Abstract
Objective: To determine the clinical profile and blood pressure (BP) control rates of anticoagulated patients with hypertension and atrial fibrillation (AF).
Methods: The PAULA study was a multicenter cross-sectional/retrospective observational study conducted throughout Spain. The study included patients with nonvalvular AF who were receiving vitamin K antagonist therapy during the past year and were attended at primary care setting. Adequate BP control was defined according to 2013 ESC/ESH guidelines.
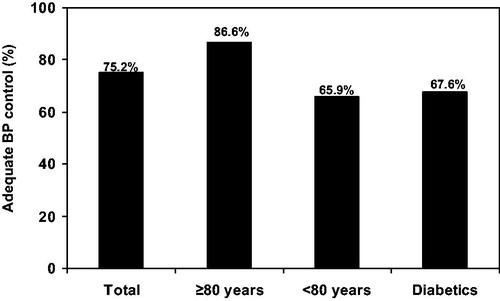
Results: A total of 1,222 hypertensive patients were included (mean age 77.9 ± 8.3 years; 51.2% women; CHADS2 2.5 ± 1.1; CHA2DS2-VASc 4.2 ± 1.4; HAS-BLED 1.6 ± 0.9). 33.5% of patients had diabetes, 24.9% heart failure and 14.0% prior stroke/transient ischemic attack. Mean BP was 131.4 ± 14.5/74.9 ± 9.8 mm Hg. With regard to antihypertensive treatment, most of patients were on combined therapy (67.9%). The commonest prescribed antihypertensive drugs were diuretics (64.4%), followed by angiotensin receptor blockers (30.1%), and beta blockers (29.4%). 75.2% of hypertensive patients achieved BP control targets; 86.6% of patients ≥80 years and 67.6% of diabetics.
Conclusions: More than 75% of hypertensive patients with AF achieved BP goals, and this rate was higher in elderly. More than 2 thirds of patients were on combined therapy. BP control appears to be better in AF patients than in general hypertensive population.
Introduction
It has been estimated the current prevalence of atrial fibrillation (AF) is around 3% [Citation1]. Overall, AF is associated with an increased risk of stroke [Citation1]. The great majority of patients with AF require anticoagulant therapy to reduce the risk of thromboembolic complications [Citation2].
Hypertension is very common in patients with AF [Citation2–4] Hypertension promotes structural and functional changes in the heart facilitating the development of AF. Therefore, hypertension increases not only the risk of developing new-onset AF but the progression to permanent AF as well [Citation5,Citation6]. In addition, hypertension increases the risk of stroke in overall population, but more markedly in patients with AF. As a result, hypertension has a cumulative effect on the risk of stroke in AF patients [Citation7,Citation8].
To reduce the risk of stroke in AF patients with hypertension is important not only to assure a good anticoagulation control, but also a good blood pressure (BP) control. With regard to anticoagulation, post hoc analyses of pivotal clinical trials involving the use of direct oral anticoagulants compared with warfarin have shown that the beneficial effect of anticoagulation is independent of the presence of hypertension [Citation9–11]. Concerning hypertension, many studies have demonstrated that achieving BP goals to recommended targets reduces the risk of stroke, including patients with AF [Citation12]. However, the current available information about BP control rates in anticoagulated patients with AF in clinical practice is very scarce.
The PAULA (Perspectiva Actual de la sitUación de la anticoaguLaciónen la prácticacínica de Atenciónprimaria [Current perspective of anticoagulation in clinical practice in the primary care setting]) study was aimed to analyze the anticoagulation control rates in patients with nonvalvular AF who were on vitamin K antagonists during one year or more in primary care setting throughout Spain [Citation3]. The subset of hypertensive patients included in the PAULA study is examined in this paper, aimed to define the clinical profile and the BP control rates of this very high-risk hypertensive population.
Methods
The methodology of this study has been previously published [Citation3]. Briefly, it was an observational cross-sectional/retrospective, multicenter study, in which patients 18 years or older, with nonvalvular AF and anticoagulated with vitamin K antagonists for at least 12 months, and with >80% of INR values available from the last year, were included. The study was performed at primary care setting under clinical practice conditions. The patients were recruited between February and June 2014. The study was approved by the Clinical Research Ethics Committee of the University Hospital La Paz in Madrid. All patients signed a written informed consent before inclusion [Citation3].
The study was based on a single visit coinciding with one of the patient’s regular follow-up visits. The data were collected from the medical history and usual care with an on-site physician interview, and no study-specific diagnostic or therapeutic intervention. The data were entered in an electronic case report form, specifically developed for this study [Citation3].
Sociodemographic data, cardiovascular risk factors, history of cardiovascular disease, physical examination with BP and heart rate, full information on anticoagulant therapy with total weekly dose and INR values, concomitant therapies, and CHADS2, CHA2DS2-VASc, and HAS-BLED scores were recorded [Citation1,Citation3]. To assess patients’ INR control, the time within therapeutic range in the past 12 months was calculated at a centralized site by both the so called direct method (percent time with INR values within therapeutic range) and by the Rosendaal method [Citation13].
Adequate BP control was defined according to the 2013 European Society of Hypertension/European Society of Cardiology guidelines, what means in general population a BP <140/90 mm Hg; in diabetics BP <140/85 mm Hg; and in patients aged 80 years or older BP <150/90 mm Hg [Citation12].
Statistical analysis
Quantitative variables were described with measures of central tendency and dispersion (mean and standard deviation) and qualitative variables were described as absolute (number) and relative (%) frequencies. In the bivariate analysis to compare 2 means, parametric (Student t test) or nonparametric (Mann–Whitney U test) statistical tests were performed based on the sample distribution; to compare percentages, the chi-square test or Fisher test was used, according to sample size. A p value <.05 was considered significant. All analyses were performed using SPSS version 18, Data Entry.
Results
A total of 139 investigators from 99 health care centers located throughout all the Spanish territory included 1,524 patients, of whom 1,222 (80.2%) had hypertension.
In the subgroup of patients with arterial hypertension the mean age was 77.9 ± 8.3 years and 51.2% were women. Mean CHADS2 score was 2.5 ± 1.1, mean CHA2DS2-VASc score 4.2 ± 1.4, and mean HAS-BLED score 1.6 ± 0.9. With regard to associated morbidities, 33.5% of patients had diabetes mellitus, 24.9% heart failure, and 14.0% prior stroke or transient ischemic attack. With respect to the physical examination, mean systolic BP was 131.4 ± 14.5 mmHg, mean diastolic BP 74.9 ± 9.8 mm Hg and mean heart rate 73.3 ± 11.7 bpm. Compared with patients without hypertension, those hypertensive patients were older, had a higher body mass index and thromboembolic/bleeding risk, and had more commonly dyslipidemia, diabetes, heart failure, prior myocardial infarction, and renal insufficiency (). INR control rates were independent of the presence of history of hypertension.
Table 1. Clinical characteristics of the study population according to the presence of hypertension.
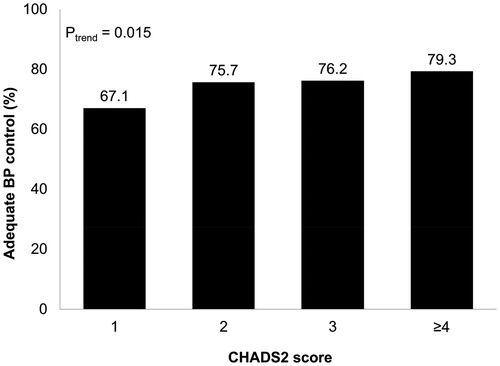
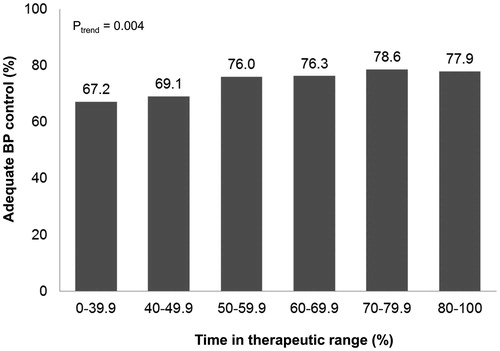
Data of the antihypertensive treatment in patients with hypertension were shown in . The majority of patients were treated with combined therapy (67.9%). The commonest prescribed antihypertensive drugs were diuretics (64.4%), followed by angiotensin receptor blockers (30.1%), beta blockers (29.4%) and angiotensin-converting enzyme inhibitors (28.7%). 75.2% of the overall hypertensive population achieved BP targets; 86.6% of patients aged 80 years or older and 67.6% of diabetics (). BP control rates according to CHADS2 score were shown in . For every increase in CHADS2 score, BP control rates improved by 3.1% (95% confidence interval 0.5–5.7%; P for trend =0.015). BP control rates according to time in therapeutic range (direct method) were shown in . For every 10% increase in time in therapeutic range, BP control rates improved by 2.0% (95% confidence interval 0.8–3.2%; P for trend = .004).
Table 2. Antihypertensive treatment in hypertensive patients.
Discussion
AF patients with hypertension have a worse clinical profile and a higher thromboembolic risk than AF patients without hypertension. In fact, the presence of other cardiovascular risk factors or cardiovascular diseases is very common in patients with hypertension and AF. Therefore, these patients are at very high risk, and not only for the development of stroke but also for myocardial infarction and cardiovascular death [Citation9]. In our study, patients had a high risk of stroke (CHADS2 score 2.5, CHA2DS2-VASc score 4.2), and a low risk of bleeding (HAS-BLED score 1.6). Thus, although uncontrolled BP increases the risk of bleeding, unless contraindicated, patients with AF and hypertension should receive chronic oral anticoagulation. Nonetheless, achieving BP goals with antihypertensive therapy is mandatory to reduce the risk of life-threatening bleeding [Citation1,Citation12].
Phase III clinical trials involving direct oral anticoagulants have analyzed the consequences of having high BP levels. In the ARISTOTLE (the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial, 87.5% of patients had a history of hypertension requiring treatment. High BP levels at any moment along the study was independently associated with a substantially higher risk of stroke or systemic embolism (Hazard Ratio [HR] 1.53; 95% confidence interval [CI] 1.25–1.86) as well as hemorrhagic stroke (HR 1.85; 95% CI 1.26–2.72) [Citation10]. In the ROCKET-AF (Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation) study, 90.5% of patients had hypertension (34.6% uncontrolled). The adjusted risk of stroke or systemic embolism significantly increased for every 10mm Hg in screening systolic BP (HR 1.07; 95% CI 1.02–1.13). There was a trend towards an increased risk of stroke or systemic embolism in patients with uncontrolled hypertension compared to those subjects with controlled BP [Citation11].
These results have been also confirmed in observational studies. Thus, data from the J-RHYTHM Registry suggest that BP control seems more important than the history of hypertension at preventing thromboembolism and major hemorrhage in patients with nonvalvular AF [Citation14]. In our study, more than 75% of patients achieved BP goals, particularly elderly subjects; being more than 2 thirds of hypertensives on combined therapy. Remarkably, as CHADS2 score increased, BP control rates improved. In a small study including 78 patients who were receiving antihypertensive drugs and warfarin, nearly 57% of them showed a good BP control [Citation15]. In the last years, BP control has significantly improved in the general hypertensive population worldwide [Citation16]. For example, in Spain, BP control rates raised from 36.1% in 2002 to 46.3% in 2010, likely due to a higher use of combined therapy [Citation17]. However, these figures are clearly inferior to that obtained in our study. Therefore, the data of this study strongly suggest that BP control is much better in hypertensive patients with AF than in the general hypertensive population. This better BP control found in anticoagulated patients with AF may be related with the fact that subjects on vitamin K antagonists must be followed periodically for anticoagulation monitoring and consequently, the follow-up is much stricter. In addition, BP control rates improved as thromboembolic risk increased. It is likely that in these patients, physicians were more worried about the importance of achieving BP goals. On the other hand, the concern about the risk of bleeding complications in uncontrolled hypertensives could also have an important role on the BP control.
In our study, 64% of hypertensive patients were taking diuretics, nearly 60% renin angiotensin system inhibitors and almost 30% beta blockers. It has been reported that inhibition of the renin angiotensin aldosterone system can prevent structural remodeling and recurrent AF. This is particularly true in patients with left ventricular hypertrophy or heart failure [Citation18,Citation19]. As a result, although achieving BP goals should be likely one of the most important targets in the treatment of hypertensive patients with AF, renin angiotensin system inhibitors should be preferable in subjects with paroxysmal AF to prevent recurrences. In patients with permanent AF, beta blockers may help to control simultaneously both BP levels and heart rate [Citation1,Citation12]. On the other hand, our data showed that for every 10% increase in time in therapeutic range, BP control rates improved by 2%. This emphasizes the importance of making a comprehensive approach in these patients with the aim of both improving anticoagulation and BP control.
The limitations of this study are those of an observational study. In addition, many variables were collected from the registries of patient’s usual care medical history, with the consequent limitations. Nevertheless, the high number of patients included, the meticulous care taken with the quality control of the recorded data, and the monitoring may noticeably reduce the potential effect of these limitations. The study was based on a retrospective design, but this is actually an advantage, because it provides 'real life' information on the true clinical BP in clinical practice, whereas in a prospective study, BP control could be highly influenced by patient inclusion biases. Lastly, the results of this study can only be extrapolated to patients having a similar clinical profile and to countries with a similar health-care system [Citation3].
In conclusion, in this study, patients with hypertension and AF exhibited a high thromboembolic risk, but a low risk of bleeding. More than 75% of this high-risk population achieved BP goals, and this rate was higher in elderly patients. More than 2 thirds of hypertensive patients with AF were treated with combined therapy. Diuretics followed by renin angiotensin system inhibitors were the commonest prescribed antihypertensive drugs. The stricter follow-up, the higher thromboembolic risk and the concern about bleeding risk may play a relevant role in the higher BP control rates found in these high-risk patients when compared to general hypertensive population.
Disclosure statement
This study was sponsored by Bayer Hispania S.L.; however, this sponsor had no influence over the course of the study or the collection or interpretation of the results, even though 1 of the authors is a member of Bayer’s medical department. The rest of the authors have no relevant conflict of interest to disclose.
References
- Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–2962.
- Barrios V, Escobar C, Calderón A, et al. Use of antithrombotic therapy according to CHA2DS2-VASc score in patients with atrial fibrillation in primary care. Rev Esp Cardiol (Engl Ed). 2014;67:150–151.
- Barrios V, Escobar C, Prieto L, et al. Anticoagulation control in patients with nonvalvular atrial fibrillation attended at primary care centers in Spain: the PAULA study. Rev Esp Cardiol (Engl Ed). 2015;68:769–776.
- Narasimhan C, Verma JS, RaviKishore AG, et al. Cardiovascular risk profile and management of atrial fibrillation in India: real world data from RealiseAF survey. Indian Heart J. 2016;68:663–670.
- Thomas MC, Dublin S, Kaplan RC, et al. Blood pressure control and risk of incident atrial fibrillation. Am J Hypertens. 2008;21:1111–1116.
- Chen LY, Bigger JT, Hickey KT, et al. Effect of intensive blood pressure lowering on incident atrial fibrillation and P-Wave indices in the ACCORD blood pressure trial. Am J Hypertens. 2015. [Epub Ahead of Print].
- Ogunsua AA, Shaikh AY, Ahmed M, et al. Atrial fibrillation and hypertension: mechanistic, epidemiologic, and treatment parallels. Methodist DebakeyCardiovasc J. 2015;11:228–234.
- Panaich SS, Patel N, Arora S, et al. A review of hypertension management in atrial fibrillation. Curr Hypertens Rev. 2016. [Epub Ahead of Print].
- Nagarakanti R, Wallentin L, Noack H, et al. Comparison of characteristics and outcomes of Dabigatran versus Warfarin in hypertensive patients with atrial fibrillation (from the RE-LY Trial). Am J Cardiol. 2015;116:1204–1209.
- Rao MP, Halvorsen S, Wojdyla D, et al. Blood pressure control and risk of stroke or systemic embolism in patients with atrial fibrillation: results from the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial. J Am Heart Assoc. 2015;4:pii: e002015.
- Vemulapalli S, Hellkamp AS, Jones WS, et al. Blood pressure control and stroke or bleeding risk in anticoagulated patients with atrial fibrillation: results from the ROCKET AF trial. Am Heart J. 2016;178:74–84.
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–1357.
- Rosendaal FR, Cannegieter SC, Van der Meer FJ, et al. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993;69:236–239.
- Kodani E, Atarashi H, Inoue H, et al. Impact of blood pressure control on thromboembolism and major hemorrhage in patients with nonvalvular atrial fibrillation: a subanalysis of the J-RHYTHM registry. J Am Heart Assoc. 2016;5:e004075.
- Guzet F, Bitigen A, Karabay CY, et al. Blood pressure control in anticoagulated hypertensive patients. Blood Press Monit. 2015;20:20–26.
- Barrios V, Escobar C. Letter from Barrios and Escobar regarding article, ‘trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the national health and nutrition examination survey, 2001 to 2010’. Circulation. 2013;127:e859.
- Barrios V, Escobar C, Alonso-Moreno FJ, et al. Evolution of clinical profile, treatment and blood pressure control in treated hypertensive patients according to the sex from 2002 to 2010 in Spain. J Hypertens. 2015;33:1098–1107.
- Heckbert SR, Wiggins KL, Glazer NL, et al. Antihypertensive treatment with ACE inhibitors or beta-blockers and risk of incident atrial fibrillation in a general hypertensive population. Am J Hypertens. 2009;22:538–544.
- Schneider MP, Hua TA, Bohm M, et al. Prevention of atrial fibrillation by Renin-Angiotensin system inhibition a meta-analysis. J Am Coll Cardiol. 2010;55:2299–2307.