Abstract
Background. We hypothesized that indices of angiogenesis (vascular endothelial growth factor (VEGF), angiopoietins (Ang‐1 and ‐2), platelet activation (soluble P‐selectin)) and endothelial damage/dysfunction (von Willebrand factor (vWf)) would be more deranged in South Asians than in white Europeans when measured within the coronary sinus or coronary artery per se (that is, intracardiac sampling of blood supplying and draining the heart), as compared to measurements from the peripheral venous system.
Methods. To test this hypothesis, we performed a cross‐sectional study of 87 subjects undergoing cardiac catheterization, where 43 were South Asian and 44 were white European.
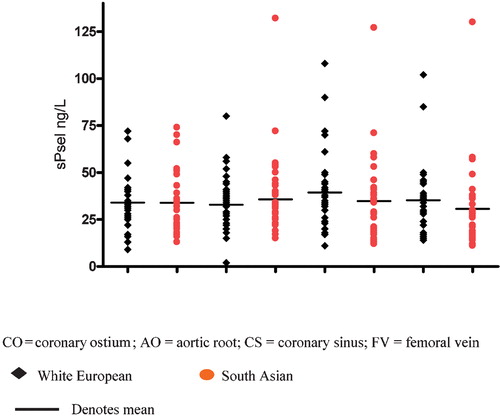
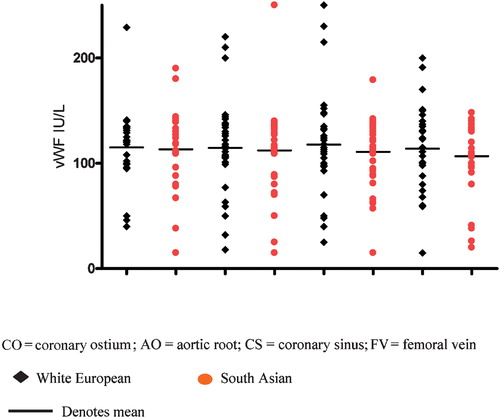
Results. South Asian participants were younger (P = 0.01) but had a lower rate of self‐reported smoking (P = 0.01). The extent of coronary atherosclerosis, assessed using presence of lesions>50%, number of vessels diseased and Gensini score, was comparable between the two ethnic groups (all P = NS). When samples were analysed from the coronary circulation or the femoral vein in relation to South Asian and white European ethnicity, there were no significant differences in the levels of VEGF, angiopoietins 1 and 2, soluble P‐selectin and vWf levels between the two ethnic groups.
Conclusion. Indices of angiogenesis, platelet activation, and endothelial damage/dysfunction are comparable in South Asians and their white European counterparts. Our results suggest that their pathophysiological roles may be comparable in South Asians and white Europeans in the context of coronary artery disease.
Introduction
In the assessment of individual patient cardiovascular (CV) risk, age, sex and body mass index, hypertension, diabetes, smoking, lipid profile, and family history of premature coronary disease are important Citation1, Citation2. Whilst these scoring systems allow population‐based risk calculations, they seem limited in providing a comprehensive risk profile, particularly in South Asians Citation3–6. Previous studies have suggested that this ethnic group is more likely to present acutely with coronary events and have a higher associated mortality at an earlier age Citation7, Citation8.
Underlying pathophysiological abnormalities such as insulin resistance are more prevalent in South Asians and may account for some of the excess CV risk Citation9, Citation10. However, increasing evidence point to a ‘deranged’ balance of haemostatic, endothelial, and inflammatory factors, which are linked to atherosclerosis in South Asians Citation11–14. Features of enhanced cytokine response Citation15 and impaired endothelium function Citation16 are already known to be present in South Asians compared to white Europeans. Recently, our group has demonstrated abnormal circulating adipokines in South Asians, correlating with coronary artery disease severity at angiography Citation17. However, dependent on their circulating kinetics and responsiveness, peripheral assays of these markers may be less sensitive or specific for coronary disease due to a combination of dilution effects and variable relevance in individual subjects.
We hypothesized that indices of angiogenesis (vascular endothelial growth factor (VEGF), angiopoietins (Ang‐1 and ‐2), platelet activation (soluble P‐selectin)) and endothelial damage/dysfunction (von Willebrand factor (vWf)) would be more deranged in South Asians than in white Europeans when measured within the coronary sinus or coronary artery per se (that is, intracardiac sampling of blood supplying and draining the heart), as compared to measurements from the peripheral venous system. To test this hypothesis, we performed a cross‐sectional study of subjects undergoing cardiac catheterization.
Key messages
Abnormal angiogenesis, platelet activation, and endothelial damage/dysfunction are involved in the pathogenesis of atherosclerotic vascular disease.
This study shows that indices of angiogenesis, platelet activation, and endothelial damage/dysfunction are comparable in South Asians and their white European counterparts.
Our results suggest that their pathophysiological roles of angiogenesis, platelet activation, and endothelial damage/dysfunction may be comparable in South Asians and white Europeans in the context of coronary artery disease.
Methods
We completed a cross‐sectional study comparing indices of angiogenesis, thrombosis, endothelial damage/dysfunction, and inflammation in blood samples derived from a range of coronary and peripheral vascular sites. Comparisons were made of blood levels (analyses blinded to sample site and ethnicity) in stable patients undergoing diagnostic cardiac catheterization for the assessment of coronary artery disease (CAD). Data pertaining to ethnic origin were obtained using patients' self‐reported ethnic group on hospital admission. A similar search strategy to identify ethnic groups has been used previously Citation18. Of our 87 patients undergoing cardiac catheterization, 43 were South Asian and 44 were white European (Table ), and none were of mixed race.
Table I. Baseline clinical characteristics in study cohorts.
Exclusion criteria were as follows: atrial fibrillation; significant valvular heart disease; previous coronary artery bypass surgery; primary angioplasty for acute ST elevation myocardial infarction; infection or pyrexial illness; recent (<3 months) ischaemic stroke; chronic and systemic illnesses including renal failure (on supportive therapy), hepatic impairment, cancer, and inflammatory connective tissue disease; inflammatory bowel disease; any oral steroid intake; and/or hormone replacement therapy. The local ethics committee approved the study, and all subjects gave informed written consent before taking part.
Sampling technique
Central access was gained by introducing 5 and 6 French sheaths (Cordis Ltd, New Jersey, USA) in the femoral vein and artery. A 6 French Judkins catheter (Cordis Ltd, New Jersey, USA) was used to cannulate the coronary ostium and a pigtail catheter positioned in the aortic root. Both aortic root and coronary ostium samples were sampled, as it is unclear in the published literature as to the importance of coronary arterial versus aortic root samples—both sites are anatomically close, but the predominant flow patterns are markedly different (diastolic versus systolic flow). In this study, an Amplatz AL‐1 catheter (Cordis Ltd, New Jersey, USA) or a modified Sims catheter (Cook Ltd, Letchworth, UK) was used to cannulate the coronary sinus. All catheters and sheaths were flushed with a solution of 0.5% heparinized normal saline (0.9% sodium chloride). The positions of all catheters were verified using fluoroscopy and anterograde or retrograde angiography as appropriate. The extent of CAD was estimated using calculated Gensini scores Citation19 with an obstructive lesion defined as luminal stenosis of >50% on two orthogonal views at angiography.
The first 10 mL of blood drawn at each anatomical site was discarded. With each test sample, 6 mL of blood was collected into two tubes (3 mL) containing sodium citrate (3.2% Buffered Sodium Citrate, Vacuette, Greiner Bio‐one, Bad Haller, Austria). Samples were acquired from the coronary ostium, the aortic root, the coronary sinus, and, finally, the femoral vein, where relevant. All tubes were stored in melting ice, then plasma was prepared by centrifugation at 3,000 rpm (1,000 g) for 20 min at 4°C. All aliquots were stored at −70°C to allow batch analysis of research indices.
Laboratory methods
Vascular endothelial growth factor (VEGF), angiopoietins 1 and 2, soluble P‐selectin (sP‐sel) levels were measured in duplicate by enzyme‐linked immunosorbent assays (ELISA) (R&D Systems, Abingdon, Oxfordshire, United Kingdom) with von Willebrand factor (vWf) levels using commercial reagents (Dako‐Patts, Ely, United Kingdom). Complete description of the assays for VEGF, angiopoietin 1 and angiopoietin 2 can be found elsewhere (20–22). The inter‐ and intra‐assay coefficients of variation for all ELISA assays were <5% and <10% respectively.
Power calculations
As there are no published data using coronary sinus, ostium, and aortic root between the two ethnic groups, we based our calculation on studies using peripheral indices between the two ethnic groups with cardiovascular disease Citation23, hypothesizing a difference in biomarker levels of at least half a standard deviation of data or log10‐transformed data. In order to achieve this, we calculate a minimum sample of 23 subjects for a P<0.05 and 1‐β = 0.80.
Statistical analyses
Following application of the Komolgorov‐Smirnov test to determine variable distribution, non‐categorical data distributed normally were expressed as mean (standard deviation) and data distributed non‐normally (for instance, VEGF, angiopoietin 1 and 2) were expressed as median (interquartile range). Friedman two‐way repeated measures analysis of variance (RMANOVA) was used to evaluate the difference between sample sites within subjects with subsequent post hoc analysis of difference using Bonferroni correction. Categorical data (sex and gender) were analysed by the chi‐square test, and continuous data between the two ethnic groups were analysed using unpaired Student t‐test. A probability, P, of less than 0.05 was considered as statistically significant. Analyses and power calculations were done using SPSS Version 12.0 (SPSS Inc., Chicago, USA).
Results
South Asians participants were younger (P = 0.01) but had a lower rate of self‐reported smoking (P = 0.01) (Table ). The extent of coronary atherosclerosis, assessed using presence of lesions>50%, number of vessels diseased, and Gensini score, was comparable between the two ethnic groups (all P = NS). Of the whole cohort, 33 white Europeans and 34 South Asians had angiographic evidence of significant coronary artery disease (Table ).
Table II. Clinical characteristics of two ethnic groups with coronary artery disease.
When samples were analysed from the coronary circulation or the femoral vein in relation to South Asian and white European ethnicity, there were no significant differences in the levels of VEGF, angiopoietins 1 and 2, soluble P‐selectin, and vWf levels (Table ).
Table III. Analysis of VEGF, angiopoietins 1 and 2 levels sampled at different sites in the whole cohort.
Discussion
To our knowledge, this is the first study to compare indices of angiogenesis, thrombogenesis, and endothelial function between South Asians and white Europeans using coronary arterial, aortic root, and coronary sinus blood assays. The main findings were that these ‘biomarkers’ of vascular disease were comparable between the two ethnic groups at each site, irrespective of the presence of atheroma on angiography.
Our baseline demographic data remain consistent with previous studies, showing that South Asians undergoing assessment for chest pain are more likely to be younger, with a lower rate of smoking. Whilst debate about possible ethnic difference in the extent of angiographic coronary disease exists, no such disparity was seen in our cohort using presence of lesions>50%, number of vessels diseased, and Gensini score. Various studies have demonstrated evidence of a ‘deranged’ balance of haemostatic, endothelial, and inflammatory processes linked with atherosclerosis in South Asians. All of the studies involved used peripheral venous samples. We found no such difference between South Asians and white Europeans in measurement of VEGF, angiopoietin 1 and 2, soluble P‐selectin, and vWf from peripheral and intracardiac sources.
Overall, this cross‐sectional study is limited by point estimates of dynamic biomarkers at pre‐specified time points and sites. Furthermore, the observations are limited to participants without evidence of on‐going acute ischaemia, though, overall, participants are reflective of ‘real‐life’ patients in day‐to‐day practice. Though regional sampling was used, we may not be able to detect signals of the perivascular or intramyocytic levels of these mediators. Alternatively, the signals may be generated on a shorter or longer timescale than can be accommodated in an acute invasive protocol such as employed here. Also, ‘atherosclerotic plaque load’ may be different between the left and right coronary artery systems, and the dominance of the coronary arteries may also be different for different patients; furthermore, the coronary sinus is not the sole venous drainage of the heart, making detailed study of intracoronary gradients difficult to interpret in this relatively small study. Finally, such exploratory analysis may not explain the complex interrelationships of these biomarkers, including the effect(s) of associated comorbidities, if any.
In conclusion, we have shown that indices of angiogenesis, platelet activation and endothelial damage/dysfunction are comparable in South Asians and their white European counterparts. Our results suggest that their roles may be comparable in South Asians and white Europeans in the context of coronary artery disease.
Acknowledgements
We acknowledge the support of our patients and the staff of our catheterization laboratory in the completion of this work. The study was funded by grants from the Peel Medical Research Trust and Sandwell and West Birmingham Hospitals NHS Trust Research and Development programme for the Haemostasis, Thrombosis and Vascular Biology Unit.
References
- Anderson K. M., Odell P. M., Wilson P. W. F., Kannel W. B. Cardiovascular disease risk profiles. Am Heart J 1991; 121: 293–8
- The Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation 2002; 106: 3143–421
- Khot U. N., Khot M. B., Bajzer C. T., Sapp S. K., Ohman E. M., Brener S. J., et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA 2003; 290: 898–904
- Lip G. Y., Barnett A. H., Bradbury A., Cappuccio F. P., Gill P. S., Hughes E., et al. Ethnicity and cardiovascular disease prevention in the United Kingdom: a practical approach to management. J Hum Hypertens 2007; 21: 183–211
- Cappuccio F. P., Oakeshott P., Strazzullo P., Kerry S. M. Application of Framingham risk estimates to ethnic minorities in United Kingdom and implications for primary prevention of heart disease in general practice: cross sectional population based study. BMJ 2002; 325: 1271–85
- Bhopal R., Fischbacher C., Vartiainen E., Unwin N., White M., Alberti G. Predicted and observed cardiovascular disease in South Asians: application of FINRISK, Framingham and SCORE models to Newcastle Heart Project data. J Public Health (Oxf) 2005; 27: 93–100
- British Heart Foundation Statistics Database. Coronary Heart Disease Statistics. 2002. Available at: http://www.bhf.org.uk/professionals/uploaded/bhf%20heartstats%202003%20‐%204‐page.pdf (accessed April 21, 2005)
- Tunstall‐Pedoe H., Kuulasmaa K., Mahonen M., Tolonen H., Ruokokoski E., Amouyel P. Contribution of trends in survival and coronary‐event rates to changes in coronary heart disease mortality: 10‐year results from 37 WHO MONICA project populations. Monitoring Trends and Determinants in Cardiovascular Disease. Lancet 1999; 353: 1547–57
- McKeigue P. M., Shah B., Marmot M. G. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991; 337: 382–6
- Misra A., Vikram N. K. Insulin resistance syndrome (metabolic syndrome) and obesity in Asian Indians: evidence and implications. Nutrition 2004; 20: 482–91
- Whincup P. H., Gilg J. A., Papacosta O., Seymour C., Miller G. J., Alberti K. G., et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ 2002; 324: 635–42
- Kain K., Catto A. J., Grant P. J. Impaired fibrinolysis and increased fibrinogen levels in South Asian subjects. Atherosclerosis 2001; 156: 457–61
- Hughes K., Aw T. C., Kuperan P., Choo M. Central obesity, insulin resistance, syndrome X, lipoprotein(a), and cardiovascular risk in Indians, Malays, and Chinese in Singapore. J Epidemiol Community Health 1997; 51: 394–9
- Kain K., Catto A. J., Young J., Bamford J., Bavington J., Grant P. J. Insulin resistance and elevated levels of tissue plasminogen activator in first‐degree relatives of South Asian patients with ischemic cerebrovascular disease. Stroke 2001; 32: 1069–73
- Yudkin J. S., Yajnik C. S., Mohamed‐Ali V., Bulmer K. High levels of circulating proinflammatory cytokines and leptin in urban, but not rural, Indians. A potential explanation for increased risk of diabetes and coronary heart disease. Diabetes Care 1999; 22: 363–4
- Chambers J. C., McGregor A., Jean‐Marie J., Kooner J. S. Abnormalities of vascular endothelial function may contribute to increased coronary heart disease risk in UK Indian Asians. Heart 1999; 81: 501–4
- Lim H. S., Tayebjee M. H., Tan K. T., Patel J. V., Macfadyen R. J., Lip G. Y. Serum adiponectin in coronary heart disease: ethnic differences and relation to coronary artery disease severity. Heart 2005; 91: 1605–6
- Bhopal R. Race and ethnicity: responsible use from epidemiological and public health perspectives. J Law Med Ethics 2006; 34: 500–7; 479
- American Heart Association Committee Report: A reporting system on patients evaluated for coronary artery disease. Circulation. 51. 7
- Chin B. S., Chung N. A., Gibbs C. R., Blann A. D., Lip G. Y. H. Vascular endothelial growth factor and soluble P‐selectin in acute and chronic congestive heart failure. Am J Cardiol 2002; 90: 1258–60
- Caine G. J., Blann A. D., Stonelake P. S., Ryan P., Lip G. Y. H. Plasma angiopoietin‐1, angiopoietin‐2 and tie‐2 in breast and prostate cancer: a comparison with VEGF and Flt‐1. Eur J Clin Invest 2003; 33: 883–90
- Chong A. Y., Caine G. J., Freestone B., Blann A. D., Lip G. Y. Plasma angiopoietin‐1, angiopoietin‐2, and angiopoietin receptor tie‐2 levels in congestive heart failure. J Am Coll Cardiol 2004; 43: 423–8
- Blann A. D., Belgore F. M., McCollum C. N., Lip G. Y. H. Vascular endothelial growth factor and its receptor, Flt‐1, in the plasma of patients with coronary or peripheral atherosclerosis, or Type II diabetes. Clin Sci 2002; 102: 187–94