Abstract
Background. Failure to decrease blood pressure (BP) normally during night‐time, which is called non‐dipping, in hypertensive individuals is associated with higher cardiovascular morbidity and mortality. In addition, non‐dipping BP leads to structural changes in the left ventricle; however, the effect of non‐dipping BP on coronary flow reserve (CFR) has not been studied yet. Methods. In this study, we measured CFR of 22 subjects with non‐dipper hypertension, and 15 subjects with dipper hypertension using transthoracic second‐harmonic Doppler echocardiography (Acuson Sequoia C256®). None of the subjects had any systemic disease or coronary risk factor except hypertension. Results. Age, gender, body mass index, lipids and echocardiographic findings including left ventricular mass index were similar between the groups. Office BP recordings were similar between non‐dipper and dipper groups (147.9±6.1/93.9±4.3 vs 144.0±8.0/93.0±3.7). Daytime and 24‐h ambulatory BP measurements were similar within the groups, but night‐time BPs were significantly greater in non‐dipper group than those were in dipper group. Left ventricular diastolic and systolic functions, and both baseline and hyperemic peak diastolic coronary velocity as well as CFR, were similar between the non‐dipper and dipper groups (CFR: 2.47±0.59 vs 2.39±0.47). Conclusion. CFR were similar in patients with non‐dipper and dipper hypertension in the absence of excessive left ventricular hypertrophy and other cardiovascular risk factors.
Introduction
Decreased coronary vasodilator reserve suggesting microvascular dysfunction may exist in the majority of patients with essential hypertension, and might be responsible for ischemic symptoms in these patients, though their epicardial coronary arteries are angiographically normal Citation[1]. The mechanism involved in microvascular dysfunction leading to myocardial ischemia and angina in patients with hypertension without coronary artery disease (CAD) is not clear yet. Left ventricular hypertrophy (LVH) resulting from elevated blood pressure (BP) is a well‐known factor responsible for impairment of coronary vasodilator capacity Citation[2–4]. However, angina and impairment of coronary vasodilating capacity may occur in some hypertensive individuals in the absence of LVH Citation[5], Citation[6]. Furthermore, abnormalities in coronary reactivity may also exist in asymptomatic hypertensive individuals Citation[1], Citation[2].
Hypertensive as well as normotensive individuals are divided into dippers and non‐dippers, according to night‐time reduction in BP⩾ or <10%, respectively Citation[7]. Recent studies have shown that not only LVH Citation[8], Citation[9] but also the risk of cardiovascular (CV) mortality Citation[10], Citation[11], silent cerebrovascular disease Citation[12] and progression of nephropathy Citation[13] were greater in subjects with non‐dipping BP than in those with dipping BP.
So far, the mechanisms that may be involved in the alteration of coronary flow reserve (CFR) in hypertension have not been extensively studied in humans because of the complex and invasive techniques used to evaluate CFR. Transthoracic second‐harmonic Doppler echocardiography (TTDE), which has been evolved recently, is capable of measuring coronary blood flow velocity in the middle to distal portion of left anterior descending coronary artery (LAD). Pharmacological stress TTDE is currently a useful and highly reproducible tool in evaluating CFR, and in several studies, its feasibility has been validated Citation[14], Citation[15]. Furthermore, in a recent study, it has been shown that CFR measured by TTDE has an excellent correlation with CFR measured by positron emission tomography, which has been validated as a gold standard for CFR measurement Citation[16].
Although substantial evidence supports the contention that night‐time BP is more important than daytime BP in predicting outcome and developing end‐organ damage, particularly in individuals who have night time BP fall <10% (non‐dipping); to date, there is no study investigating CFR and coronary microvascular function in these patients. In this study, we aimed to evaluate CFR in newly diagnosed and never‐treated essential hypertensive subjects with dipping and non‐dipping BP without excessive LVH and/or coronary risk factors using TTDE.
Methods
Study population
The overall study population consisted of 37 subjects: 22 subjects with non‐dipper hypertension (group I) and 15 patients with dipper hypertension (group II). Their demographic and clinical data are shown in Table . Inclusion criteria were 18–55 years of age, and for women to be on a regular menstrual cycle. Exclusion criteria were having any systemic disease such as hemolytic, hepatic and renal diseases or any disease that could cause CFR impairment (e.g. diabetes mellitus or impaired oral glucose tolerance test), family history of CAD in first‐degree male relatives younger than 55 years and in first‐degree female relatives younger than 65 years, and alcohol use. Subjects using any vasoactive drug, those who took previous anti‐hypertensive therapy, current smokers, and those who had ST segment or T wave changes specific for myocardial ischemia, Q waves and incidental left bundle branch block on ECG were excluded from the study. Also excluded were individuals with total cholesterol levels greater than 240 mg/dl, high‐density lipoprotein (HDL) cholesterol levels less than 30 mg/dl, LDL cholesterol levels greater than 160 mg/dl, triglyceride levels greater than 240 mg/dl, and those with elevated liver enzymes, body mass index (BMI) greater than 30 kg/m2, excessive LVH (LVMI equal or greater than 125 g/m2 for men and 110 g/m2 for women). Written informed consent was obtained from each subject, and the institutional ethics committee approved the study protocol.
Table I. Demographic and biochemical characteristics and office blood pressure measurements were similar between the groups.
BP measurement and ambulatory BP monitoring (ABPM)
BP was measured using a mercury sphygmomanometer in office setting; first and fifth phases of Korotkoff sounds were used for systolic and diastolic BP. Non‐invasive 24‐h ABPM were performed with a portable compact digital recorder (Spacelabs Medical Inc., Model 92512, Redmond, VA, USA), and analyzed using customized analytical software (Spacelabs Medical Inc., Model 90207). Appropriate cuff sizes were chosen for each subject. All subjects wore an ABPM device for a single 24‐h period. The device was programmed to inflate and record BP at pre‐specified intervals (every 15 min during daytime hours and every 30 min during night‐time hours), which provided approximately 80 BP recordings during the 24‐h period. The display of ABPM was deactivated so that viewing each BP reading did not distract subjects.
Reports generated from a session of ABPM contained BP recordings for the entire 24 h, heart rate, mean arterial pressure and BP load as well as summary statistics for the overall 24‐h, daytime and night‐time period. If at least 80% of the total BP readings were valid, the ABPM record was considered satisfactory and used for further analyses.
Diagnosis of hypertension
In each subject, BP was measured on three separate days after 15 min of comfortable sitting and averaged. Then each subject undertook 24 h ABPM. Individuals who had systolic BP⩾140 mmHg and/or a diastolic BP⩾90 mmHg in office setting, and in ABPM, an average 24‐h systolic BP>130 mmHg and/or diastolic BP>80 mmHg, an average daytime systolic BP>135 mmHg and/or diastolic BP>85 mmHg or an average night‐time systolic BP>125 mmHg and/or diastolic BP>75 mmHg were diagnosed as hypertensive.
Echocardiographic examination
Each subject was examined using an Acuson Sequoia C256® Echocardiography System equipped with 3V2c and 5V2c broadband transducers with second‐harmonic capability (Acuson Corp, Mountain View, CA, USA). Two‐dimensional, M‐mode and subsequent transthoracic tissue Doppler and Doppler harmonic echocardiography examination were performed on each subject.
Left ventricular mass determination
Left ventricular mass (LVM) was calculated from M‐mode records taken on parasternal long‐axis images according to the formula below Citation[17], and left ventricular mass index (LVMI) was expressed as LVM per square meter of body surface area.
CFR measurement
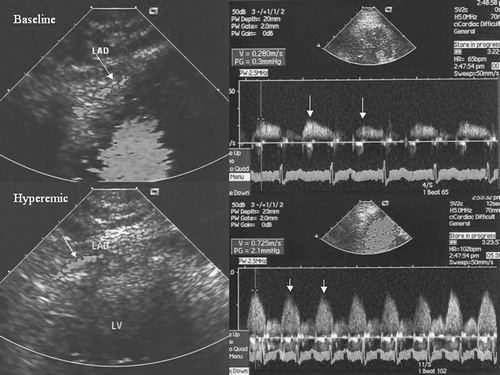
Visualization of the distal LAD was performed using a modified, foreshortened, two‐chamber view obtained by sliding the transducer on the upper part and medially from an apical two‐chamber view to reach the best alignment to the interventricular sulcus. Subsequently, coronary flow in the distal LAD was examined by color Doppler flow mapping over the epicardial part of the anterior wall, with the color Doppler velocity range of 8.9–24.0 cm/s (Figure ). The color gain was adjusted to provide optimal images. The acoustic window was around the midclavicular line, in the fourth and fifth intercostal spaces, with the subject in the left lateral decubitus position Citation[18]. The left ventricle was imaged on the long‐axis cross‐section, and the ultrasound beam was then inclined laterally. Next, coronary blood flow in the LAD (middle to distal) was searched by color Doppler flow mapping. All subjects had Doppler recordings of the LAD with a dipyridamole infusion at a rate of 0.56 mg/kg over 4 min. All subjects had continuous heart rate and electrocardiographic monitoring as well as BP recording at baseline, during dipyridamole infusion and at recovery. Echocardiographic images were recorded on VHS videotapes. Two experienced echocardiographers who had been blinded to the clinical data analyzed the recordings. By placing the sample volume on the color signal, spectral Doppler of the LAD showed the characteristic biphasic flow pattern with larger diastolic and smaller systolic components. Coronary diastolic peak velocities were measured at baseline and after dipyridamole (0.56 mg/kg over 4 min) by averaging the highest three Doppler signals for each measurement. CFR was defined as the ratio of hyperemic to baseline diastolic peak velocities (Figure ). CFR⩾2.0 was considered normal Citation[18].
Statistical analyses
All analyses were carried out using SPSS 9.0 (SPSS for Windows 9.0, Chicago, IL, USA). All group data are expressed as mean±standard deviation. The two groups were compared using the Mann–Whitney U test for multiple comparisons, because of small sample size of the groups. The chi‐square statistics was used to assess differences between categorical variables. Spearman's correlation analysis was used to test the associations between coronary flow measurements and other studied variables. Linear regression analysis was used to determine the independent predictors for CFR. A p‐value less than 0.05 was considered significant.
Results
Clinical characteristics of the study population
The general characteristics and risk factors for CAD of the study population are presented in Table . Age, gender, BMI, baseline heart rate, lipid profiles and fasting glucose levels as well as high‐sensitivity C‐reactive protein (hsCRP) and hemoglobin were similar within the non‐dipper and dipper groups. Systolic and diastolic BP in office setting was similar between dipper and non‐dipper hypertensive subjects.
ABPM analysis
By definition, average daytime systolic, diastolic and mean BP were not different between non‐dippers and dippers. In contrast, average night‐time systolic, diastolic and mean BP were significantly higher in the non‐dipper hypertension group than in the dipper group (Table ).
Table II. Data from ABPM of the study subjects. Mean daytime ABPM measurements were similar in non‐dipping and dipping hypertension groups; however, in patients with non‐dipping hypertension night‐time ABPM measurements were higher than those in the dipper ones.
Analyses of the echocardiographic measurements
Interventricular septum (IVS) thickness, left ventricle posterior wall (PW) thickness, left ventricular end diastolic diameter (LVDD), left ventricular systolic diameter (LVSD), left ventricular ejection fraction (EF), LVMI and left ventricular diastolic parameters were similar between non‐dipper and dipper hypertension groups (Table ).
Table III. Data from echocardiographic examinations including left ventricular mass index and diastolic function parameters of the study subjects.
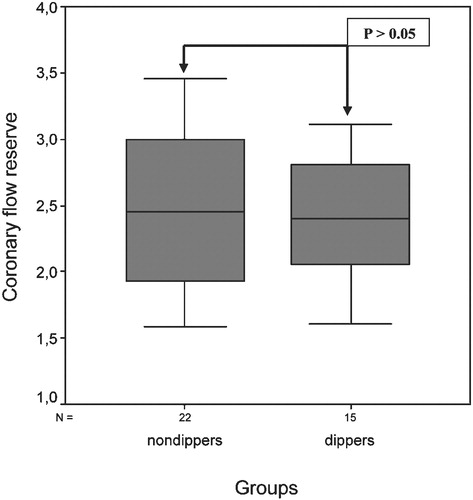
Analysis of CFR measurements
Baseline and peak heart rate and BPs were similar between the two groups. Both baseline and hyperemic diastolic peak flow velocity of LAD (DPFV) were similar between the non‐dipper and the dipper groups (Table ). Accordingly, CFR was similar between the two groups (Figure ).
Correlation analyses
Table shows the correlations between CFR and study variables. CFR was significantly and directly correlated with mitral E velocity and mitral E/A ratio. In addition, CFR was also weakly correlated with hsCRP, mitral A velocity and E deceleration time, but these correlations did not reach statistical significance.
Table IV. Correlations of coronary flow reserve with the study variables. Coronary flow reserve significantly correlated with mitral E velocity and mitral E/A ratio.
In stepwise multiple linear regression analysis, we found that CFR was independently correlated with left atrium diameter (β = −0.313, p = 0.01), mitral E wave deceleration time (β = −0.443, p = 0.003) and mitral E/A ratio (β = 0.288, p = 0.03).
Discussion
In the present study, we aimed to evaluate CFR and coronary microvascular functions in subjects with non‐dipper hypertension, whose BP did not decrease enough during the night, and in patients with dipper hypertension using TTDE. We found that non‐dipper hypertensive patients showed CFR and microvascular functions as well as measure of early and late diastolic peak flow velocity ratio and E wave deceleration time of mitral valve similar to those of dipper patients.
The influence of ABPM profile on left ventricular geometry, and CV morbidity and mortality has been widely studied in the past few years. In addition, substantial evidence suggests that patients who do not show a normal fall in BP during sleep, the so‐called non‐dipping, tend to have greater end‐organ damage including LVH Citation[19], and increased CV morbidity and mortality Citation[10], Citation[11] than those who do (dipping). However, the influence of inadequate BP fall during the night on left ventricular anatomy and end‐organ damage has not yet been clarified. Some investigators reported that reduced extent of a nocturnal BP fall was associated with greater LVH and left ventricular diastolic dysfunction, increased carotid intima‐media thickness and prevalence of carotid plaques Citation[8], Citation[20–22]. Contrary to these findings, other studies failed to determine any significant difference between dipper and non‐dipper hypertension Citation[23], Citation[24]. These inconsistent results may be accounted for by some different factors. The majority of these factors are that a high percentage of the patients enrolled in these studies had been previously treated with antihypertensive drugs, which may have influenced CV remodeling. Grandi and coworkers Citation[25] found that there was no difference between dippers and non‐dippers regarding left ventricular diameter, mass, systolic and diastolic function, and aortic distensibility. Furthermore, The extent of nocturnal BP fall did not correlate with any morphofunctional parameter as well as the prevalence of LVH, and left ventricular diastolic dysfunction was similar in dippers and non‐dippers. In a more recent study, Della Mea and coworkers Citation[26] revealed that non‐dippers showed LVM, relative wall thickness, and measure of early and late diastolic peak flow velocity ratio similar to those of dippers. Conversely, Verdecchia and coworkers Citation[20] showed that LVMI was significantly higher in non‐dipper hypertensive patients than that in dipper ones.
It has been shown that hypertensive patients with no epicardial CAD have reduced CFR and increased rest coronary flow velocity even in the absence of LVH and left ventricular diastolic dysfunction Citation[2–6]. Quantitative histological studies performed from septal biopsy tissue showed that reduced coronary dilatory capacity was associated with increased arteriolar media area, perivascular and interstitial fibrosis in patients with arterial hypertension and angina pectoris in the absence of relevant coronary artery stenosis Citation[1]. These are sensitive indicators of hypertensive end‐organ damage Citation[27], Citation[28].
In a recent study, it has been shown that non‐invasive measurement of coronary flow velocity and CFR in the distal LAD using TTDE accurately reflects invasive measurement of coronary flow velocity and CFR by the Doppler guide wire method Citation[29]. In addition, although positron emission tomography has been validated as a gold standard for evaluating CFR and coronary microvascular function, it has been shown that CFR measured by TTDE has an excellent correlation with CFR measured by positron emission tomography in the corresponding myocardial area Citation[16]. Based on these observations, TTDE, which is a non‐invasive, relatively inexpensive and easily used method in clinical practice, can be considered a very suitable and reliable method for measuring CFR in hypertensive individuals.
Although there has been a lot of study evaluating relationship between circadian variation of BP and left ventricular geometry and diastolic impairment, and substantial evidence has been supported that sustained hypertension impairs CFR, to date, there has been no study investigating the influence of ABPM profile on CFR, which reflects coronary vasodilating capacity and microvascular function, in hypertensive patients free of coronary risk factors. To our knowledge, this is the first study to investigate possible effects of ABPM profile on CFR. In the present study, we found that in the absence of other CV risk factors and excessive LVH, non‐dipping BP does not alter CFR and left ventricular diastolic function more than dipping BP does. However, in our study, the study groups included newly diagnosed and never treated subjects with mild to moderate hypertension, so we do not know how long our patients were subject to increased BP. These close values of the two hypertension groups regarding CFR and left ventricular diastolic function might have resulted from shorter duration of hypertension. Therefore, this may be regarded as a limitation of our study, and further studies on subjects with longer duration of hypertension would be valuable.
In previous reports, coronary flow was measured in the middle or distal part of LAD by TTDE and the success rate was reported as 98–100% Citation[16], Citation[29]. In our study, the success rate was 100%. Because systolic heart movement causes disturbances in Doppler signal resulting in difficulties in obtaining reliable measurements during systole, we only measured peak diastolic component of coronary flow (DPFV).
It has been previously demonstrated that LVH and left ventricular diastolic dysfunction can cause CFR impairment and/or coronary microvascular dysfunction Citation[4], Citation[30]. In our study, to prevent the confounding effects of LVH on the study results, we excluded subjects with excessive LVH (LVMI equal or greater than 125 g/m2 for men and 110 g/m2 for women). Although left ventricular diastolic function was similar among the groups, we have observed that CFR directly and significantly correlated with maximum mitral E velocity and mitral E/A ratio, and negatively correlated with maximum mitral A velocity and mitral E wave deceleration time, but these correlations did not reach statistical significance (Table ). Furthermore, we have also found that CFR was independently correlated with left atrium diameter, mitral E wave deceleration time and mitral E/A ratio in stepwise linear regression analysis.
In summary, in the absence of other CV risk factors and excessive LVH, non‐dipper essential hypertensive patients show similar CFR compared with dipper ones.
References
- Schwartzkopff B., Motz W., Frenzel H., Vogt M., Knauer S., Strauer B. E. Structural and functional alterations of the intramyocardial coronary arterioles in patients with arterial hypertension. Circulation 1993; 88: 993–1003
- Antony I., Nitenberg A., Foult J. M., Aptecar E. Coronary vasodilator reserve in untreated and treated hypertensive patients with and without left ventricular hypertrophy. J Am Coll Cardiol 1993; 22: 514–520
- Opherk D., Mall G., Zebe H., Schwarz F., Weihe E., Manthey J., et al. Reduction of coronary reserve: A mechanism for angina pectoris in patients with arterial hypertension and normal coronary arteries. Circulation 1984; 69: 1–7
- Galderisi M., de Simone G., Cicala S., De Simone L., D'Errico A., Caso P., de Divitiis O. Coronary flow reserve in hypertensive patients with appropriate or inappropriate left ventricular mass. J Hypertens 2003; 21: 2183–2188
- Brush J. E., Cannon R. O III., Schenke W. H., Bonow R. O., Leon M. B., Maron B. J., et al. Angina due to microvascular disease in hypertensive patients without left ventricular hypertrophy. N Eng J Med 1988; 319: 1302–1307
- Kozakova M., Palombo C., Pratali L., Pittella G., Galetta F., L'Abbate A. Mechanisms of coronary flow reserve impairment in human hypertension. An integrated approach by transthoracic and transesophageal echocardiography. Hypertension 1997; 29: 551–559
- O'Brien E., Sheridan J., O'Malley K. Dippers and non‐dippers. Lancet 1988; 2: 397
- Kuwajima I., Suzuki Y., Shimosawa T., Kanemaru A., Hoshino S., Kuramoto K. Diminished nocturnal decline in blood pressure in elderly hypertensive patients with left ventricular hypertrophy. Am Heart J 1992; 123: 1307–1311
- Schmieder R. E., Rockstroh J. K., Aepfelbacher F., Schulze B., Messerli F. H. Gender‐specific cardiovascular adaptation due to circadian blood pressure variations in essential hypertension. Am J Hypertens 1995; 8: 1160–1166
- Yamamoto Y., Akiguchi I., Oiwa K., Hayashi M., Kimura J. Adverse effect of nighttime blood pressure on the outcome of lacunar infarct patients. Stroke 1998; 29: 570–576
- Ohkubo T., Imai Y., Tsuji I., Nagai K., Watanabe N., Minami N., et al. Relation between nocturnal decline in blood pressure and mortality. The Ohasama Study. Am J Hypertens 1997; 10: 1201–1207
- Kario K., Matsuo T., Kobayashi H., Imiya M., Matsuo M., Shimada K. Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension 1996; 27: 130–135
- Timio M., Venanzi S., Lolli S., Lippi G., Verdura C., Monarca C., et al. “Non‐dipper” hypertensive patients and progressive renal insufficiency: A 3‐year longitudinal study. Clin Nephrol 1995; 43: 382–387
- Caiati C., Zedda N., Montaldo C., Montischi R., Iliceto S. Contrast‐enhanced transthoracic second harmonic echo Doppler with adenosine: A noninvasive, rapid and effective method for coronary flow reserve assessment. J Am Coll Cardiol 1999; 34: 122–130
- Lambertz H., Tries H. P., Stein T., Lethen H. Noninvasive assessment of coronary flow reserve with transthoracic signal‐enhanced Doppler echocardiography. J Am Soc Echocardiogr 1999; 12: 186–195
- Saraste M., Koskenvuo J., Knuuti J., Toikka J., Laine H., Niemi P., Sakuma H., Hartiala J. Coronary flow reserve: Measurement with transthoracic Doppler echocardiography is reproducible and comparable with positron emission tomography. Clin Physiol 2001; 21: 114–122
- Devereux R. B., Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 1977; 55: 613–618
- Lambertz H., Tries H. P., Stein T., Lethen H. Noninvasive assessment of coronary flow reserve with transthoracic signal‐enhanced Doppler echocardiography. J Am Soc Echocardiogr 1999; 12: 186–195
- Cuspidi C., Macca G., Sampieri L., Fusi V., Severgnini B., Michev I., et al. Target organ damage and non‐dipping pattern defined by two sessions of ambulatory blood pressure monitoring in recently diagnosed essential hypertensive patients. J Hypertens 2001; 19: 1539–1545
- Verdecchia P., Schillaci G., Guerrieri M., Gatteschi C., Benemio G., Boldrini F., et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation 1990; 81: 528–536
- Pierdomenico S. D., Lapenna D., Guglielmi M. D., Costantini F., Romano F., Schiavone C., et al. Arterial disease in dipper and nondipper hypertensive patients. Am J Hypertens 1997; 10: 511–518
- Ferrara A. L., Pasanisi F., Crivaro M., Guida L., Palmieri V., Gaeta I., et al. Cardiovascular abnormalities in never‐treated hypertensives according to nondipper status. Am J Hypertens 1998; 11: 1352–1357
- Fagard R., Staessen J. A., Thijs L. The relationships between left ventricular mass and daytime and night‐time blood pressures: A meta‐analysis of comparative studies. J Hypertens 1995; 13: 823–829
- Roman M. J., Pickering T. G., Schwartz J. E., Cavallini M. C., Pini R., Devereux R. B. Is the absence of a normal nocturnal fall in blood pressure (nondipping) associated with cardiovascular target organ damage?. J Hypertens 1997; 15: 969–978
- Grandi A. M., Broggi R., Jessula A., Laurita E., Cassinerio E., Piperno F., et al. Relation of extent of nocturnal blood pressure decrease to cardiovascular remodeling in never‐treated patients with essential hypertension. Am J Cardiol 2002; 89: 1193–1196
- Della Mea P., Lupia M., Bandolin V., Guzzon S., Sonino N., Vettor R., et al. Adiponectin, insulin resistance, and left ventricular structure in dipper and nondipper essential hypertensive patients. Am J Hypertens 2005; 18: 30–35
- Schwartzkopff B., Strauer B. E. Coronary reserve and arteriolosclerosis in hypertensive heart disease. Z Kardiol 2000; 89: 32–35
- Frohlich E. D. Fibrosis and ischemia: The real risks in hypertensive heart disease. Am J Hypertens 2001; 14: 194S–199S
- Hozumi T., Yoshida K., Akasaka T., Asami Y., Ogata Y., Takagi T., et al. Noninvasive assessment of coronary flow velocity and coronary flow velocity reserve in the left anterior descending coronary artery by Doppler echocardiography: Comparison with invasive technique. J Am Coll Cardiol 1998; 32: 1251–1259
- Galderisi M., Cicala S., De Simone L., Caso P., Petrocelli A., Pietropaolo L., et al. Impact of myocardial diastolic dysfunction on coronary flow reserve in hypertensive patients with left ventricular hypertrophy. Ital Heart J 2001; 2: 677–684