Abstract
Targeted screening of hypertension in childhood might be more efficient than universal screening. We estimated the sensitivity, specificity, negative and positive predictive values of combined parental history of hypertension and overweight/obesity for the diagnosis of hypertension in 5207 children aged 10–14 years. Children had hypertension if they had sustained elevated blood pressure over three separate visits. The prevalence of hypertension was 2.2%. 14% of children were overweight or obese, 20% had a positive history of hypertension in at least one parent and 30% had either or both conditions. Targeted screening of hypertension to children with either overweight/obesity or with hypertensive parents limits the proportion of children (30%) to screen and identifies up to 65% of all hypertensive cases.
Introduction
Hypertension is a leading cause of mortality worldwide.[Citation1] There is growing evidence that elevated blood pressure (BP) takes its origin early in life and tracks into adulthood, raising the possibility of a lifelong reduction in cardiovascular risk through early detection and intervention.[Citation2–5] As a consequence, several health professional societies recommend universal screening for hypertension in children.[Citation6,Citation7]
Recent publications highlight, however, the lack of high-level evidence to support this recommendation and question, first, whether hypertension should be screened in childhood and, second, if recommended, what might be the most efficient screening strategy.[Citation8–10] Universal screening of hypertension performs poorly in childhood, mainly because of the low prevalence of hypertension.[Citation11] There is also evidence that paediatricians are reluctant to do such screening and underdiagnose hypertension.[Citation12] Targeted screening to children at higher risk of hypertension has therefore been proposed.[Citation9] Overweight/obesity and parental history of hypertension are recognized risk factors for hypertension in childhood.[Citation8,Citation11] Both characteristics are relatively easy to assess in daily clinical care. Their ability to capture simultaneously environmental and genetic risk factors further strengthens their value as clinical tools to identify children with hypertension.[Citation13] Targeting screening to children with any of these characteristics could be a more efficient strategy to identify hypertension in children.
In a previous study, we showed that targeted screening of children with a parental history of hypertension did not perform better than universal screening.[Citation14] However, the screening performance of parental history of hypertension was evaluated in isolation, without considering other risk factors for childhood hypertension. Therefore, in this study, our goal was to assess the performance of combined risk factors for hypertension, i.e. parental history of hypertension and overweight/obesity, which both are relatively easily assessed, to identify children with hypertension. We first assessed the strength of the associations of overweight, obesity, and parental history of hypertension with hypertension in children. Second, we estimated the sensitivity, specificity, negative and positive predictive values of these factors in isolation or in combination for the identification of hypertension in children.
Materials and methods
Data source
We used data from a school-based survey conducted between September 2005 and May 2006 in the state of Vaud, Switzerland.[Citation11] The vast majority (up to 96%) of children living in this region attend a public school. For the survey, all children from all public 6th grade classes (mean age 12 years) in the state were invited to participate without any specific exclusion criteria. Participation was voluntary. No catch-up visit could be organized for children who were away from school on the day of the visit. Approval was obtained from the directors of schools and from the Ethics Committee of the University of Lausanne. Children and one of their parents gave written informed consent.
Children completed a pretested questionnaire at school based on the international Health Behavior in School-aged Children Study on their physical activity, sedentary behaviours, and dietary habits.[Citation15] Age and nationality of participants were obtained from school files. The parents completed a separate structured questionnaire which was filled out at home. They were asked about their age, educational level, nationality, current height and weight, smoking, and diagnosis or treatment for hypertension, hypercholesterolemia, and diabetes. Child’s birth weight, gestational age, duration of breast feeding and exposure to smoking during pregnancy were also gathered from the parental questionnaire.
At the initial screening visit, the children’s weight (to the nearest 0.1 kg) and height (to the nearest 0.1 cm) were measured by trained officers with electronic scales and fixed stadiometers. The children wore light clothes but no shoes. Blood pressure (BP) was measured with clinically validated oscillometric devices (Omron M6; Omron Healthcare Europe BV, Hoofddrop, the Netherlands).[Citation16] Accuracy of BP readings of all oscillometric devices used in the study was checked once by comparing the obtained BP values with those obtained from a mercury sphygmomanometer connected to the automated device using a Y tube. The cuff width was adapted to the mid-arm circumference (paediatric cuff (17.0–21.9 cm) or normal cuff (22.0–32.0 cm). Children were measured in the seated position, on the right arm, after an initial five-minute rest. Three BP readings (to the nearest 1 mmHg) were obtained at one-minute intervals. The average of the last two readings was used for analysis. Children who had an elevated BP according to the American reference data, i.e. BP ≥ the 95th percentile for age, gender and height, had BP measured at up to two additional visits at one-week intervals.[Citation6] The latter measurements were done by specifically trained school nurses.
Hypertension in children
A child was considered hypertensive if he/she had sustained elevated BP, i.e. systolic or diastolic BP at or above the sex-, age-, and height-specific 95th percentile according to the US reference data, at each of the three separated visits.[Citation6] Stage 1 hypertension was defined as systolic or diastolic BP between the sex-, age-, and height-specific 95th and the 99th percentile +5mmHg, and stage 2 hypertension as systolic or diastolic BP above the sex-, age-, and height-specific 99th percentile +5mmHg.[Citation6]
Risk factors
Overweight and obesity
Body weight was categorized into three mutually exclusive categories according to body mass index (BMI). BMI was computed by dividing weight by height squared (kg/m2). Normal weight was defined as a BMI below the 85th percentile of the US reference data, overweight as a BMI between the 85th and the 94th percentile, and obesity as a BMI above the 95th percentile.[Citation17]
Parental history of hypertension
Parents who had ever been told by a physician to be hypertensive or who currently took a drug for hypertension were considered to be hypertensive.[Citation14] Parental history was considered as unknown if the parent did not respond to the question or reported not to know whether she/he had elevated BP. Parental history of hypertension was then categorized into three mutually exclusive categories: (1) negative in both parents or negative in one parent and unknown in the other, (2) unknown in both parents and (3) positive in either or both parents.
Other variables
Children’s age, sex, sedentary behaviour and physical activity, dietary habits, as well as their parent’s nationality and education level, were considered a priori as potential confounders of the associations between overweight/obesity or parental history of hypertension and hypertension in children.[Citation8,Citation11,Citation18] Sedentary behaviour was assessed by the self-reported weekly screen time (hours) including television, video games and Internet watching. Physical activity was assessed by the self-reported weekly walking time (hours). Dietary habits were assessed by the self-reported frequency of intake of fruits, vegetables, sugar-sweetened drinks and chips (assessed by the question: “on how many days per week do you usually eat X?”; possible answers: <1 day/week, 1 day/week, 2–4 days/week, 5–6 days/week, 7 days/week, or several times every day). Parents’ nationality was categorized into “at least one Swiss parent” and “no Swiss parent”. Parental education was categorized into primary (primary school completed), secondary (high school or vocational training completed), and tertiary (university degree). The highest educational degree of either parent was considered.
Small-for-gestational age (SGA), defined as a birth weight below the sex-specific 10th percentile of weight for gestational age based on US reference data, was assessed as potential risk factor for targeted screening of hypertension in children.[Citation19–21]
Statistical analysis
We used logistic regression modelling to assess the associations of hypertension with body weight categories (normal weight, overweight, and obesity) and parental history of hypertension (either or both parents with a history of hypertension). Crude OR and ORs adjusted for selected potential confounders were computed with 95% confidence intervals (CI). We included only subjects with complete data.
The performance, expressed as sensitivity, specificity, positive, and negative predictive values, of overweight/obesity and parental history of hypertension to identify hypertension in children was assessed and 95% binomial proportion CI were calculated. Overweight/obesity and parental history of hypertension were first considered separately and second in combination. In additional analyses, we also assessed the performance of combined overweight/obesity or parental history of hypertension to identify stage 2 hypertension in children. Sensitivity was defined as the proportion of children with hypertension correctly identified by a risk factor (being overweight/obese or having a positive parental history of hypertension), specificity as the proportion of children without hypertension correctly identified by the lack of the risk factor (being of normal weight or not having a positive parental history of hypertension), positive predictive value as the proportion of children with hypertension identified by the risk factor, and negative predictive value as the proportion of children without hypertension without the risk factor.[Citation22] All analyses were performed with STATA 11 (StataCorp LP, College Station, TX) and two-sided p-value <.05 was considered as statistically significant.
Results
About 5207 (76%) children out of 6873 eligible children participated in the survey. They were aged 10–14 years. General characteristics of participants are presented in . Hypertension was diagnosed in 2.2% of children (stage 1: 1.8%; stage 2: 0.4%). About 14% of children were overweight or obese. A positive history of hypertension in either or both parents was reported by 19.8% of parents. 3.7% of children carried both risk factors while 30.3% of them carried either of them. shows the prevalence of hypertension among children according to categories of body weight and family history of hypertension.
Figure 1. Prevalence (with upper bound of the 95% confidence interval) of hypertension among children according to categories of body weight and family history (H) of hypertension (-: mother and father did not report having hypertension; ?: unknown history; +: one or two parents reported having hypertension).
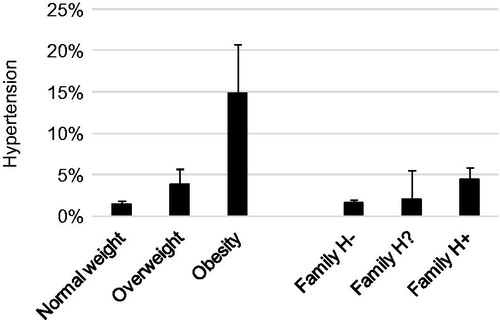
Table 1. Characteristics of children and parents.
Parental history of hypertension, overweight and obesity were strongly associated with hypertension in children (). After adjustment for all selected potential confounders, these associations remained highly significant ().
Table 2. Association between overweight, obesity and parental history of hypertension and hypertension in children (N = 5207).
In our study sample, there was no direct association between SGA and childhood hypertension (crude odds ratios (OR) 0.6, 95%CI 0.3–1.6, p = .32). Further, there is evidence that the association is present only when current weight is taken into account in the analysis.[Citation20,Citation21] Hence, we did not include SGA as a risk factor for targeted screening for the identification of hypertension in children. Other potential risk factors like parents’ educational level and nationality, children’ sedentary behaviour, physical activity and dietary habits were not statistically or only marginally associated with hypertension in children (data not shown).
The performance of screening for hypertension in children with a parental history of hypertension, being obese or being overweight/obese, in isolation or in combination, is reported in . Considered in isolation, the sensitivity (40.7%) and positive predictive value (4.5%) of parental history of hypertension were relatively low. Sensitivity and positive predictive values of overweight/obesity considered in isolation were higher, but remained relatively low (respectively 43.4% and 6.6%). For both factors, the negative predictive values were high. When considered together, the sensitivity of either overweight/obesity or parental history of hypertension for the identification of childhood hypertension was much higher (64.6%), but the positive predictive value remained low (4.6%).
Table 3. Clinical performance of parental history of hypertension, overweight/obesity, and combination of parental history of hypertension and overweight/obesity for the identification of hypertension in children (N = 5207).
In additional analyses, combined overweight/obesity or parental history of hypertension had a similar performance to identify stage 2 hypertension in children (sensitivity 68.2%, specificity 69.9%, positive predictive value 1%) compared with stages 1 and 2 hypertension considered together.
Discussion
Our study confirms that overweight, obesity and parental history of hypertension are major independent risk factors for hypertension in children.[Citation11,Citation23–25] The performances of overweight, obesity and parental history of hypertension to identify hypertension in children were weak when considered in isolation. However, considered together, their sensitivity increased substantially. Thus, restricting screening of hypertension to children with either overweight/obesity or hypertensive parents would substantially limit the proportion of children to screen (30%) and identify up to 65% of hypertensive cases. Such a strategy would, however, also miss over one third of all hypertensive children.
To our knowledge, the performance of a targeted screening strategy for hypertension – that is, sustained elevated blood pressure – combining strong and easily measurable risk factors has never been reported. Strengths of our study are the large sample size, the school-based setting covering over 96% of the population in this age category, a fair participation rate (76%), and the population-based sample. Another major strength of our study is the rigorous assessment of hypertension in children based on measurements obtained on up to three visits, by trained survey officers, and using clinically validated oscillometric devices.[Citation11]
Several limitations need to be highlighted. Children who missed the initial screening visit could not be reassessed later. This may have led to some underestimation of hypertension in children. Moreover, there was no information available on non-participating children and their parents, particularly regarding their BMI. We can therefore not exclude that they differed significantly from the study population and thus induced some selection bias. A major limitation is the self-reported nature of parents’ data, which probably weakens the association with hypertension in children as self-reported status of BP is prone to underreporting.[Citation26] However, as paediatricians do not measure parents’ BP in practice, the use of parental history rather than an objective BP measurement confers a greater generalizability to our results. Further, we had no information on the cause of hypertension. It seems however reasonable to assume that most hypertensive cases identified in this age category are primary or essential.[Citation27] Other limitations are the lack of information on pubertal status, ethnicity and the fact that it is a post hoc analysis with data from a study not designed to address the present research question.
The results of our study are limited to children aged 10–14 years. The prevalence of primary hypertension is expected to be higher in older than younger children. Family history could therefore perform better in older than younger children. The proportion of identified hypertensive cases could be higher in a population with a greater prevalence of childhood overweight/obesity. It would therefore be useful to assess the performance of such a targeted screening strategy in populations where the prevalence of hypertension and its determinants are largely different.
Clinical perspective
The aim of any screening strategy is to identify in a healthy population those individuals who are at increased risk to develop a disease or who have the disease at an early stage and to offer an early intervention if necessary.[Citation28] Screening of hypertension in children aims to reduce lifelong CVD risk and can be seen as a part of cardiovascular disease (CVD) prevention starting in childhood.[Citation5] Universal screening of hypertension for children older than three years is advocated by several health professional societies but performs poorly, notably due to the low prevalence of hypertension in children.[Citation6–7] Targeted screening has therefore been proposed.[Citation9,Citation14]
To be worthwhile for screening a risk factor needs to be strongly associated with the disease.[Citation14,Citation22] Our study shows that targeted screening, even to the strongest risk factors for hypertension in childhood, performs poorly when they are considered in isolation. A way to partly overcome this limitation is to combine several risk factors. By combining the strongest risk factors for hypertension in childhood, i.e. being overweight/obese and having parental history of hypertension, the proportion of children to screen is limited to 30% and the performance increases substantially as up to 65% hypertensive cases were identified. Inversely, the targeted strategy leaves however also around a third of all hypertensive children in the population undetected. In case of rare and serious conditions, typically as those screened during the neonatal period, such a performance would certainly not be satisfactory. For a CV risk factor, however, without clinical disease expected for decades, it is probably much more debatable, in particular given the repeated nature of the screening procedure.
Other potential risk factors for childhood hypertension like SGA, sedentary behaviour, physical activity and dietary habits were not or only marginally associated with hypertension in our sample. Including these risk factors in a combined targeted screening strategy would therefore not improve its performance substantially.
A limitation of screening for hypertension in children, whether universal or targeted, remains the low positive predictive value of any of these strategies. The low prevalence of child hypertension strongly limits the interest of any early detection strategy. The positive predictive value of universal screening is 2.2%, as it corresponds to the prevalence of childhood hypertension in the population. By restricting screening to children with overweight/obesity or positive parental history of hypertension, the positive predictive value will increase, yet remains low (5%), which means that a substantial number of children with normal BP will still be unnecessarily screened and some of them further investigated to exclude hypertension.
In conclusion, overweight/obese children and children with hypertensive parents were are at higher risk of hypertension. Considered in isolation, these risk factors perform poorly to identify hypertension in children but performance was largely improved by considering these two risk factors jointly. Restricting screening of hypertension to children with overweight/obesity or hypertensive parents would substantially limit the proportion of children to screen and allow the identification of a relatively large proportion of all hypertensive cases in the population.
Disclosure statement
The authors report no conflicts of interest.
Funding
The study was funded by a grant from the Swiss National Science Foundation [No 3200B0-109999/1].
References
- Lawes CM, Vander Hoorn S, International Society of Hypertension, et al. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518.
- Berenson GS, Srinivasan SR, Bao W, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa heart study. N Engl J Med. 1998;338:1650–1656.
- McNiece KL, Gupta-Malhotra M, Samuels J, et al. Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 National high blood pressure education program working group staging criteria. Hypertension. 2007;50:392–395.
- Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180.
- Labarthe DR. Prevention of cardiovascular risk factors in the first place. Prev Med. 1999;29:S72–S78.
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576.
- Lurbe E, Cifkova R, Cruickshank JK, et al. Management of high blood pressure in children and adolescents: recommendations of the European society of hypertension. J Hypertens. 2009;27:1719–1742.
- Thompson M, Dana T, Bougatsos C, et al. Screening for hypertension in children and adolescents to prevent cardiovascular disease. Pediatrics. 2013;131:490–525.
- Chiolero A, Bovet P, Paradis G. Screening for elevated blood pressure in children and adolescents: a critical appraisal. JAMA Pediatr. 2013;167:266–273.
- Chiolero A, Bovet P, Paradis G. Controversy about hypertension screening in children: a public health perspective. J Hypertens. 2015;33:1352–1355.
- Chiolero A, Cachat F, Burnier M, et al. Prevalence of hypertension in schoolchildren based on repeated measurements and association with overweight. J Hypertens. 2007;25:2209–2217.
- Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874–879.
- Valdez R, Greenlund KJ, Khoury MJ, et al. Is family history a useful tool for detecting children at risk for diabetes and cardiovascular diseases? A public health perspective. Pediatrics. 2007;120:S78–S86.
- Bloetzer C, Paccaud F, Burnier M, et al. Performance of parental history for the targeted screening of hypertension in children. J Hypertens. 2015;33:1167–1173.
- Janssen I, Katzmarzyk PT, Boyce WF, et al. Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obes Rev. 2005;6:123–132.
- Topouchian JA, El Assaad MA, Orobinskaia LV, et al. Validation of two automatic devices for self-measurement of blood pressure according to the International protocol of the European society of hypertension: the Omron M6 (HEM-7001-E) and the Omron R7 (HEM 637-IT). Blood Press Monit. 2006;11:165–171.
- Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190.
- Giussani M, Antolini L, Brambilla P, et al. Cardiovascular risk assessment in children: role of physical activity, family history and parental smoking on BMI and blood pressure. J Hypertens. 2013;31:983–992.
- Olsen IE, Groveman SA, Lawson ML, et al. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–e224.
- Huxley R, Neil A, Collins R. Unravelling the fetal origins hypothesis: is there really an inverse association between birthweight and subsequent blood pressure? Lancet. 2002;360:659–665.
- Chiolero A, Paradis G, Kaufman JS. Assessing the possible direct effect of birth weight on childhood blood pressure: a sensitivity analysis. Am J Epidemiol. 2014;179:4–11.
- Grimes DA, Schulz KF. Uses and abuses of screening tests. Lancet. 2002;359:881–884.
- Parikh NI, Pencina MJ, Wang TJ, et al. A risk score for predicting near-term incidence of hypertension: the Framingham heart study. Ann Intern Med. 2008;148:102–110.
- Munger RG, Prineas RJ, Gomez-Marin O. Persistent elevation of blood pressure among children with a family history of hypertension: the Minneapolis children's blood pressure study. J Hypertens. 1988;6:647–653.
- Whincup PH, Cook DG, Shaper AG. Early influences on blood pressure: a study of children aged 5-7 years. BMJ. 1989;299:587–591.
- Vargas CM, Burt VL, Gillum RF, et al. Validity of self-reported hypertension in the National health and nutrition examination survey III, 1988-1991. Prev Med. 1997;26:678–685.
- McCrindle BW. Assessment and management of hypertension in children and adolescents. Nat Rev Cardiol. 2010;7:155–163.
- Raffles AE, Gray JAM. Screening: evidence and practice. Oxford: Oxford University Press; 2007.
