Abstract
Objectives: The association of temperature maintenance with blood pressure (BP) has not been studied and the association of temperature with season-related BP was not being well understood. The present study aims to be further aware of season-related BP variation in Chinese adults.
Methods: We used decoded data from adults who visited the hospital for health examination from January 2008 to November 2013. Multivariate regression models were used to analyses the association between outdoor temperature and BP.
Results: The analysis included 438,811 adults. Larger change of BP accompanied with unit change of average outdoor temperature among outpatient than inpatient patients. The association of temperature with BP was stronger in normotensives than that in hypertensives. Compared with temperature variation, the impact of temperature maintenance on BP was smaller. These associations were stronger in men, older individuals.
Conclusions: Temperature was strongly inversely associated with BP in Chinese adults. Temperature maintenance was mildly associated with BP compared to temperature variance. Seasonal temperature variation should be considered when screening for hypertension.
Introduction
Hypertension contributes one of the leading causes of cardiovascular diseases like heart disease, coronary artery disease and stroke. Raised blood pressure (BP) is a risk contributor for cardiovascular mortality and for coronary heart disease morbidity [Citation1–3]. Meteorological conditions, such as ambient average temperature and relative humidity, are suspected to be one of the factors influence BP levels. Previous studies have reported the short-term relationship between meteorological conditions, BP and adverse cardiovascular diseases and events [Citation4,Citation5].
Most studies have provided evidence of an inverse association of ambient temperature with high BP during the cold seasons [Citation6]. The fluctuation of BP is considered to be mediated by meteorological factors, especially by outdoor temperature. And a sudden exposure to cold environment causes increased BP in both normotensive and hypertensive subjects. A study in healthy adults in Beijing, China reported that decreasing temperature was associated with significantly increasing BP [Citation7]. Both hypertensive group and normotensive group had increased BP on account of cold exposure in a clinical trial [Citation8]. At the same time, the seasonal variation was not only observed for clinic BP, but also found in home BP [Citation9]. A population-based longitudinal study with subjects older than 65 years found that outdoor temperature was strongly correlated with clinic BP [Citation10]. A study with men aged 53–100 years found modest association between clinic diastolic blood pressure (DBP) and temperature [Citation11]. Taking account of using heat system, studies reported an inverse association between outside temperature and home BP only in warm seasons [Citation6,Citation9]. These effects of temperature on BP were stronger among those with older age, female sex in elderly hypertensive patients in a longitudinal study in Shanghai, China [Citation12].
Previous studies have focused on the estimated effects of temperature on BP and seasonal variations of blood pressure-related diseases. Nevertheless, studies simply revealed the fluctuation of BP in seasons, while BP variations in different seasons were not mentioned. Other than temperature fluctuations, sustained high or low temperature may influence BP changes. To our knowledge, there are no previous studies focused on the influence of temperature maintenance on BP. The objective of this study was to discuss and to further understand the association of daily average temperature and temperature maintenance between day to day with both systolic blood pressure (SBP) and DBP in health examination adults in China.
Methods
Study population
Zhejiang is a relatively prosperous province with a population of 54 million according to the Sixth National Population Census. Hangzhou is the capital of Zhejiang province located at northern latitude 30° and it is the economic, cultural, science and educational center of Zhejiang province. Hangzhou is characterized by a subtropical monsoon climate, featuring distinct seasons, ample sunlight and rainfall. This study was conducted in the Second Affiliated Hospital of Zhejiang University School of Medicine (Hangzhou, Zhejiang Province, China). It is a comprehensive and tertiary care hospital with high quality of medical treatment, scientific research and teaching.
The decoded dataset of health examination included people above 18 years who visited the hospital for health examination from January 2008 to November 2013. From the decoded dataset, we extracted the data about patients’ gender, age, height, weight, health examination type (inpatient health examination and outpatient health examination), health examination date and BP. The study was approved by the Medical Ethical Committee of Zhejiang University School of Medicine.
Physiological measurements
Body weight (kg) and height (cm) were measured according to the standard procedures. Body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2). A validated automated oscillometric BP monitor, type Omron HBP-9020 was used to obtain BP measurements. The measurement was preformed after at least 5 minutes of rest in a seated position.
Meteorological data
Daily ambient average temperature and average relative humidity were monitored at Hangzhou meteorological station and were obtained from the Hangzhou Meteorological Administration. Data from January 2008 to September 2015 were extracted to cover dataset period. We used only Hangzhou temperature measurement site for our analyses.
Statistical analysis
According to age, subjects were grouped into <50 years and ≥50 years. Furthermore, subjects were classified into either a group with normotensive (SBP <140 mmHg and DBP <90 mmHg) or a group with hypertensive (SBP ≥140 mmHg or DBP ≥90 mmHg). Given that indoor heat system and air condition system might reduce the effect of seasonal variation on BP levels, subjects were classified into inpatient health examination and outpatient health examination according to health examination type. The season for health examination date was classified as follows: spring (March to May), summer (June to August), autumn (September to November) and winter (December to February). Considering the effects of interaction between temperature and humidity, we created z scores for BP (standardized by average humidity or average temperature). BP standardized by average humidity was calculated as standardized by the integer value of average humidity. BP standardized by average temperature was calculated as standardized by average Celsius degree. Given that temperature maintenance might have an influence on the fluctuation of BP, we took number of days for variation of average temperature between day to day into the model. For example, first we defined temperature variation as if temperature change were within −0.1 °C to 0.1 °C, then we calculated temperature difference between every two days. If the value were within the scope, then we counted the number of lasing days as temperature maintenance. We calculated in Java language in Eclipse, version 4.5.0. The association of variation temperature ranging from 0.1 °C to 3 °C with BP is largest as variation temperature was below 0.6 °C, so we used temperature below 0.6 °C to calculate the number of days for variation of average temperature. By establishing model, we used interaction term to test if average temperature had different effects on BP in different seasons and groups. In order to compare the differences among associations of temperature with BP in same models across different groups, we made dummy variables and also created interaction terms between dummy variables and response variables into one model.
Descriptive statistics were used to characterize study samples and meteorological factors in different seasons. Comparisons of demographic characteristics in different seasons were conducted with Chi Square test. One-way analysis of variance (ANOVA) was used for comparing the continuous variables in different groups. Associations of variables and BP were examined by multivariate linear regression model with adjustment of age, gender and BMI. We treated all statistical analyses with SAS, version 9.4 (SAS Inc., Cary, NC, USA). A P value below .05 was considered statistical significance.
Results
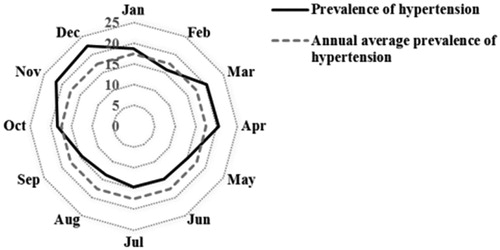
A description of sociodemographic characteristics of the participants was showed in . Both SBP and DBP differed significantly across four seasons, with higher values in spring and winter than that in summer and autumn. In total population, significantly inverse associations were observed between outdoor average temperature, average relative humidity with SBP and DBP. But the association was weaker between temperature maintenance with SBP and DBP when compared with average temperature (). The effect of temperature on BP was higher in spring and autumn than that in summer and winter. In summer, outdoor average temperature did not significantly associate with SBP, and average relative humidity was not significantly associated with DBP. Temperature maintenance was significantly associated with SBP in summer and autumn, and was significantly associated with DBP in autumn (). When average temperature was below 10 °C and above 25 °C, standardized BP decreased slowly with temperature. However, when temperature ranging from about 10 °C to 25 °C, standardized BP decreased sharply with average temperature (). BP standardized by average temperature decreased with average relative humidity when average humidity was below 50%, then stayed stable as humidity increased (). Winter season had highest prevalence of hypertension compared with annual average prevalence (). Compared to winter, significant associations of temperature on BP were found in spring, summer and autumn in total population (Supplementary Table S5).
Figure 1. (a) The association of average temperature with blood pressure standardized by average humidity; (b) The association of average humidity with blood pressure standardized by average temperature; The association of average temperature with blood pressure among total population standardized by average humidity stratified by gender (c), age group (d) and health examination type (e).
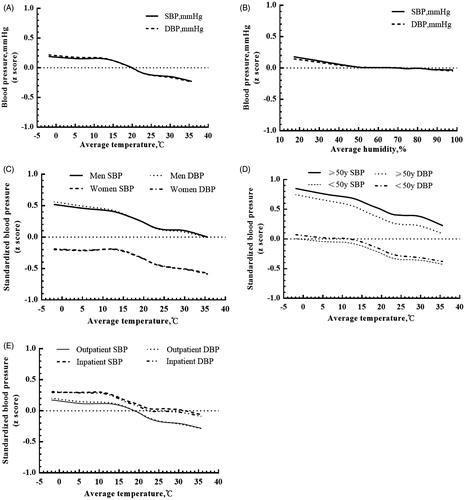
Table 1. Distribution of sociodemographic characteristics among population taking health examination by season.
Table 2. AdjustedTable Footnotea association of temperature and humidity with blood pressure.
Table 3. AdjustedTable Footnotea association of temperature and humidity with blood pressure among total population stratified by season.
In population with normotensive, average outdoor temperature and relative humidity were adversely significantly associated with SBP and DBP (). The association of average temperature with SBP and DBP in spring and autumn were stronger than that in summer and winter. Significant association between temperature maintenance with SBP was observed in autumn and winter, while significant association between temperature maintenance with DBP was observed in winter (Supplementary Table S3). Statistically significant associations of average temperature with BP were found in spring and autumn compared with winter in normotensives (Supplementary Table S6). In hypertensive subjects, the association with temperature and SBP was greater in spring and winter than that in summer and autumn, while the association with DBP was greater in spring and autumn than that in summer and winter. However, average temperature had no statistically significant association with SBP in summer. No statistically significant associations of temperature maintenance were found with BP in hypertensive patients (Supplementary Table S4). Associations of average temperature with SBP in summer as well as DBP in spring were significant compared to that in winter(Supplementary Table S6).
The results stratified by gender, age and visiting type were similar to those in the whole sample. Effects of temperature on BP were showed significantly stronger effects in population with men sex, age above 50 years old, and outpatient health examination than reference groups (). Significant associations of temperature on BP in four seasons were found in outpatient subjects. No statistically significant associations were found in summer in inpatient health examination subjects (). Average temperature varied with SBP/DBP when stratified by gender, age and visiting type. From 10 °C to 25 °C, the trend of standardized BP was changed, while the overall trends were similar (). The association of temperature with BP was significant when stratified by gender (Supplementary Table S1, S2). We used BP standardized by average humidity replaced the original BP as outcome variable in above analyses, the results did not obviously change (data not shown). There were significant differences in four seasons in men. However, DBP in summer was not significant compared to that in winter in women (Supplementary Table S7). The association of average temperature with BP in different gender, age, visiting type, hypertensive or normotensive were statistically significant(Supplementary Table S8).
Table 4. AdjustedTable Footnotea association of temperature with blood pressure in four seasons in inpatient and outpatient health examination.
Discussion
The results of this study showed that there was a seasonal variation with BP. Temperature in spring and autumn exerted more effects on BP than that in summer and winter. Temperature variance had larger impacts on BP than temperature maintenance. Larger change of BP accompanied with unit change of average outdoor temperature among outpatient than inpatient patients. The association of average temperature on BP was stronger in normotensive people than that in hypertensives. These associations were stronger in men, older individuals.
If temperature has interactive effects with season, then temperature in four seasons might have different effects on BP. The effects of season-related temperature on BP would be different at same temperature in four seasons. Our results showed that there was different BP fluctuation in different seasons, and BP was higher in winter than that in other seasons. Similar to our findings, several studies have reported that individuals’ BP was higher in cold seasons than that in warm seasons. Madsen et al. [Citation13] reported daily temperature was inversely related to BP in a population of 18,770 Oslo citizen. A national cohort of blacks and whites found significantly inverse association between outdoor temperature and BP after adjusted for various confounders [Citation14]. A study enrolled in normotensive volunteers in Greenland demonstrated a clear dose-response relationship between low temperature and high SBP/DBP [Citation15]. A longitudinal study in hypertensive patients followed up for three years showed an inverse association between ambient temperature with BP [Citation16]. While Hozawa et al. reported an inverse association of outdoor temperature with home BP only in warm seasons in Japan [Citation9], which might because of using of heating system at home in winter seasons. Our results also demonstrated that the prevalence of hypertension incidence is much higher during winter seasons as well as in March and April. Cold environments and large temperature differences between day to day in spring could potentially lead to a rise in BP.
Temperature affecting the change in BP includes several mechanisms. Cold temperatures provoke a range of physiological reaction and increase the activities of the sympathetic nervous system as well as renin-angiotensin system [Citation17]. At the same time, the sympathetic nervous system may secrete catecholamine and initiate cold-induced hypertension through the renin-angiotensin system [Citation18]. Moreover, sodium losing with profuse sweating in summer may lead to lower BP values. The present study found that temperature variance in spring and autumn had great impacts on BP, it might because temperature fluctuation in spring and autumn is larger than that in summer and winter. When people are exposed to continuous high and low temperature in summer and winter, the body may adapt to the changes in environments.
Sega et al. [Citation19] found seasonal clinical BP patterns were similar for normotensive subjects and hypertensives, we found similar patterns. However, the results of temperature associated with BP fluctuation in normotensive subjects are inconsistent. As with Hayashi et al. and Sinha et al. [Citation20,Citation21] our study also had reported seasonal variations in normotensives. Nevertheless, a prospective study of borderline hypertensive patients revealed small irrelevant between winter and summer [Citation22], which might because borderline hypertensives took an intermediate status between normotensives and hypertensives. Our analysis suggested that the impact of average temperature on SBP was greater than DBP in population with normotensive. This finding was in line with Jansen et al. and Askari et al., who reported SBP had a greater seasonal variation compared to DBP [Citation15,Citation23]. From another aspect, we found that ambient temperature had a relative smaller effect on BP in hypertensive patients. Study in hypertensive patients in a stable environment temperature showed that BP in the morning and night were significant higher in winter than that in summer, and there was no correlation between the seasonal change in BP in the morning and that at night [Citation24].
The effect of gender difference on the reaction of BP seems controversial. Our findings showed that men experienced greater reaction on BP-temperature association, which were consisted with some studies [Citation25]. While Srivastava et al. [Citation26] detected that women were more sensitive to cold than men, and Barnett et al. [Citation27] suggested increased temperature had stronger effects in women than that in men. Further researches confirmation is needed. Some researchers had reported that older people’s BP is more sensitive to temperature variation [Citation28]. We also found older people might be more sensitive with cold and heat exposures than younger people. This might partly due to comparing with younger people; older people have poorer vasoconstrictor response to cold environment, which leads to heat loss [Citation29].
The effects of temperature maintenance on BP were not reported in previous studies. We did not find temperature maintenance had great associations with BP as we expected. We only observed temperature maintenance had little impacts on BP in normotensive subjects in winter and had no effect on hypertensive patients. The results showed that temperature maintenance had less impact on BP compared with average temperature and average humidity. We found that average relative humidity was barely associated with BP. Our results revealed that on average, SBP was 0.0145 mmHg and DBP was 0.0113 mmHg lower per 1% increasing in average relative humidity. A longitudinal study in 100,000 healthy individuals showed that relative humidity was only minimally associated with DBP after adjustment for mean daily temperature [Citation30]. A study consisted of men aged 50–100 showed that no association was found between average relative humidity and BP [Citation11]. Study in 10 diverse regions of China found that the associations of BP with season and outdoor temperature were not modified by outdoor relative humidity [Citation6].
Our study extends previous findings on temperature and BP. Our analysis was performed on a large number of individuals with inpatient health examination and outpatient health examination. And the present study first evaluated the effects of temperature maintenance on BP. At the same time, when sub-analyses were conducted in different groups, the results remained stable. One limitation of our study was that we didn’t obtain information of hypertension control and treatment, which might cause misclassification bias. However, the results would be more apparent when eliminated the bias.
In conclusion, we found average temperature was inversely associated with BP in Chinese adults. These results suggest that temperature has different effect on season-related BP in population with inpatients and outpatients, normotensive and hypertensive. Temperature variation has a greater impact on BP than temperature maintenance. Seasonal variation should be taken account when monitoring BP.
Yu_et_al._supplemental_content.doc
Download MS Word (185 KB)Acknowledgements
We acknowledge the assistance and cooperation of the faculty and staff of The Second Affiliated Hospital Zhejiang University School of Medicine and Hangzhou Meteorological Bureau. This study was supported by the Natural Science Foundation of Zhejiang Province in China (Grant No.: LY14H260003).
Disclosure statement
There are no conflicts of interest.
Additional information
Funding
References
- Shiue I, Shiue M. Indoor temperature below 18 degrees C accounts for 9% population attributable risk for high blood pressure in Scotland. Int J Cardiol. 2014;171:e1–e2.
- Gu Q, Burt VL, Paulose-Ram R, et al. High blood pressure and cardiovascular disease mortality risk among U.S. adults: the third National Health and Nutrition Examination Survey mortality follow-up study. Ann Epidemiol. 2008;18:302–309.
- Kannel WB, Schwartz MJ, McNamara PM. Blood pressure and risk of coronary heart disease: the Framingham study. Dis Chest. 1969;56:43–52.
- Guo Y, Li S, Zhang Y, et al. Extremely cold and hot temperatures increase the risk of ischaemic heart disease mortality: epidemiological evidence from China. Heart. 2013;99:195–203.
- Michelozzi P, De Sario M. Temperature changes and the risk of cardiac events. BMJ. 2010;341:c3720.
- Lewington S, Li L, Sherliker P, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens. 2012;30:1383–1391.
- Wu S, Deng F, Huang J, et al. Does ambient temperature interact with air pollution to alter blood pressure? A repeated-measure study in healthy adults. J Hypertens. 2015;33:2414–2421.
- Komulainen S, Tahtinen T, Rintamaki H, et al. Blood pressure responses to whole-body cold exposure: effect of carvedilol. Eur J Clin Pharmacol. 2000;56:637–642.
- Hozawa A, Kuriyama S, Shimazu T, et al. Seasonal variation in home blood pressure measurements and relation to outside temperature in Japan. Clin Exp Hypertens. 2011;33:153–158.
- Alperovitch A, Lacombe JM, Hanon O, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch Intern Med. 2009;169:75–80.
- Halonen JI, Zanobetti A, Sparrow D, et al. Relationship between outdoor temperature and blood pressure. Occup Environ Med. 2011;68:296–301.
- Chen R, Lu J, Yu Q, et al. The acute effects of outdoor temperature on blood pressure in a panel of elderly hypertensive patients. Int J Biometeorol. 2015;59:1791–1797.
- Madsen C, Nafstad P. Associations between environmental exposure and blood pressure among participants in the Oslo Health Study (HUBRO). Eur J Epidemiol. 2006;21:485–491.
- Kent ST, Howard G, Crosson WL, et al. The association of remotely-sensed outdoor temperature with blood pressure levels in REGARDS: a cross-sectional study of a large, national cohort of African-American and white participants. Environ Health. 2011;10:7.
- Jansen PM, Leineweber MJ, Thien T. The effect of a change in ambient temperature on blood pressure in normotensives. J Hum Hypertens. 2001;15:113–117.
- Chen Q, Wang J, Tian J, et al. Association between ambient temperature and blood pressure and blood pressure regulators: 1831 hypertensive patients followed up for three years. PLoS One. 2013;8:e84522.
- Cuspidi C, Ochoa JE, Parati G. Seasonal variations in blood pressure: a complex phenomenon. J Hypertens. 2012;30:1315–1320.
- Sun Z. Cardiovascular responses to cold exposure. Front Biosci (Elite Ed). 2010;2:495–503.
- Sega R, Cesana G, Bombelli M, et al. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arteriose Monitorate E Loro Associazioni. J Hypertens. 1998;16:1585–1592.
- Sinha P, Kumar TD, Singh NP, et al. Seasonal variation of blood pressure in normotensive females aged 18 to 40 years in an urban slum of Delhi, India. Asia Pac J Public Health. 2010;22:134–145.
- Hayashi T, Ohshige K, Sawai A, et al. Seasonal influence on blood pressure in elderly normotensive subjects. Hypertens Res. 2008;31:569–574.
- Brueren MM, Schouten BJ, Schouten HJ, et al. No relevant seasonal influences on office and ambulatory blood pressure: data from a study in borderline hypertensive primary care patients. Am J Hypertens. 1998;11:602–605.
- Askari S, Asghari G, Ghanbarian A, et al. Seasonal variations of blood pressure in adults: Tehran lipid and glucose study. Arch Iran Med. 2014;17:441–443.
- Fujiwara T, Kawamura M, Nakajima J, et al. Seasonal differences in diurnal blood pressure of hypertensive patients living in a stable environmental temperature. J Hypertens. 1995;13:1747–1752.
- Lanzinger S, Hampel R, Breitner S, et al. Short-term effects of air temperature on blood pressure and pulse pressure in potentially susceptible individuals. Int J Hyg Environ Health. 2014;217:775–784.
- Srivastava RD, Kumar M, Shinghal R, et al. Influence of age and gender on cold pressor response in Indian population. Indian J Physiol Pharmacol. 2010;54:174–178.
- Barnett AG, Sans S, Salomaa V, et al. The effect of temperature on systolic blood pressure. Blood Press Monit. 2007;12:195–203.
- Kingma BR, Frijns AJ, Saris WH, et al. Increased systolic blood pressure after mild cold and rewarming: relation to cold-induced thermogenesis and age. Acta Physiol (Oxf). 2011;203:419–427.
- Kenney WL, Armstrong CG. Reflex peripheral vasoconstriction is diminished in older men. J Appl Physiol (1985). 1996;80:512–515.
- van den Hurk K, de Kort WL, Deinum J, et al. Higher outdoor temperatures are progressively associated with lower blood pressure: a longitudinal study in 100,000 healthy individuals. J Am Soc Hypertens. 2015;9:536–543.