Abstract
Risk of cardiovascular events within the diabetic population has decreased and survival increased with patients living longer and thus facing the development of end-stage renal disease (ESRD). This calls for good care of patient with diabetes with a focus on hypertension. Patient data were collected from 42 Finnish primary care centres. Each was asked to enrol 10–12 consecutive patients with type-2 diabetes between March 2011 and August 2012. Along with the office blood pressure measurements and laboratory tests, the presence of albuminuria was measured and glomerular filtration rate estimated (eGFR). The 2013 ESH criteria for diabetic hypertensive patients (<140/85 mmHg) was reached by 39% of all 625 study patients and 38% of the pharmacologically treated 520 patients. The absence of detectable albumin in urine was significantly associated with the control of systolic blood pressure and achievement of treatment goals. Beta blockers were the most common antihypertensive agents and patients treated with them had lower eGFR compared to those not treated with these agents. The blood pressure of patients was not in full concordance with the present guideline recommendations. However, satisfactory improvement in blood pressure control, reduction of albuminuria and hence ESRD prevention was achieved.
Introduction
Half of the Finnish men aged 35–64 years and one-third of the women in the same age group are hypertensive.[Citation1] About half a million Finns (10% of the population) received a special reimbursement for antihypertensive drug treatment and 270,000 for diabetes mellitus in 2012.[Citation2] Although both systolic and diastolic blood pressure levels are decreased markedly since the year 1972, the blood pressure level of the Finnish population is still high compared to other nations.[Citation3,Citation4] The prevalence of type-2 diabetes is increasing worldwide.[Citation5] It is estimated that the total number of patients with diabetes is at least 500,000 in Finland.[Citation6,Citation7] Due to the high frequency of hypertension in diabetes, there are accordingly a substantial number of patients with both of these conditions.
Hypertension, microalbuminuria and decreased glomerular filtration rate (GFR) are risk factors for diabetic renal failure and should be treated adequately, preferably with angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARB).[Citation7,Citation8] Decreased risk of myocardial infarction and stroke within the diabetic population has resulted in an increase in survival, with more patients living to older age and thus facing the possible development of end-stage renal disease (ESRD). This calls for more effective and extensive care of the diabetic patient with a special focus on hypertension.
The current, evidence-based Finnish Hypertension Guidelines were first introduced in the year 2002, updated in 2005 and 2009 and latest in 2014.[Citation8] In addition to published national guidelines, a series of changes supporting more effective antihypertensive treatment have taken place. Due to widespread use of generic medications, the reimbursed prices of the antihypertensive drugs have fallen. Also home blood pressure monitoring has been increasingly available. The use of antihypertensive combination therapy, fixed-dose drug combinations and new, antihypertensive drugs with improved tolerability has increased.
The primary aim of the present study was to assess the antihypertensive treatment routines of diabetic patients in Finnish general practice and weight loss with the achieved treatment results in relation to the treatment guidelines. A special attention was focused on renal function and its possible changes among patients who surpassed or failed the given guidelines.
Patients and methods
The stages of nephropathy in diabetes was an observational, cross-sectional, multicentre, study performed in the primary care in Finland. The primary objective was to investigate the prevalence of chronic kidney disease (CKD) in patients with type-2 diabetes.[Citation9] Secondary objectives included a description of current treatment status, cardiovascular comorbidity and metabolic profile. The present paper deals with the hypertensive control of these patients.
Throughout the country, 155 primary care sites were randomly invited to participate. Out of those 42, 27% agreed to join. Each site was invited to enrol 10–12 consecutive patients with type-2 diabetes, 18 years or older coming for a regular diabetes visit occurring between March 2011 and August 2012. There was no specific criterion for the known duration of diabetes. Patients with other forms of diabetes mellitus, or those participating in another clinical study were excluded. The median number of patients recruited by a physician was 15 (range 1–60). In four patients, the diagnosis of type-2 diabetes was not reliable. Thus, the final study population consists of 625 patients. All patients gave their informed consent. The study protocol was approved by the ethics review committee of the hospital district of Southern Finland and conducted in accordance with the guidelines of the declaration of Helsinki.
From each patient, the following parameters were collected from the patient documents and during the visit: age, gender, height, body weight, blood pressure, diabetes duration, current antihyperglycaemic therapy, history of dyslipidaemia, history of ischemic heart disease or stroke, smoking status and details of antihypertensive and lipid-lowering treatment. Blood pressure was measured at the office using validated oscillometric devices in sitting position according to the instructions stated in the 2009 National Guidelines for antihypertensive care.[Citation8] Finnish 2009 Guideline recommendations for patients with diabetes (< 130/80 mmHg), the ESH 2013 criteria for all hypertensive patients (<140/90 mmHg) and ESH criteria for patients with diabetes (<140/85 mmHg) were used in the analysis of the achieved antihypertensive care.[Citation8,Citation9]
Further, the patients were asked if they had ever got photocoagulation for retinopathy and if they had experienced assistance requiring hypoglycaemias. The latest available laboratory value during the last 12 months for serum creatinine, GHbA1c, total-, LDL- and HDL-cholesterol, triglycerides and blood haemoglobin were collected from patient documents.
The presence of albuminuria was measured as either urinary albumin–creatinine ratio or collected urine albumin (cU–Alb–Mi). CKD was determined based on the presence of albuminuria and decreased estimated glomerular filtration rate (eGFR) that was calculated using the CKD–EPI equation.
The sample size calculations for the main study [Citation9] were based on the prevalence of CKD of any degree and a total of 577 patients were required to estimate the prevalence with sufficient precision. For this study, the required sample size was not estimated. Data are expressed as mean (SD, range) for normally distributed continuous variables and as median (interquartile range) for variables with non-normal distributions. The patient groups were compared using the t-test for independent samples (or analysis of variance (ANOVA) in case of more than two groups) or Mann–Whitney U-test, respectively. Categorical data are expressed as number (%) of subjects and the Chi-squared test was used to study the associations between categorical variables. All the tests were two-sided and a p value <0.05 was considered statistically significant. Analysis was performed using IBM SPSS Statistics for Windows (version 22.0, IBM Corp., Armonk, NY).
Results
Altogether data from 625 patients from 42 primary care centres (27% of those invited) was analysed in the study. The median number of patients recruited by a physician was 15 (range 1–60). The mean age of the patients was 67 (10) years and 47% of the patients were female. The mean body mass index (BMI) was 33 (6.5) kg/m2. About two-thirds (67.4%) of the patients had never smoked. A history of dyslipidaemia was present in 73% and hypertension in 83% of the patients. The mean diabetes duration since diagnosis was 9.2 years and GHbA1c 6.9 (1.3) %. A diabetes history of longer than 10 years was noticed in 41% of the patients. Already diagnosed CKD was present in 429/625 (67%) of the study patients. The clinical characteristics of the study patients are presented in detail in .
Table 1. Clinical characteristics of the study patients.
The mean blood pressure of all study patients was 142 (18)/80 (11) mmHg as measured in the office. One hundred and five patients (17%) did not use any antihypertensive medication and lifestyle modification was their only mode of treatment. Of the remaining 520 patients, 100 (16%) received antihypertensive monotherapy and more than one preparation was used by 420 patients (67%). The mean blood pressure of patients who used antihypertensive medications was 142 (18)/80 (11) mmHg. One-sixth (16%, 81/520) of the patients using antihypertensive medication reached Finnish 2009 Guideline for hypertension recommendations for patients with diabetes (< 130/80 mmHg) and 38% (197/520) for the corresponding ESH 2013 criteria for patients with diabetes (<140/85 mmHg).[Citation8,Citation9] Compared to men, the treated female patients reached ESH 2013 criteria significantly more often (). Almost half of the study patients (43%, 224/520) would have reached the 2013 ESH criteria for all hypertensive patients (<140/90 mmHg) (9). For further blood pressure details are given in and Supplementary Table 1.
Table 2. Office blood pressure, achievement of different blood pressure targets and usage of antihypertensive medications in patients with diabetes.
The achievement of the Finnish 2009 Guideline targets for patients with diabetes (<130/80 mmHg) by the study patients is presented in detail in . Patients with a history of diabetic nephropathy had significantly higher systolic and lower diastolic blood pressure but had no differences in the achievement of the target (). Patients who had eGFR lower than 90 ml/min had also significantly lower diastolic blood pressure. Patients with albuminuria had significantly higher systolic blood pressure and poorer achievement of blood pressure target of <130/80 mmHg compared to those with normal urinary albumin findings. Patients with eGFR <90 ml/min achieved the blood pressure target of 130/80 twice as often as remaining patients, but without significance ().
Table 3. The achievement of blood pressure target <130/80 mmHg in association with gender, diabetic nephropathy, HbAC1 (%), eGFR and albuminuria.
The median GHbA1C levels of patients who reached the three treatment goals (<130/80, <140/85 or <140/90 mmHg) showed also no differences. The median eGFR values were same regardless the achievement of the blood pressure targets (Supplementary Table 2).
The absence of detectable albumin in urine was significantly associated with better control of systolic blood pressure and achievement of all studied treatment goals compared to patients with albuminuria (). The mean U–alb–crea ratio and cU–alb–min values were significantly lower among those patients who reached the goals of <140/85 or <140/90 mmHg ( and ).
Figure 1. Mean systolic and diastolic blood pressure (mmHg) and the achievement of <130/80 mmHg target (%) in relation to observed albuminuria (normal = green, micro = red or macro = blue) among 625 Finnish patients with diabetes. *p = 0.02, **p < 0.001.
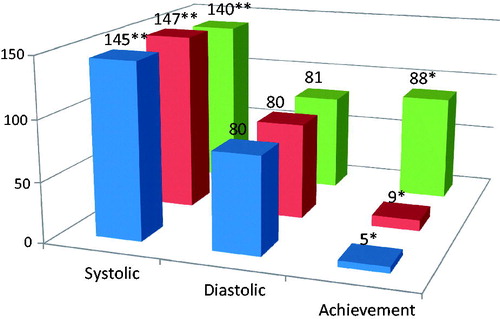
Table 4. Urinary albumin–creatinine ratio (U-alb/crea), urine albumin secretion (cU–Alb–mi) and albuminuria in patients who were treated with antihypertensive medication. Results are compared between categories of achievement of the ESH 2013 blood pressure targets.
The use of antihypertensive medications, statins and ASA was quite evenly distributed among the study patients (Supplementary Table 3). Beta blockers were the most common sole antihypertensive group, but quite seldom used as a single agent (26/313). Diuretics were used more among women and calcium antagonists among men. Patients who took diuretics or beta-blockers as a part of their medication had significantly lower median eGFR and higher proportion of patients with eGFR <90 ml/min compared with those treated without these medications. Patients who used ACE inhibitors had significantly higher eGFR compared to non-users (Supplementary Table 3). The effects of beta-blockers were studied further by considering patients with diabetes and no history of coronary artery disease separately. Median eGFR was significantly lower and the share of patients with GFR <90 ml/min equally higher among them compared to patients with a history of coronary artery disease (Supplementary Table 4).
Discussion
According to the present cross-sectional study, 39% of patients with type-2 diabetes in Finnish primary care reached the respective blood pressure target of <140/85 mmHg stated in the 2013 ESH hypertension guidelines.[Citation10] Only 17% of the studied patients were treated solely without medicines and they had results similar to those of the majority who were given pharmaceuticals. This indicates good patient selection for medical treatment. As diabetics with actively treated hypertension are most probably morbid and possess risk of developing ESRD, the discussion is concerned on them. Although the study consists only of patients with type-2 diabetes the discussion of the results can be expanded to cover all patients with diabetes.
The present data were obtained as a cross-sectional multicentre survey in the community-owned Finnish primary care sites. Considering the similarity of these sites conclusions were possible to be drawn. The homogeneity of patient material was ensured by having populations from all the regions in Finland. This type of patient collection may underestimate the morbidity of diabetes, because patients who regularly visit physician offices are most often those who are committed to their treatment. However, rather high BP levels and high comorbidity suggest that also morbid patients were included. Despite some shortcomings the adopted approach resulted in a fairly demographic patient sample.
All blood pressure measurements were performed with automated digital oscillometric devices and readings were keyed in as integers. There was no rounding to 0–5 mmHg as was usual with mercury sphygmomanometer. Automated technique eliminates effects of the digit preference, which is known to hamper the interpretation of BP results by traditional sphygmomanometer and lead to underestimation of BP levels.[Citation11] Recently, Giorgini et al (2014) reviewed BP measurement protocols of studies published in 1990–2014 and found that in 47% of the papers the type of the BP-measuring device was not stated and only in 16% automated oscillometric device was adopted.[Citation12] Therefore, it is unjustified to compare results from the present study to older BP population studies without this consideration.
More than a decade ago 22% of the Finnish-treated hypertensive men and 26% of women reached the treatment target of 140/85 mmHg in general practice.[Citation13] A more recent survey from 2009 revealed no better results, 23% and 24%, respectively.[Citation4] This poor blood pressure control observed in Finland parallels the corresponding results from other European countries.[Citation3] However, according to the NHANES study, 52% of adult hypertensive patients reached the treatment goal of 140/90 mmHg in the USA in 2011–2012, suggesting that better treatment results would be achievable also in Europe, as was later documented from Germany by Ruckert et al.[Citation14,Citation15] Although the present study deals only with hypertensive patients with diabetes, this hope seems realistic also in Finland as nearly half (43%) of the treated study patients would have met with the NHANES equal ESH 2013 criteria (<140/90) and the number of the patients reaching the target has clearly increased since 2006.[Citation10,Citation16]
The proportion of Finnish diabetics reaching blood pressure target of ≤130/80 (9%) mmHg was very marginal in 2006.[Citation4] Our study from 2006 shows that Finnish general practitioners were more aware of treatment guidelines for diabetic patients with hypertension compared to patients with uncomplicated hypertension.[Citation16] Thus, it is quite surprising that during six years only moderate improvement in blood pressure control (9% vs. 15% in the present study) has been achieved. Insufficient guideline penetration into physicians’ daily work and/or justified critical interpretation of the guidelines in selected cases may be the explanation. The slacking of BP targets for the treatment of diabetic hypertensive patients might be seen as a support of the latter assumption. In the present study glycaemic control was fairly good and was not related to the blood pressure levels or treatment results achieved.
Abnormal urinary findings or subnormal eGFR are common findings among patients with type-2 diabetes. Roughly, 70% of our patients had previously diagnosed diabetic nephropathy and 25% albuminuria at the time of the study and were in risk of developing progressive glomerular damage.[Citation10] The absence of albuminuria marks sufficient BP care and is a hallmark of good treatment of hypertensive patients with diabetes.[Citation17,Citation18] In the present study, the lack of albumin in urine was significantly associated with blood pressure control and achievement of all studied blood pressure goals (). This result was mainly due to use of ACE inhibitors and ARBs to susceptible patients. Despite the association between lack of albuminuria and good blood pressure control the eGFR did not differ significantly between patients who met or failed the guideline BP levels.
Surprisingly, many patients without coronary artery disease or heart failure were treated with beta blockers. Beta blockers have been popular antihypertensive agents in Finland and their use has even increased.[Citation4,Citation5] The use of beta blockers is indicated if the patient suffers from symptomatic coronary artery disease, cardiac insufficiency or cardiac arrhythmias. The present study shows that the use of beta blockers in patients without cardiovascular disease alone or in combination was associated with lower eGFR (Supplementary Table 4). Of course, when treating severely hypertensive patients combination therapy very often necessitates the adoption of beta blockade. As a matter of fact, 92% of beta blockers were prescribed as an additive component. Prescribing beta blockers in non-complicated hypertension should always be well justified.
The present study suggest that despite effective guideline promoting the BP treatment results among Finnish patients with type-2 diabetes are not in full concordance with guideline recommendations. Roughly, 40% of the studied patients received good blood pressure care and proper proteinuria control. Improving the current situation is substantial task. Better medications, more frequent visits and also population-level initiatives may be needed. Guideline compliance of the physicians should be taken into account, because there may be justified criticism or failing trustworthiness of the guidelines. Treatment alternatives should be evaluated carefully. Beta blockers are still the most often adopted drug regimen in the antihypertensive treatment and diminished eGFR may accompany their unjustified usage.
Supplement_Table_4..doc
Download MS Word (37 KB)Supplement_Table_3..doc
Download MS Word (58.5 KB)Supplement_Table_2doc.doc
Download MS Word (33 KB)Supplement_Table_1..docx
Download MS Word (17.8 KB)Acknowledgements
This study was supported by Boheringer Ingelheim Pharma GmbH. We acknowledge the recruitment of the patients to the study by Drs N. Aaltonen, B-M. Bjon, L. Eriksson, T. Hälvä-Torday, S. Hietaniemi, H. Jaatinen, P. Kalliola, V.Kallioniemi, P. Kauppinen, M. Kilponen, P. Korhonen-Jalonen, R. Kurttila, M. Laine, L. Linnasmägi, J. Linros, I. Mikkai, J. Nikula, M. Nurminen, L. Passi, L. Petlin, J. Rahko, J. Saarela, E-C. Schmuser, A. VAden, M. Vähätalo, J. Vidgren, T. Wahe-Rohrbach, A, Patala, H. Levänen, J. Strand, K. Askonen, L. Hiltunen, S. Moilanen, T. Valle.
Disclosure statement
This study was supported by Boheringer Ingelheim Pharma GmbH. Kaj Metsärinne, Ilkka Kantola, Leo Niskanen, Aila Rissanen and Antti Virkamäki are members of Boheringer Ingelheim Advisor Board and TA an employee of the company. NP, VK, JV and TP have no conflict of interest.
References
- Kastarinen MJ, Antikainen RL, Laatikainen TK, et al. Trends in hypertension care in eastern and south-western Finland during 1982–2002. J Hypertens. 2006;24:829–836.
- Finnish Statistics on Medicines. Finnish medicines agency FIMEA and social insurance innstitution. Helsinki: Edita Prima Oy; 2013. p. 126.
- Kastarinen M, Antikainen R, Peltonen M, et al. Prevalence, awareness and treatment of hypertension in Finland during 1982–2007. J Hypertens. 2009;27:1552–9.
- Varis J, Savola H, Vesalainen R, et al. Treatment of hypertension in Finnish general practice seems unsatisfactory despite evidence based guidelines. Blood Press. 2009;18:62–7.
- International Diabetes Federation. IDF diabetes atlas. 6th ed. Brussels, Belgium: International Diabetes Federation; 2013. Available from: http://www.diabetesatlas.org.
- Koski S. Diabetesbarometri; 2010. p. 6–7. www.diabetes.fi/files/1377/Diabetesbarometri_2010.pdf.
- Current Care Guideline for Diabetes. Working group appointed by the Finnish Medical Society Duodecim and the Medical Advisory Board of the Finnish Diabetic Society. Duodecim. 2013;129:2390–2391.
- Hypertension. Available from: http//.kaypahoito.fi/web/english/guidelineabstracts/guideline?id=ccs00014&suositusid=hoi04010.
- Metsärinne K, Bröijersen A, Kantola I, et al. for the STONE study investigators. High prevalence of chronic kidney disease in Finnish patients with type 2 diabetes treated in primary care. Prim Care Diabetes. 2015;9:31–8.
- Mancia C, Fagard R, Narkiewicz R, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension of the European society of hypertension (ESH) and of the European society of cardiology (ESC). J Hypertens. 2013;31:1281–357.
- Roubsanthisuk W, Wongsurin U, Saravich S, et al. Blood Pressure determination by traditionally trained personnel is less reliable and tends to underestimate the severity of moderate to severe hypertension. Blood Press Monit. 2007;12:61–68.
- Giorgini P, Weder A, Jackson E, et al. A review of blood pressure measurement protocols among hypertension trials; implications for “evidence-based” clinical practice. J Am Soc Hypertens. 2014;8:670–676.
- Meriranta P, Tikkanen I, Kumpusalo E. Verenpainepotilas terveyskeskuksessa: hoitotulokset paranemassa. Suomen Lääkärilehti. 2004; 36:3253–3258.
- Yoon SS, Carroll MD, Fryar CD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS Data Brief. 2015;(220):1–8.
- Rückert I-M, Schunk M, Holle R, et al. Blood pressure and lipid management fall far short in persons with type 2 diabetes: results from the DIAB-CORE consortium including six German population-based studies. Cardiovasc Diabetol. 2012;11:11–50.
- Varis J, Tumpula O, Kantola I. Self-reported awareness of the hypertension guidelines does Not lead to knowledge of the treatment thresholds. J Res Cardiol. 2015;2015:722338. doi:10.5171/2015.722338.
- Menne J, Izzo JL, Jr, Ito S, et al. ROADMAP investigators. Prevention of microalbuminuria in patients with type 2 diabetes and hypertension. J Hypertens. 2012;30:1679–8.
- Emdin CA, Rahimi K, Neal B, et al. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA 2015;313:603–615.
