Abstract
Objective: There is an association between exercise systolic blood pressure (SBP) and cardiovascular disease and mortality. The aim of this study was to investigate this association, with 35 years of follow-up.
Methods: Through 1972–75, 2014 healthy, middle-aged men underwent thorough medical examination and a bicycle exercise test. 1999 participants completed six minutes at 100 W. SBP was measured manually, both before the test and every two minutes during the test. Highest SBP measured during the first six minutes (SBP100W) was used in further analyses.
Results: Participants were divided into quartiles (Q) based on their SBP100W; Q1: 100–160 mm Hg (n = 457), Q2: 165–175 mm Hg (n = 508), Q3: 180–195 mm Hg (n = 545) and Q4: 200–275 mm Hg (n = 489). After 35-years follow-up, there was a significant association between exercise SBP at baseline and cardiovascular disease and mortality. In the multivariate analysis adjusting for resting SBP, age, smoking status, total serum cholesterol and family history of coronary heart disease, as well as physical fitness, there is a 1.39-fold (CI: 1.00–1.93, p = 0.05) increased risk of cardiovascular mortality in Q4 compared to Q1. When not adjusting for physical fitness, there is a 1.29-fold (CI: 1.03–1.61, p = 0.02) increase in risk of cardiovascular disease between Q1 and Q4.
Conclusions: The results of this study suggest that the association between exercise SBP at moderate workload and cardiovascular disease and mortality in middle-aged men extends through as long as 35 years and into old ages.
Introduction
A hypertensive response to exercise at moderate workload is associated with future risk of cardiovascular (CV) disease and mortality [Citation1–3]. However, some studies have shown conflicting results, and the results can potentially also be cancelled out by resting systolic blood pressure (SBP) [Citation2,Citation4]. We have previously shown that peak exercise SBP at the moderate workload of 100 W (SBP100W) predicts fatal coronary heart disease (CHD) and CV mortality in apparently healthy, middle-aged, Caucasian men after 16 years of follow-up [Citation5,Citation6]. Regarding CV mortality, SBP100W is independent of resting SBP after 21 years of follow-up [Citation7]. An increase in exercise SBP during seven years has also been reported by us to predict long-term risk of CHD and mortality [Citation8]. However, to our knowledge, the implications of exercise SBP on CV mortality have not been investigated beyond 21 years in a population of healthy, middle-aged men.
The aim of this study was to investigate the possible association between exercise SBP and both fatal and non-fatal CV disease in the Oslo Ischemia Study, through 35 years of follow-up, n = 1999. Preliminary mortality results from these analyses have been presented earlier [Citation9], but not fully published.
Methods
Participants and End Points
During 1972–1975, 2341 apparently healthy male employees aged 40–59 years were invited from five companies or governmental agencies to participate in the Oslo Ischemia Study. Participants suffering from advanced pulmonary, renal or liver disease or other chronic diseases or disorders including known or suspected CV disease were excluded. Participants receiving pharmacological treatment, including antihypertensive treatment, were not permitted to participate. The participants also had to be free from disorders of the musculoskeletal system preventing them from being able to complete a bicycle test. Further details on selection methods and exclusion criteria for this cohort have been presented earlier [Citation10,Citation11].
Of the 2341 men considered eligible, 2014 (86%) agreed to participate and gave their informed consent before entering the initial examination, Survey 1 (see Clinical Examination below).
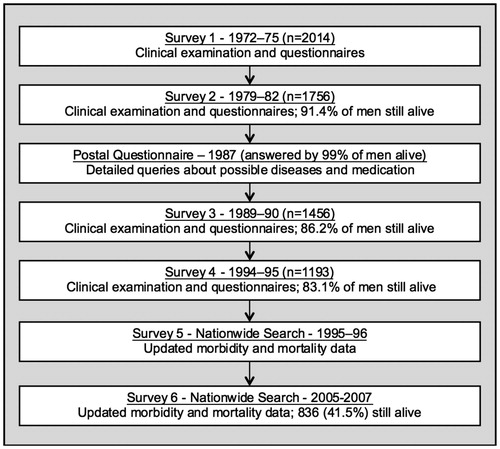
CV mortality is defined as fatal myocardial infarction, stroke (ischaemic or haemorrhagic), ruptured aortic aneurysm and sudden death. CV disease is defined as fatal or non-fatal myocardial infarction, angina pectoris, heart failure, fatal or non-fatal stroke, transitory ischaemic attack, abdominal aortic aneurysm, peripheral artery disease treated with angioplasty and claudicatio intermittens. Endpoints are verified by systematic review of patient records (Survey 5 and 6, ). Angina pectoris was defined by having characteristic symptoms or the written diagnosis of angina pectoris in hospital records in combination with documented use of short- or long-acting nitrates. Most of the men diagnosed with angina pectoris also exhibited objective signs of exercise-induced ischemia during follow-up examinations. Observation time for CV disease is time from baseline to the first occurring CV event for each participant.
Clinical Examination
At Survey 1, all participants underwent thorough medical examination by the same physician (J.E.) and laboratory testing, including chest X-ray imaging, spirometry, resting blood pressure measurement in supine position and resting electrocardiography (ECG), as described earlier [Citation12]. Medical history and family history of CHD were obtained through questionnaires.
Exercise Testing
Participants had to perform a symptom-limited, ECG-monitored bicycle test starting at a workload of 100 W, equal to 600 kilopondmeter (kpm)/min and 5.5 metabolic equivalents (METs). The test was performed on an electrically braked, stationary bicycle with ergometer. After the initial six minutes, the workload was increased with 50 W every sixth minute. The participants were encouraged to continue exercising until near exhaustion or objective signs of cardiac ischaemia appeared on ECG.
Exercise Blood Pressure Measurements
SBP was measured auscultatory to the nearest 5 mm Hg every second minute, using a mercury sphygmomanometer. SBP100W was defined as the highest measured SBP at the 100 W workload and represented the third measurement of blood pressure in almost all participants. Physical fitness was defined as the sum of work (Joule) at all workloads divided by body weight (kg). This definition was used because of its close correlation with maximal oxygen uptake and by this, the most accepted definition of physical fitness [Citation11]. Peak SBP tended to be the last measurement before termination of the test. Due to methodological difficulties with non-invasive measurements during exercise tests, diastolic blood pressure was not measured. Further details on blood pressure measurement and the bicycle test have been presented elsewhere [Citation5].
Follow-Up
Similar clinical examination and exercise test were performed during Surveys 2–4, as part of the Oslo Ischemia Study. Morbidity data were later obtained from one postal questionnaire in 1987, the clinical surveys in 1979–82, 1989–90 and 1994–95 and two nationwide searches using data from Statistics Norway and medical records from all Norwegian hospitals in 1995–96 and 2005–07 ().
Statistical Methods
Associations between CV disease and mortality and exercise blood pressure was tested using quartile groups of SBP100W. The risks of CV disease and mortality were estimated with Kaplan-Meier plots. Cox proportional hazards model were used when calculating hazard ratios. In the multivariate analyses, adjustments were made using baseline characteristics: age, resting SBP, smoking status, total serum cholesterol, and family history of CHD. Multivariate analyses were also performed with additional adjustments for physical fitness. Tests are two-sided and statistical significance was defined as α ≤0.05. The analyses were made using JMP 13.0.0, SAS Institute Inc. (Cary, NC, United States).
Results
Of the 2014 participants included in Survey 1, 1999 completed the 100 W stage of the bicycle test. Baseline characteristics are presented in . Average age of the participants was 49.8 years and the average resting SBP was within today’s definition of normotension, with 130.1 mm Hg. 43.8% were current smokers and average level of total serum cholesterol was 6.7 mmol/l. 22.6% had family history of CHD. Participants were divided into quartiles (Q) based on their SBP100W; Q1: 100–160 mm Hg (n = 457), Q2: 165–175 mm Hg (n = 508), Q3: 180–195 mm Hg (n = 545) and Q4: 200–275 mm Hg (n = 489).
Table 1. Baseline Characteristics of Participants.
After 35 years of follow-up, there was a significant association between SBP100W and CV mortality in healthy, middle-aged men (). The risk of CV mortality increases with increasing SBP100W in a quartile-based, unadjusted model. Unadjusted, there is a 3.06-fold increase in risk of CV mortality in Q4 compared to Q1 (confidence interval (CI): 2.36–4.01).
Figure 2. Kaplan-Meier plot showing mortality from cardiovascular disease in 1999 participants divided in quartiles of SBP100W and followed-up for 35 years. Fatal cardiovascular disease includes fatal myocardial infarction, stroke, ruptured aortic aneurysm and sudden death. SBP100W: Peak systolic blood pressure at 100 W workload; CV: cardiovascular.
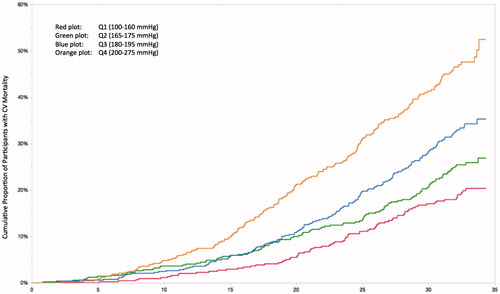
With an increase of one standard deviation (SD) in SBP100W, equal to 24.2 mm Hg, there was a 1.17-fold increase (p < 0.006, CI: 1.05–1.31) in CV mortality in a multivariate analysis, with adjustments for resting SBP, age, smoking status and total serum cholesterol. In the multivariate analysis adjusting for resting SBP, age, total serum cholesterol, smoking status and family history of CHD, there is a significant 51% increased risk of CV mortality in Q4 compared to Q1 (), and also significantly increased risk in Q3 compared to Q1, hazard ratio (HR) 1.35 (CI: 1.01–1.80). When adjusting for physical fitness in addition to the abovementioned classical CV risk factors, the HR for Q4 compared to Q1 is reduced to 1.39, though still borderline significantly increased (CI: 1.00–1.93, p = 0.05).
Table 2. Hazard Ratios of Cardiovascular Mortality in Quartiles of SBP100W at Baseline.
There was also a significant association between SBP100W and CV disease after 35 years of follow-up (p < 0.0001, ). Both when adjusting for age separately and in the multiple-adjusted model adjusting for age, systolic blood pressure at rest, total serum cholesterol, smoking status and family history of CHD, there was a significantly increased risk of CV disease in Q4 compared to Q1 (). When adding physical fitness into the multivariate model, the association is no longer statistically significant (p = 0.11).
Figure 3. Kaplan-Meier plot showing cardiovascular disease in 1999 participants divided in quartiles of SBP100W and followed-up for 35 years. Cardiovascular disease includes peripheral artery disease, abdominal aortic aneurysm, claudicatio intermittens, fatal or non-fatal cerebral stroke, transitory ischaemic attack, angina pectoris, fatal or non-fatal myocardial infarction and heart failure. SBP100W: Peak systolic blood pressure at 100 W workload; CV: cardiovascular.
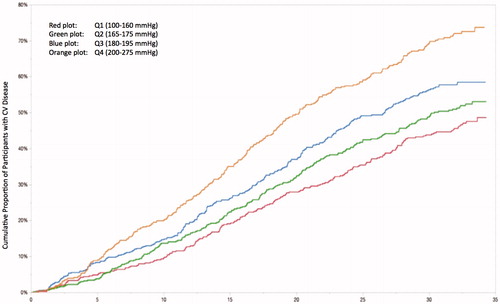
Table 3. Hazard Ratios of Cardiovascular Disease in Quartiles of SBP100W at Baseline.
Discussion
In the present study, we investigated exercise SBP in prediction of future CV disease and mortality. Our results show a significant association between exercise SBP at moderate workload and CV disease and mortality through 35 years of follow-up in a cohort of healthy, middle-aged, Caucasian men. The predictive value of SBP100W is independent of both classical CV risk factors and physical fitness combined, suggesting exercise SBP to be an independent predictor of CV mortality.
The finding of a significant association between exercise SBP and CV mortality is consistent with our previous findings from this cohort and a recent review and meta-analysis regarding exercise SBP [Citation3]. It is our opinion that increased exercise SBP should be regarded as a consistent and reliable predictor for CV mortality. In the multivariate analysis excluding physical fitness, there is also significantly increased risk in Q3 compared to Q1. This indicates an increase in risk of CV mortality with exercise SBP >180 mm Hg at moderate workload. We have previously presented data indicating 190 mm Hg to be a threshold for exercise blood pressure [Citation13]. With further analyses in this study, using quartile grouping instead of a fixed threshold, we have revealed even lower thresholds for CV risk.
Regarding CV disease, fatal or non-fatal, there is a significantly increased risk with increasing SBP100W. The association regarding CV disease is not as strong as regarding CV mortality and the results did not reach statistical significance in the multivariate analysis including physical fitness. Still, the results of this study indicate that exercise SBP at moderate workload predicts CV disease, independent of the classical CV risk factors. One reason explaining the different predictive power of SBP100W regarding CV mortality and CV disease might be that the latter group contains “softer” endpoints as angina pectoris and claudicatio intermittens, possibly diluting the results. It is also possible that exercise SBP is a more potent inducer of atherosclerosis in coronary and cerebral arteries, favouring CV mortality rather than CV disease including peripheral artery disease.
In the present study, physical fitness has been included in the multivariate analyses, although being a quite unusual parameter to make adjustments for in epidemiological analyses. When performing exercise tests, participants have different physical capacity, and even though the blood pressure was registered at moderate workload, the workload represent a part of the participant’s total capacity, which is the rationale for performing adjustments for physical fitness.
Physiology and Pathophysiology
During exercise, an increase in SBP is considered to be a physiological response. This is due to the increase in cardiac output needed to meet the metabolic demands of the exercising muscles, and SBP increases with increasing workload. Why some individuals show an exaggerated SBP during exercise is not fully understood. The aetiology is most likely of vascular origin rather than due to left ventricular hypertrophy and dysfunction, as often seen in exercise-induced hypotension [Citation14]. Insufficient reduction in total peripheral resistance due to failing vascular properties or endothelial dysfunction has been proposed [Citation14–16]. The same exercise protocol as in the present study was used in another study, showing a significantly higher total peripheral vascular resistance in men with exercise SBP ≥200 mm Hg [Citation16].
It is not possible to determine the pathophysiological mechanism for the association between systolic blood pressure at moderate workload (SBP100W) and CV disease and mortality in our epidemiological study. Therefore, exaggerated SBP response on exercise might act as a marker for a yet unknown, or possibly known [Citation16], but not acknowledged risk factor for CV disease and mortality. Exaggerated blood pressure during exercise tests has been suggested to correlate to blood pressure responses during physical stress in daily life [Citation17] and by this also to be associated with increased risk of future CV disease not covered by recommended resting blood pressure measurements after five minutes of rest in supine or sitting position, e.g. masked hypertension. Masked hypertension has also been associated with exaggerated SBP response to both maximal- or moderate intensity exercise, which might explain the increased risk of CV mortality [Citation18]. Consequently, SBP at moderate workload might represent a stressor revealing failing compensatory mechanisms not discovered under standardised, resting conditions. Even though 100 W is to be considered as a moderate workload, the shifting from rest to exercise without a more gradual increase in workload may enhance the effect on blood pressure response. If so, an exaggerated SBP response to exercise should be regarded as a marker of disease rather than a risk factor for developing disease, as have been emphasised earlier [Citation6].
Variation and Reproducibility of Exercise Blood Pressure
During the bicycle test, peak SBP was measured. If exercise SBP is correlated to CV disease and mortality, it is reasonable to believe that SBP on maximal workload would have an impact on risk prediction. In our study, none of the results of the analyses are altered by SBP on maximal workload (data not shown), and SBP on moderate workload seems to be independent from this potential predictor. This is consistent with other studies, both from this cohort and other studies investigating exercise SBP [Citation3,Citation7]. One might speculate on why SBP on maximal workload is cancelled out by other predictors. One reason is that maximal SBP is dependent on duration and workload of exercise. This is to a great extent depending on how much effort each participant puts into the test, which is based on subjective qualities differing between participants. In addition to difficulties reaching the proper workload representing maximal workload, greater effort might cause greater movement artefacts and disturbances which could result in unreliable values, at least when using a non-invasive method as in this study. Diastolic blood pressure or pulse pressure is not investigated in this study due to difficulties obtaining reliable results in an exercise setting with non-invasive measurements.
Because maximum exercise capacity differs between participants, adjustment for physical fitness, in addition to the classical CV risk factors is important. Although 100 W is considered to be a moderate workload, some participants may show a physiologically increased SBP due to being closer to their maximum exercise capacity. This is reflected by the alterations in the results when introducing physical fitness in the multivariate model. Adjustments for physical fitness thus strengthen SBP100W as a predictor for CV mortality.
Importantly, within two weeks of the first exercise test, the test was repeated in 130 of the participants. Blood pressures, heart rates and working capacities in the two tests were within ±5% in 90% of the participants and within ±10% in all of the men [Citation5]. This indicates excellent reproducibility of exercise SBP with this protocol, strongly suggesting that the protocol is reliable.
Clinical Aspects of Exercise Blood Pressure
There is no agreement on what should be considered to be an exaggerated SBP response to exercise and the threshold values have only been arbitrarily defined [Citation14]. Some studies have used the 90th or 95th percentile, or SBP ≥210 mm Hg for men and SBP ≥190 mm Hg for women [Citation19–21]. Based on the findings in our study, a larger population of participants might have an increased risk of CV disease and mortality than earlier acknowledged by using the arbitrarily defined limits described above.
Exercise SBP measurements are of uncertain clinical importance until threshold values for exercise SBP are defined. It is not known if intervention alters outcome in individuals with hypertensive response to exercise [Citation17]. Still, with the predictive power of exercise SBP, it might be used in the overall risk assessment of individuals and in the future help clinicians decide which individuals who would benefit from regular examinations and intervention, whether invasive, pharmacological or lifestyle interventions.
This study was performed on healthy, middle-aged individuals without any chronic drug treatment. However, in a clinical setting, patients often have CV co-morbidity or primary prevention treatment, and further research will be needed to strengthen the predictive value of exercise blood pressure in this group.
Limitations
In our study, we have investigated the SBP response to moderate workload in a population of healthy, middle-aged, Caucasian men. Our results cannot necessarily be used in the risk assessment of women, neither in men of another descent. Still, our opinion is that exercise SBP might predict future CV risk not specific for healthy Caucasians.
For blood pressure measurements in our study, a non-invasive method was used. This method is less accurate than invasive methods. Precise results are also more difficult to obtain with non-invasive methods during exercise than in supine or sitting position. However, if exercise SBP measurements are to be used in the routine assessments in outpatient clinics, a non-invasive method with the patient sitting on a bicycle or walking on a treadmill is the only feasible method.
In modern epidemiology, the concept of “competing risk” has gained increased attention. However, as analyses on competing risk have previously been performed on the same cohort and been found to have only minor impact on the results [Citation22], such analyses were not considered needed in the present study.
Conclusions
In this long-term cohort study, systolic blood pressure at moderate workload was investigated as a predictor for cardiovascular disease and mortality in healthy middle-aged men. The results of this study suggest that an exaggerated SBP response at moderate workload is, independently of other important risk factors, associated with increased risk of cardiovascular disease and mortality that extends through as long as 35 years and into old ages.
Perspectives
The result of our 35-year follow-up indicates an independent association between SBP100W and CV mortality. This is in line with the current assumptions regarding exercise SBP. The present study indicates a sustained increase in risk of CV events beyond 21 years of follow-up. The novelty of this study is the sustained risk of CV mortality after 35 years, and also the increased CV risk already from 180 mm Hg.
| Abbreviations | ||
| CV | = | Cardiovascular |
| SBP | = | Systolic blood pressure |
| CHD | = | Coronary heart disease |
| SBP100W | = | Peak systolic blood pressure during six minutes of bicycling at a 100 W workload |
| ECG | = | Electrocardiography/electrocardiogram |
| Q | = | Quartile |
| W | = | Watts |
| CI | = | Confidence interval, 95% |
| HR | = | Hazard ratio |
Disclosure statement
Oslo Ischemia Study is supported by Oslo University Hospital, Ullevaal.
SE Kjeldsen has received honoraria from ABDiiBRAHiM, Bayer, MSD, and Takeda. J Bodegard holds a position as epidemiologist in AstraZeneca. The other authors report no conflict of interest.
References
- Filipovsky J, Ducimetiere P, Safar ME. Prognostic significance of exercise blood pressure and heart rate in middle-aged men. Hypertension. 1992;20:333–339.
- Weiss SA, Blumenthal RS, Sharrett AR, et al. Exercise blood pressure and future cardiovascular death in asymptomatic individuals. Circulation. 2010;121:2109–2116.
- Schultz MG, Otahal P, Cleland VJ, et al. Exercise-induced hypertension, cardiovascular events, and mortality in patients undergoing exercise stress testing: a systematic review and meta-analysis. Am J Hypertens. 2013;26:357–366.
- Fagard R, Staessen J, Thijs L, et al. Prognostic significance of exercise versus resting blood pressure in hypertensive men. Hypertension. 1991;17:574–578.
- Mundal R, Kjeldsen SE, Sandvik L, et al. Exercise blood pressure predicts cardiovascular mortality in middle-aged men. Hypertension. 1994;24:56–62.
- Mundal R, Kjeldsen SE, Sandvik L, et al. Exercise blood pressure predicts mortality from myocardial infarction. Hypertension. 1996;27:324–329.
- Kjeldsen SE, Mundal R, Sandvik L, et al. Supine and exercise systolic blood pressure predict cardiovascular death in middle-aged men. J Hypertens. 2001;19:1343–1348.
- Skretteberg PT, Grundvold I, Kjeldsen SE, et al. Seven-year increase in exercise systolic blood pressure at moderate workload predicts long-term risk of coronary heart disease and mortality in healthy middle-aged men. Hypertension. 2013;61:1134–1140.
- Skretteberg PT, Grundvold I, Kjeldsen SE, et al. Exercise systolic blood pressure at 100 watt predicts cardiovascular mortality in apparently healthy men; a 35-year follow-up study: 7b.02. J Hypertens. 2010;28:e405.
- Erikssen J, Enge I, Forfang K, et al. False positive diagnostic tests and coronary angiographic findings in 105 presumably healthy males. Circulation. 1976;54:371–376.
- Sandvik L, Erikssen J, Thaulow E, et al. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med. 1993;328:533–537.
- Mundal R, Kjeldsen SE, Sandvik L, et al. Clustering of coronary risk factors with increasing blood pressure at rest and during exercise. J Hypertens. 1998;16:19–22.
- Mariampillai JE, Engeseth K, Kjeldsen SE, et al. 2D.01: Exercise systolic blood pressure ≥190 mm Hg at moderate workload predicts coronary heart disease in healthy, middle-aged men. J Hypertens. 2015;33(Suppl 1):e28.
- Le VV, Mitiku T, Sungar G, et al. The blood pressure response to dynamic exercise testing: a systematic review. Prog Cardiovasc Dis. 2008;51:135–160.
- Chang HJ, Chung J, Choi SY, et al. Endothelial dysfunction in patients with exaggerated blood pressure response during treadmill test. Clin Cardiol. 2004;27:421–425.
- Fossum E, Høieggen A, Moan A, et al. Insulin sensitivity is related to physical fitness and exercise blood pressure to structural vascular properties in young men. Hypertension. 1999;33:781–786.
- Laukkanen JA, Kurl S. Blood pressure responses during exercise testing-is up best for prognosis? Ann Med. 2012;44:218–224.
- Sharman JE, Hare JL, Thomas S, et al. Association of masked hypertension and left ventricular remodeling with the hypertensive response to exercise. Am J Hypertens. 2011;24:898–903.
- Lauer MS, Levy D, Anderson KM, et al. Is there a relationship between exercise systolic blood pressure response and left ventricular mass? The Framingham Heart Study. Ann Intern Med. 1992;116:203–210.
- Lauer MS, Pashkow FJ, Harvey SA, et al. Angiographic and prognostic implications of an exaggerated exercise systolic blood pressure response and rest systolic blood pressure in adults undergoing evaluation for suspected coronary artery disease. J Am Coll Cardiol. 1995;26:1630–1636.
- Mottram PM, Haluska B, Yuda S, et al. Patients with a hypertensive response to exercise have impaired systolic function without diastolic dysfunction or left ventricular hypertrophy. J Am Coll Cardiol. 2004;43:848–853.
- Grundvold I, Skretteberg PT, Liestøl K, et al. Low heart rates predict incident atrial fibrillation in healthy middle-aged men. Circ Arrhythm Electrophysiol. 2013;6:726–731.