Key Messages
Rapid Cycle Deliberate Practice (RCDP) demonstrates immediate effectiveness in enhancing forceps delivery skills among obstetrics and gynecology residents, leading to improved immediate performance, which also increased their satisfaction with the teaching process and operational confidence.
Long-term skill retention through RCDP appears limited, highlighting the importance of ongoing reinforcement to prevent skill decay and maintain proficiency.
1. Introduction
Maternal deaths due to intrapartum complications account for 50% of all maternal deaths[Citation1]. The prolonged second stage of labor can easily cause postpartum hemorrhage, puerperal infection, asphyxia of newborns, and other serious consequences [Citation2]. Vaginal delivery techniques, such as forceps and vacuum-assisted delivery, are important skills that obstetricians and midwives must acquire expertise in to handle the second stage of labor [Citation3]. These techniques are also effective measures to address maternal dystocia, reduce the rate of cesarean sections, and improve the rate of vaginal delivery. The successful natural delivery by the puerpera depends closely on the obstetricians’ and midwives’ mastery of obstetrics skills. Skillful and appropriate application of the required techniques by the operator can reduce the occurrence of serious maternal and infant complications [Citation4].
In recent years, both locally and abroad, the rate of vaginal midwifery has been declining. Currently, the global rate of fetal head attraction midwifery is 2.7%, and forceps midwifery is 0.6% [Citation5]. The study revealed that the rate of vaginal births in some parts of China also declined from 1993 (10.6%) to < 1% in 2010 [Citation6]. Two large multicenter studies respectively reported that the rate of vacuum-assisted delivery and forceps delivery in China were 3.3% and 1.9% in 2002, whereas the rate of vaginal surgery including forceps and vacuum-assisted delivery was 1.107% in 2011 [Citation7, Citation8]. This decline is associated with obstetricians’ lack of proper grasp of forceps technology and their preference for cesarean delivery when dealing with dystocia [Citation9].
Due to limited experience of gynecology and obstetrics (G&O) residents in clinical practice and the urgency of forceps delivery time, residents have fewer opportunities to practice and hence possess limited ability to perform the operation. The ‘Practice Bulletin’ from The American College of Obstetricians and Gynecologists (ACOG) [Citation10] requires senior G&O physicians to master at least one vaginal operation technique; it is particularly important for G&O residents to be adequately trained in midwifery skills. However, when dystocia occurs during natural delivery, the circumstances regarding the mother and child are critical; it is therefore difficult to conduct one-on-one bedside teaching. At present, forceps training and teaching include simulation teaching, network teaching and other multi-mode attempts, as well as virtual simulation workshops [Citation11–13].
Rapid Cycle Deliberate Practice (RCDP) is a novel skill teaching method developed in recent years. Dr. Elizabeth Anne Hunt, an anesthesiologist and critical care physician at Johns Hopkins University, was the first to use this technique to teach cardiopulmonary resuscitation (CPR) skills to pediatric residents [Citation14]. The process involves decomposing a skill into several relatively independent operation steps according to its professional characteristics, such as Step A, B, C and D. In practice, completion of part A is followed by a pause, and the instructor immediately provides short feedback to the trainees to address any shortcomings, and ensure accuracy of step A. The process is then repeated from the beginning; A–B is completed accurately, followed by another pause. The instructor provides feedback, and repeats until A–B–C and A–B–C–D are completed [Citation15]. RCDP is a student-centered, simulated teaching strategy that identifies the needs of residents and provides immediate feedback to improve individual or team performance.
RCDP encompasses the decomposition of teaching objectives, gradually increasing learning difficulty, direct teaching feedback, and the creation of a safe psychological environment. Currently, RCDP has been applied to simulation teaching of first aid skills for adults and children, including CPR, airway management, trauma first aid and sepsis treatment, and has achieved favorable immediate teaching effects [Citation16–19]. However, there is limited data supporting the long-term skill retention effect, and there is no specific research regarding the application of RCDP in obstetric skills teaching, particularly forceps midwifery training. This study aims to investigate the effect of applying RCDP in forceps midwifery skills training for G&O residents.
2. Materials and methods
2.1. Trial design
This research employed a randomized controlled simulation study design. Commencing in March 2021, a total of 60 G&O residents, engaged in their second-year standardized residency training at the Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, were purposefully selected for participation. The participants were allocated in a 1:1 ratio to ensure balanced distribution across the groups. Notably, none of the participants possessed prior experience in forceps operations or had undergone forceps-specific training. The assessment of the RCDP group’s efficacy was performed utilizing a comparative framework, evaluating its superiority over the group receiving feedback after simulations. The study obtained written informed consent from all participants, with ethical approval granted by the Ethics Committee of Shengjing Hospital of China Medical University.
2.2. Randomization and blinding
This study was designed as a single-blind trial, where the instructors were informed about the group assignments, while the residents and assessors remained unaware of the group allocations. The residents themselves developed a stratified block randomization sequence using a computer program with varying block sizes. It is noteworthy that the data analysts were solely exposed to the study identification numbers, without access to information about the participants’ actual group assignments or specific tasks performed during the study.
2.3. Intervention
Participants for the obstetrics and gynecology residents’ forceps simulation training were recruited through WeChat. The purpose of the study, centered on enhancing forceps skills through periodic instructor-led training, was explained to volunteers. A survey was administered to collect demographic information such as age, gender, and prior midwifery experience. Inclusion criteria encompassed residents who had not previously undergone midwifery training.
To ensure standardized training quality, all instructors and trained examiners underwent comprehensive and consistent RCDP training before the commencement of the study. This encompassed meticulous quality control measures for teaching methods, operational guidance, and feedback provision.
Prior to hands-on training, participants received a one-hour theoretical instruction on the principles and execution of forceps delivery during vaginal birth. This comprehensive session covered essential knowledge, modifications, contraindications, and fundamental procedural steps. Subsequent knowledge assessment gauged participants’ understanding.
Practical training followed a group-oriented approach. Residents were divided into five sub-groups, each comprising six trainees. During training sessions, one resident assumed the role of the primary operator, while others served as assistants or observers. Rotation of primary operators within the group facilitated practice for all participants, ensuring each individual operated as the primary for a minimum of 10 min, cumulating in over 60 min of group practice time. Post-group exercises, participants underwent assessments. After assessments, residents had the liberty to practice independently at the Clinical Skills Center during their spare time.
2.4. Implementation of training
In the RCDP group, participants adopted the RCDP training approach as detailed in the reference [Citation14]. The comprehensive forceps delivery procedure was segmented into four distinct phases: preparation (A), placement (B), closing (C), and traction (D). Following procedural segmentation, upon completing the initial ‘preparation work before the operation,’ the procedure halted. Instructors provided targeted feedback to participants, reinforcing correct operational segments, identifying deficiencies, and suggesting enhancements. Subsequently, practice resumed from the outset until the culmination of ‘forceps placement’ (A–B), at which point the procedure paused once more for further feedback. This iterative feedback process continued as residents sequentially proceeded through ‘forceps closing’ (C) and ‘traction’ (D) phases. This cycle persisted until participants executed the entire forceps procedure flawlessly (A–B–C–D). This cycle of practice and feedback was then repeated for other residents within the same group.
In the traditional teaching method (TTM) group, a different approach was employed. After residents completed a full iteration of forceps delivery, the instructor provided feedback, reinforcing accurate operational segments while identifying shortcomings and offering suggestions for refinement. Subsequently, residents were granted the opportunity to repeat the complete forceps procedure. The instructor reviewed the procedure with the resident again after a 10-minute interval, during which another resident within the same group executed the procedure in a similar manner as described above.
2.5. Assessment of training effect
Prior to the initiation of skill training, a theoretical knowledge assessment was administered to all residents to gauge their foundational knowledge level. The assessment comprised a study-specific questionnaire, with a maximum achievable score of 100. The assessment aimed to ensure a baseline understanding of forceps-assisted vaginal delivery concepts and techniques among participants.
Subsequent to the culmination of skills training, an evaluation of residents’ performance was conducted using the ‘Checklist for Performance of Simulated Forceps-Assisted Vaginal Delivery’ (Supplementary file). The assessment incorporated a total score of 100, encompassing the following components: preparation (30 points), forceps insertion (24 points), forceps closure (18 points), and fetal traction (28 points).
Two trained examiners, not involved in the instructional feedback process, concurrently assessed participants’ operational execution. Their evaluations were averaged to generate a comprehensive skill operation score for each resident. This approach ensured objective and consistent assessment of participants’ performance.
A follow-up assessment was conducted one year later by the original examiner to ascertain the degree of retention of forceps-assisted delivery skills among the residents. This evaluation aimed to gauge the sustainability of skill acquisition over time and offered insights into the long-term effectiveness of the training methodologies.
2.6. Satisfaction assessment
Following the training sessions, prompt dissemination of online questionnaires was carried out among the residents belonging to both study groups. These questionnaires were designed to be completed anonymously within a single day. The questionnaire encompassed two essential components, both of which were obligatory for participants.
The initial segment involved a Visual Assessment Simulation (VAS) [Citation20], employing a scoring scale ranging from 0 to 100. The purpose of this segment was to gauge the residents’ self-assessed confidence levels in independently performing the operation after undergoing the training.
The second section centered on evaluating participants’ contentment with the training methodologies and course organization. This evaluation utilized the Satisfaction with Simulation Experience (SSE) scale, which was developed by Levitt-Jones et al. in 2011 [Citation21]. This scale comprises 18 items, structured across three dimensions. The assessment was conducted through a 5-point Likert scale encompassing the responses: ‘Strongly disagree,’ ‘disagree,’ ‘not sure,’ ‘agree,’ and ‘strongly agree.’ The total score achievable on this scale ranged between 0 and 90.
Intricately, the SSE scale’s ‘Debriefing and reflection’ subscale comprised nine items, reflecting the value and significance of the debriefing phases. Similarly, the ‘Clinical reasoning’ subscale comprised five items, assessing the potency of simulation training in enhancing clinical thinking abilities. The ‘Clinical learning’ subscale, with four items, gauged the extent to which simulation training contributed to the augmentation of clinical skills [Citation21]. The internal consistency of the SSE scale was assessed through Cronbach’s α in prior studies [Citation21], yielding values of 0.78 for the SSE scale, 0.94 for the Debriefing and reflection subscale, 0.86 for the Clinical reasoning subscale, and 0.85 for the Clinical learning subscale.
2.7. Statistical analysis
Statistical analysis was performed using SPSS 23.0 (IBM SPSS Inc., USA). An independent sample t-test was used for normally distributed continuous variables examined using the Kolmogorov–Smirnov normality test, and the Mann–Whitney U test was used to compare continuous variables exhibiting a skewed distribution. A paired t-test/Mann-Whitney-U were used to evaluate changes in pre- to post-test scores. Count variables were expressed by frequency (%) and Fishers exact probability method was used for comparison between groups. Statistical significance was set at p < .05.
3. Results
3.1. Participant characteristics
All participants enrolled in the study were second-year residents undergoing standardized training. None had prior experience in forceps skills simulation training, ensuring homogeneity across the RCDP and TTM groups. Demographic variables such as age, sex ratio, education, and work background were thoroughly examined, revealing no significant discrepancies, as outlined in .
Table 1. General characteristics of obstetrics and gynecology residents who underwent second-year standardized residency training.
3.2. Comparative analysis of RCDP and TTM groups
Commencing with comparable theoretical knowledge scores (85.00 [range: 83.00–87.00] vs. 85.00 [range: 83.00–87.00], z = 0.57; p = .57), the RCDP and TTM groups diverged post-training. Promptly after training, the RCDP group displayed significantly superior immediate test scores (92.00 [range: 85.00–95.00] vs. 88.00 [range: 84.00–93.00]), z = 3.79; p < .001, refer to . Remarkably, one year later, no substantial skill score disparities existed between the groups (86.00 [range: 85.00–88.00] vs. 85.50 [range: 84.00–88.25]), z = 0.54; p = .59). Nonetheless, the RCDP group exhibited significantly greater decay in performance than the TTM group (5.0 [range: 3.0–8.25) vs. 2.00 [range: 1.00–5.00]), z = 3.49; p < .001), as depicted in .
Figure 1. Distribution of testing scores before and after forceps simulation training of residents in RCDP and TTM groups. RCDP: Rapid Cycle Deliberate Practice; TTM: traditional teaching method.
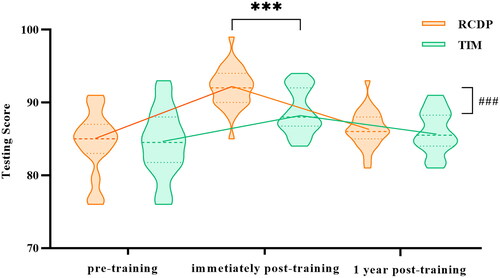
Table 2. The immediate scores after training of two groups. [M (P25, P75)].
3.3. Participant satisfaction
Shifting the focus to participant satisfaction, all surveys were completed with a 100% response rate. Confidence levels in independent operations were comparable between RCDP and TTM groups (80.00 [range: 76.50–84.00]) vs. [80.0 (77.75–84.25)], z = 0.223; p = 8.24), as outlined in . Further examination of Satisfaction with Simulation Experience (SSE) scores revealed significant differences. Particularly, the Debrief and Reflection subscale scores were notably higher in the RCDP group (p < .001), while no substantial differences emerged in the remaining subscales within both groups ().
Table 3. Evaluation distribution of the SSE scales in the RCDP and TTM groups, n(%).
Table 4. SSE scale scores in the RCDP and TTM groups [M (P25, P75)].
4. Discussion
To the best of our knowledge, this is the first educational research study to apply RCDP in obstetric simulation training. This study emphasizes the effectiveness of the RCDP approach in enhancing the immediate proficiency of forceps delivery skills among obstetrics and gynecology residents. Post-training assessments revealed the superior performance of the RCDP group compared to the TTM group. However, the long-term sustainability of these skill improvements through RCDP appears to be limited, as there were no significant differences in forceps operation scores between the two groups one year later. Notably, the ‘Feedback and Reflection’ subscale of the SSE scale underscores the crucial role of effective feedback and thoughtful self-evaluation in enhancing training satisfaction and the overall learning experience. This indicates the significance of constructive feedback and careful self-assessment in optimizing skill acquisition during forceps delivery training.
Due to the instructional characteristics of RCDP, breaking down skill training into distinct segments and providing brief feedback immediately after each segment reduces the learning difficulty of each part [Citation15, Citation22, Citation23]. This single-node deliberate practice and instant teaching feedback encourage residents to execute the correct procedures in the next cycle, address shortcomings, and thus enhance the level of simulated teaching [Citation19]. As a result, RCDP has been proven effective in multiple skill teaching scenarios [Citation14, Citation15, Citation23, Citation24]. This phased structure reduces the cognitive load of each learning session, allowing residents to more effectively internalize the skills [Citation25].
In 2014, Hunt et al. [Citation14] observed that the implementation of RCDP in simulated pediatric CPR complex training significantly shortened the time from pulseless ventricular tachycardia onset to the implementation of compression and defibrillation. Hunt et al. reported in 2017 that in basic life support (BLS) training, RCDP was more effective than traditional BLS courses, exhibiting faster initiation of compressions and higher scores of chest compressions [Citation24]. Other researchers reported that RCDP significantly improved team performance in pediatric advanced life support training courses compared with traditional simulation teaching, as shown by a shorter time to start defibrillation and better team assistance [Citation17, Citation18]. In addition, RCDP significantly improved the technical mastery ability of the trainers when implementing complex training for newborns [Citation19].
When residents within the same midwifery group take on the role of assisting their colleagues ‘in the hot seat,’ this provides them with a mechanism to actively engage and observe as each learner reviews the prescribed procedures. Additionally, instructors can ‘click’ on learners at any time, taking over immediately after a pause (providing feedback). This ensures that all learners, even when not in the ‘hot seat,’ can maintain a high level of engagement at all times. The teacher’s task is to make every effort to ensure that all learners in the group have the opportunity to sit in the ‘hot seat’ and receive rapid-cycle feedback on their performance. Compared to traditional simulation methods, this approach is more effective in fostering teamwork and collaboration [Citation23]. This process exemplifies three key advantages of RCDP: Through repetitive practice with real-time error correction and skill mastery; It enhances learners’ confidence within a safe psychological environment; Skills are broken down into smaller subsets, facilitating optimal learning without imposing a significant cognitive load [Citation26, Citation27].
A notable finding of significance is that both groups of residents expressed satisfaction with the teaching methods, but the RCDP group had a more positive evaluation of the feedback component. For learners participating in forceps delivery simulation training for the first time, this teaching approach improved their satisfaction and confidence, especially for those with limited simulation experience. This further supports the effectiveness of RCDP and its potential to enhance training outcomes across various medical domains.
Interestingly, this study found that while RCDP effectively improved the immediate skills performance of residents, it did not significantly enhance their long-term forceps delivery skills. Despite both groups having opportunities for independent practice, there were no significant differences in forceps delivery performance between the two groups one year later. Further exploration is needed to understand the reasons behind this result. Existing research indicates that RCDP is effective in enhancing short-term memory, but its impact on long-term memory is inconsistent [Citation19, Citation28]. This suggests that while RCDP offers a direct advantage in knowledge application, knowledge retention has yet to be proven. Although the reinforcement of learning skills through repeated immediate feedback is possible, long-term ‘muscle memory’ may not be established through RCDP, and intermittent learning has been shown to aid in the consolidation of long-term memory. For example, studies involving repeated cardiopulmonary resuscitation training every three months using RCDP have demonstrated significant improvements in long-term memory [Citation29].
5. Limitations and future exploration
While this study provides valuable insights into the effectiveness of RCDP in enhancing forceps delivery skills among residents, certain limitations warrant consideration. The scope of group teaching and training duration were constrained by practical factors, including available teaching time and the resident staff size. Moreover, RCDP presents intriguing areas for further investigation: (1) Research Standards for RCDP: The absence of standardized research norms for RCDP raises questions about the observed statistical differences in immediate post-training scores. To ensure the consistency of RCDP topics and research outcomes, establishing common knowledge and curriculum standards is imperative. This step can guide the future application of RCDP in simulation teaching, enhancing its efficacy and impact. (2) Optimizing Long-Term Memory: While RCDP effectively boosts short-term skill levels, its potential to optimize long-term memory warrants exploration. Integrating cognitive psychology and other disciplines could shed light on how RCDP can better foster enduring skill retention. Such insights could underpin advancements in simulation teaching methodologies, contributing to skill retention reform. (3) Determining Effective Retention Period: The choice of a one-year interval for retesting was influenced by training costs and the commencement of subsequent resident cohorts. Although our results underscore the limited long-term retention of skills following RCDP training, future research should investigate the optimal retention duration after RCDP training. This could provide a more comprehensive understanding of skill retention dynamics. (4) Clinical Impact Assessment: Notably, our study solely focused on forceps training through RCDP and did not assess its clinical impact on patient outcomes. While RCDP’s influence on clinical outcomes remains a larger question, our study attempted to mitigate research bias by randomizing residents and standardizing instructor training. Future research endeavors could explore the clinical implications of RCDP in a broader context.
6. Conclusion
In summary, our study finds that RCDP provides immediate benefits, improving proficiency through real-time practice with error correction and enhancing learner confidence in a secure environment. It breaks down complex skills for effective learning. However, for long-term skill retention, additional methods may be needed. Future studies can explore combining RCDP with other methods to enhance skill retention, ultimately benefiting patient care.
Authors contributions
XW, ZS, and DZ designed the study and drafted the manuscript. XC, YZ, and YL and designed the statistical analysis plan. TL has participated the training and reviewed and co-authored the manuscript with DZ. All authors take responsibility for the appropriateness of the content. All authors contributed to the article and approved the submitted version.
Ethical approval
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Ethics Committee of Shengjing Hospital of China Medical University (No. 2021PS744K, Date.07/10/2021).
Supplemental Material
Download Zip (24.9 KB)Acknowledgements
We would like to express our gratitude to all those who helped us during the writing of this manuscript. Thanks to Graduate Medical Training Department and Clinical Skills Center in Shengjing Hospital for providing data resources. Thanks to all the peer reviewers for their opinions and suggestions.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Holdt Somer SJ, Sinkey RG, Bryant AS. Epidemiology of racial/ethnic disparities in severe maternal morbidity and mortality. Semin Perinatol. 2017;41(5):1–9. doi: 10.1053/j.semperi.2017.04.001.
- Pergialiotis V, Bellos I, Antsaklis A, et al. Maternal and neonatal outcomes following a prolonged second stage of labor: a meta-analysis of observational studies. Eur J Obstet Gynecol Reprod Biol. 2020;252:62–69. doi: 10.1016/j.ejogrb.2020.06.018.
- Dildy GA, Belfort MA, Clark SL. Obstetric forceps: a species on the brink of extinction. Obstet Gynecol. 2016;128(3):436–439. doi: 10.1097/AOG.0000000000001557.
- Patel RR, Murphy DJ. Forceps delivery in modern obstetric practice. BMJ. 2004;328(7451):1302–1305. doi: 10.1136/bmj.328.7451.1302.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2013. National vital statistics reports: from the centers for disease control and prevention, national center for health statistics. Natl Vital Stat Rep. 2015;64(1):1–65.
- Yubo Zhou HL, Liping Z. Secular trends of operative vaginal delivery in Southern and Northern China during 1993 -2010. Nat Med J China. 2014;94:3599–3602.
- Bin Wang QS, Wang Y, Li N, et al. National survey on midwifery practice in health facilities in China. Chin J Obstet Gynecol. 2007;42:305–308.
- Lei Hou GL, Zou L, Li C, et al. Cesarean delivery rate and indications in mainland China: a cross sectional study in 2011. Chin J Obstet Gynecol. 2014;49:728–735.
- Sng LS, Yip WH, Hong SYC, et al. Comparison of postpartum incontinence outcomes after vacuum-assisted and forceps-assisted deliveries in a tertiary maternity unit. Int Urogynecol J. 2022;33(6):1529–1537. doi: 10.1007/s00192-021-04952-2.
- ACOG Practice Bulletin No. 154: operative vaginal delivery. Obstet Gynecol. 2015;126:e56–e65.
- Gossett DR, Gilchrist-Scott D, Wayne DB, et al. Simulation training for forceps-assisted vaginal delivery and rates of maternal perineal trauma. Obstet Gynecol. 2016;128(3):429–435. doi: 10.1097/AOG.0000000000001533.
- Rose K, Jensen K, Guo R, et al. Simulation to improve trainee skill and comfort with forceps-assisted vaginal deliveries. AJP Rep. 2019;9(1):e6–e9. doi: 10.1055/s-0039-1677736.
- Sano Y, Hirai C, Makino S, et al. Incidence and risk factors of severe lacerations during forceps delivery in a single teaching hospital where simulation training is held annually. J Obstet Gynaecol Res. 2018;44(4):708–716. doi: 10.1111/jog.13558.
- Hunt EA, Duval-Arnould JM, Nelson-McMillan KL, et al. Pediatric resident resuscitation skills improve after “rapid cycle deliberate practice” training. Resuscitation. 2014;85(7):945–951. doi: 10.1016/j.resuscitation.2014.02.025.
- Taras J, Everett T. Rapid cycle deliberate practice in medical education – a systematic review. Cureus. 2017;9(4):e1180. doi: 10.7759/cureus.1180.
- Lemke DS, Fielder EK, Hsu DC, et al. Improved team performance during pediatric resuscitations after rapid cycle deliberate practice compared with traditional debriefing: a pilot study. Pediatr Emerg Care. 2019;35(7):480–486. doi: 10.1097/PEC.0000000000000940.
- Gross IT, Abrahan DG, Kumar A, et al. Rapid cycle deliberate practice (RCDP) as a method to improve airway management skills – A randomized controlled simulation study. Cureus. 2019;11(9):e5546. doi: 10.7759/cureus.5546.
- Lemke DS, Young AL, Won SK, et al. Rapid-cycle deliberate practice improves time to defibrillation and reduces workload: a randomized controlled trial of simulation-based education. AEM Educ Train. 2021;5(4):e10702. doi: 10.1002/aet2.10702.
- Magee MJ, Farkouh-Karoleski C, Rosen TS. Improvement of immediate performance in neonatal resuscitation through rapid cycle deliberate practice training. J Grad Med Educ. 2018;10(2):192–197. doi: 10.4300/JGME-D-17-00467.1.
- Vousden N, Hamakarim Z, Briley A, et al. Assessment of a full dilatation cesarean delivery simulator. Obstet Gynecol. 2015;125(2):369–374. doi: 10.1097/AOG.0000000000000622.
- Levett-Jones T, McCoy M, Lapkin S, et al. The development and psychometric testing of the satisfaction with simulation experience scale. Nurse Educ Today. 2011;31(7):705–710. doi: 10.1016/j.nedt.2011.01.004.
- Issenberg SB, McGaghie WC, Petrusa ER, et al. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924.
- Chancey RJ, Sampayo EM, Lemke DS, et al. Learners’ experiences during rapid cycle deliberate practice simulations: a qualitative analysis. Simul Healthc. 2019;14(1):18–28. doi: 10.1097/SIH.0000000000000324.
- Hunt EA, Duval-Arnould JM, Chime NO, et al. Integration of in-hospital cardiac arrest contextual curriculum into a basic life support course: a randomized, controlled simulation study. Resuscitation. 2017;114:127–132. doi: 10.1016/j.resuscitation.2017.03.014.
- Mancinetti M, Guttormsen S, Berendonk C. Cognitive load in internal medicine: what every clinical teacher should know about cognitive load theory. Eur J Intern Med. 2019;60:4–8. doi: 10.1016/j.ejim.2018.08.013.
- Roszczynialski KN, Register SJ, Bergman L, et al. An investigation on the perceptions of practicing interdisciplinary health professionals on rapid cycle deliberate practice simulation. Simul Healthc. 2022;17(1):e14–e19. doi: 10.1097/SIH.0000000000000577.
- Zapko KA, Ferranto MLG, Blasiman R, et al. Evaluating best educational practices, student satisfaction, and self-confidence in simulation: a descriptive study. Nurse Educ Today. 2018;60:28–34. doi: 10.1016/j.nedt.2017.09.006.
- Swinger N, Hocutt G, Medsker BH, et al. Rapid cycle deliberate practice versus traditional simulation for training extracorporeal membrane oxygenation specialists in circuit air emergency management: a randomized trial. Simul Healthc. 2022;17(1):e28–e37. doi: 10.1097/SIH.0000000000000562.
- Sullivan NJ, Duval-Arnould J, Twilley M, et al. Simulation exercise to improve retention of cardiopulmonary resuscitation priorities for in-hospital cardiac arrests: a randomized controlled trial. Resuscitation. 2015;86:6–13. doi: 10.1016/j.resuscitation.2014.10.021.
