Abstract
Purpose: Irregular heart rhythm in the course of atrial fibrillation (AFib) results in lower blood pressure (BP) measurements reproducibility which is further limited by various BP-monitors used. Therefore the aim of our study was to estimate accuracy of oscillometric BP measurement (SpaceLabs 90207) with reference to mercury manometer-based readings.
Material and methods: Study was performed in 47 hemodynamically stable patients aged 63 ± 12 yo with paroxysmal or persistent AFib, at baseline. Patients were reassessed within one week after effective cardioversion (SR; n = 29). BP was measured using Y-tube connection allowing for simultaneous measurements on the same arm with SpaceLabs 90207 and referral method. Mean values were tested with paired t-tests. Additionally, concordance correlation coefficient (ρc) and Bland-Altman plots were assessed. Results were confronted with AAMI, and ESH-IP criteria.
Results: Both during arrhythmia and sinus rhythm diastolic BP differed significantly (Δ = 4.6 ± 6.0 mm Hg, p < .001 and 2.1 ± 4.0 mm Hg, p < .001; for AFib, and SR, respectively), which was not the case for systolic BP. The ρc during arrhythmia equaled 0.89, and 0.75 for systolic and diastolic BP, respectively, which further improved while SR (0.96 and 0.89, respectively). Results confronted against AAMI and ESH-IP showed that all criteria were met except for one (60% vs. required 65% of paired differences of less than 5 mm Hg) during AFib.
Conclusions: The direct comparisons of BP readings allowed to conclude that diastolic blood pressure tended to be slightly overestimated when assessed with SpaceLabs 90207 in patients with both, AFib and SR, which was not a case for systolic BP. When the results were confronted with available validation protocols requirements, all referral criteria were met except for one. Taken together, our results suggest acceptable BP readings dispersion of SpaceLabs 90207 in BP monitoring of patients with both AFib and SR.
Introduction
Atrial fibrillation (AFib) is the most common atrial tachyarrhythmia affecting about 3% of the adult population, with greater prevalence in older persons [Citation1–3]. Apart from the advanced age, there are several other factors which markedly increase the risk of incident AFib, including widely prevalent hypertension [Citation4,Citation5]. It is roughly estimated that hypertension contributes to every second case of AFib in general population [Citation5]. Impaired atrial systolic function, and irregular ventricular rhythm, result in a decrease of stroke volume, as well as large variations in blood pressure (BP) with each heart cycle [Citation6]. Therefore, assessment of arterial BP in patients with atrial fibrillation might be affected by a substantial error with an impact on reliability of patient self-measurements, as well as on 24-hour automatic BP measurements.
There is an ongoing discussion [Citation7–15] concerning an optimal method of BP measurement during atrial fibrillation. Majority of the studies assessing precision and accuracy of automatic measurements in a group of patients with AFib investigated relatively small and heterogeneous groups. They also differed with respect to the protocol and methods of measurement used [Citation16]. Therefore, the conclusions of those studies do not always allow to refer to criteria currently found in validation protocols, such as Association for the Advancement of Medical Instrumentation (AAMI) or European Society of Hypertension International Protocol (ESH-IP). To the best of our knowledge, in the available literature there are only two studies which compared simultaneously two methods of BP measurement performed in AFib patients [Citation7,Citation14]. The comparison protocols used in other studies were primarily based on sequential rather than simultaneous measurements. Moreover, different methods of measurement in the same patients during AFib and after restoration of the sinus rhythm were compared in only one study [Citation15].
The aim of the presented study was to evaluate the agreement of oscillometric and auscultatory measurements of arterial BP performed simultaneously in patients with atrial fibrillation, both before and after sinus rhythm restoration.
Materials and methods
Forty seven consecutive patients (82% men; mean age 63 ± 12 yo.; BMI 28.8 ± 4.6 kg/m2) were qualified to the study. The inclusion criteria included stable hemodynamic clinical condition and 12-lead ECG-confirmed AFib. The only protocol-based study exclusion was hemodynamic instability. The participants of the study were consecutively enrolled among patients admitted to the Department of Hypertension and Diabetology, and the Department of Cardiology and Cardiac Electrotherapy of the Teaching Hospital of Medical University of Gdańsk, Poland. The direct reason for the hospitalization was planned electrical or pharmacological cardioversion.
The main goal of the study was to test the agreement of the two different BP measurement methods in the setting of AFib. BP data were obtained concurrently from (1) mercury sphygmomanometer using auscultatory technique, and (2) the oscillometric method obtained from SpaceLabs 90207 ABP device (Spacelabs Healthcare, WA, USA). The latter is one of the most commonly used device for ambulatory BP monitoring meeting the validation criteria of AAMI as well as the British Hypertension Society [Citation17,Citation18]. All measurements were obtained in a quiet room after several minutes of rest. The cuff width was adjusted to the arm circumference and it was positioned at the level of the heart. The attachment of air tubes of the mercury sphygmomanometer and the SpaceLabs 90207 device through Y-tube connection allowed for simultaneous measurements. The cuff was inflated via SpaceLabs 90207 in-built compressor, and it was triggered manually by the observer every two minutes. The rate of cuff deflation determined by the standard procedure implemented in SpaceLabs 90207 was approximately 4 mm Hg/s. During each individual session, the simultaneous BP measurements (device-, and observer-obtained) were repeated ten times (10 pairs of readings). In the auscultatory method, the systolic BP was assigned to the phase I Korotkoff sounds [Citation19]. The diastolic BP was determined at the moment at which heart sounds were no longer audible (Korotkoff phase V) . The baseline assessment of BP agreement was performed during arrhythmia and then replicated within 7 day period after electrical or pharmacological cardioversion (sinus rhythm restored, n = 29). All measurements were performed by the same observer.
For the analysis the averaged value of successfully obtained pairs of measurements was used.
The heart rate recorded during deflation of the cuff using digital electrocardiographic signal monitoring (PowerLab, ADInstruments Inc.) was contrasted with the SpaceLabs 90207 device readings and averaged over all measurement in the same patient.
Patients were fully informed about the study protocol and gave their written consent. The study was designed in accordance with the Helsinki Declaration and was approved by the local ethics committee (NKEBN/449/2004).
Statistical methods
All statistical analyses were performed using STATISTICA (StatSoft, Inc. 2014, version 12, www.statsoft.com.) The agreement of data distribution with normal distribution was investigated with the use of the Shapiro-Wilk method. Mann-Whitney test was employed to compare baseline BP values between patients who underwent successful cardioversion vs. those who did not. The differences between paired measurements were tested against zero value. Group values were compared by the Wilcoxon test for two dependent samples. The reproducibility of BP readings recorded with the two methods was expressed with concordance correlation coefficients [Citation20]. Additionally, the compatibility of two measurement methods was analyzed with the use of the Bland and Altman plots.
Results
In 14 patients (29%) the diagnosis of arrhythmia was related to coronary artery bypass grafting or prosthetic valve implantation of either the mitral or aortic valve. The frequency of occurrence of concomitant diseases is presented in . The most common coexisting disease was arterial hypertension (76%). The left ventricular ejection fraction assessed during patient qualification for the study was 46.6 ± 11.5%.
Table 1. Frequency of occurrence of concomitant diseases in the investigated population.
29 patients underwent successful cardioversion (sinus rhythm restored for at least one subsequent week). At baseline, systolic and diastolic BP did not differ significantly for patients who underwent successful cardioversion vs. in those who failed to restore sinus rhythm (p > .50 for all comparisons both for auscultatory and oscillometric techniques).
Agreement of blood pressure measurement methods
The ratio of effective measurements performed with the SpaceLabs 90207 device was 88% during arrhythmia and 95% after restoring sinus rhythm.
Averaged BP values measured with the use of the oscillometric and auscultatory methods are presented in . During atrial fibrillation the mean difference between both methods was 1.8 ± 6.9/4.6 ± 6.0 mm Hg for the systolic and diastolic BP, respectively. Corresponding mean differences after sinus rhythm restoration were 0.8 ± 6.3 mm Hg and 2.1 ± 4.0 mm Hg ().
Table 2. Blood pressure and heart rate values as measured by compared methods.
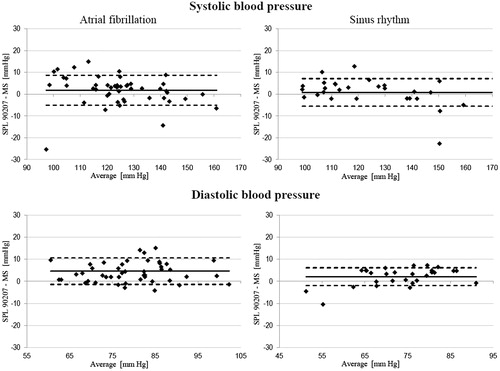
As shown in , the differences between values of BP measurements, both during arrhythmia and sinus rhythm, differed significantly from zero for diastolic but not systolic pressure. The oscillometric device used in the study indicated significantly lower heart rate in comparison to ECG detection only in atrial fibrillation group.
The measurements of precision and accuracy of the SpaceLabs 90207 vs. mercury manometer-based readings were assessed using concordance correlation coefficient (ρC) [Citation20]. The ρC during arrhythmia equaled 0.89, and 0.75 for systolic and diastolic BP, respectively. The corresponding ρC values after restoration of sinus rhythm were as follows: 0.96 and 0.89, respectively.
The agreement between paired measurements were also tested using Bland-Altman approach ().
Figure 1. Bland-Altman analysis of systolic and diastolic BP values recorded with SpaceLabs 90207 (SPL 90207) and mercury sphygmomanometer (MS), both during AFib and after restoration of sinus rhythm. Continuous line represents mean value of differences, while dotted lines show ±1SD. On X-axis the average value of BP measured simultaneously by SpaceLabs 90207 and mercury sphygmomanometer is presented.
Obtained results were also analyzed against criteria of the standard protocols for evaluation of BP devices ().
Table 3. Average differences, standard deviations as well as percentage differences of 5, 10 and 15 mm Hg, between the systolic (SBP) and diastolic (DBP) BP values recorded with SpaceLabs 90207 device (SPL 90207) and mercury sphygmomanometer (MS). Data obtained both, during AFib and after restoring sinus rhythm.
During AF, as well as sinus rhythm, obtained data satisfied almost all criteria of both protocols.
The only ESH-IP protocol missed criterion was the threshold of 65% of paired systolic BP measurements differing less than 5 mm Hg during AFib.
Discussion
Current guidelines recommend repeated measurements for improving accuracy of the assessment of BP in patients with arrhythmia. Generally accepted method for BP measurement is auscultatory one, however, nowadays the automatic devices are in widespread use. The reliability of automatic measurements, which are often based on the oscillometric method, remains uncertain in patients with AFib [Citation19]. This fact may potentially translate into relevant clinical consequences considering that home BP measurements, as well as 24-hour measurements (both crucial in the diagnosis of masked and/or white-coat hypertension) are almost always performed with the use of automatic devices.
Our study has demonstrated that simultaneously measured BP on the same arm shows comparable systolic BP readings (oscillometric vs. manual method), regardless of cardiac rhythm (). To the contrary, the values of diastolic BP measured by SpaceLabs 90207 device were significantly higher in both arrhythmia and sinus rhythm (Δ = 4.59 mm Hg, p < .001; Δ = 2.1 mm Hg, p = .008, respectively). These findings might have been only partially explained by naturally greater variances of mean systolic vs. mean diastolic BP values (). However, the analysis of the agreement of paired observations showed marked differences in concordance correlation coefficients i.e. the ρC for diastolic BP during arrhythmia equaled 0.75 (poor agreement), whereas ρC for systolic BP was 0.89, only marginally missing the arbitral values indicating moderate agreement (set at 0.90) [Citation20]. The respective concordance coefficients after restoration of sinus rhythm were 0.89 for diastolic BP, and 0.96 for systolic BP, the latter indicating substantial agreement between the two methods.
Except for the effect size, our results are in line with data presented in the meta-analysis by G. Stergiou [Citation16] summarizing six studies [Citation9–14] including 487 patients with AFib which showed that automatic devices tend to overestimate systolic by 0.5 mm Hg (95% CI −0.9, 1.9) and diastolic by 2.5 mm Hg (95% CI −0.6, 5.7) BP in comparison to the auscultatory method.
Interestingly, in recent study by Maselli published in 2015 in the group of 100 patients with AFib no significant differences between systolic BP values were obtained with the use of automatic and mercury devices, while diastolic BP values were significantly lower (2.4 ± 8.5 mm Hg) when oscillometric device was used [Citation15].
Analysis of the distribution of the average BP difference provides a basis for validation protocols for BP measuring devices [Citation21–23]. The average difference of BP below 5 mm Hg, as well as standard deviation of this difference below 8 mm Hg, are validation criteria used in the AAMI protocol [Citation23]. On the other hand, the ESH-IP and BSH protocols are based on the fraction of paired measurements with differences below 5, 10 and 15 mm Hg [Citation21,Citation22]. Categorization of our results according to those criteria allowed to claim that in case of systolic, as well as diastolic pressure, the average difference between measurements made with the SpaceLabs 90207 device and the sphygmomanometer was less than 5 mm Hg and the standard deviation was below 8 mm Hg, which meets the AAMI protocol criteria (). Those conditions were met in both clinical situations investigated, i.e. during AFib and after reestablishing sinus rhythm.
In seven published validations of use of automatic devices in patients with AFib the average difference between measurements was less than 5 mm Hg for systolic BP [Citation9–15]. However, this criterion was not met in the studies concerning diastolic BP [Citation9,Citation13]. Taking into consideration the next criterion of the AAMI protocol, in five studies reporting standard deviation of the average BP values between measurements [Citation9,Citation11,Citation13–15], three validations showed that the value exceeded 8 mm Hg for systolic BP [Citation9,Citation11,Citation15] and two - for the diastolic one [Citation9,Citation15].
Although our study was not primarily designed to comply with any available specific validation protocol requirements, we decided to confront our results with AAMI, ESH-IP criteria. As presented in our results showed a high agreement between the measurements performed with the use SpaceLabs 90207 device and the sphygmomanometer. With relation to ESH-IP protocol, the proportion of the paired measurements should equal at least 65, 81 and 93% for fraction of differences in compared measurements less than 5, 10 and 15 mm Hg, respectively. Apart from unsatisfactory percentage of measurements of systolic pressure at the time of AFib differing by less than 5 mm Hg (60% versus the required 65%), all other criteria throughout the duration of arrhythmia were met. Moreover, while assessing the BP during sinus rhythm, all the criteria for comparison of the auscultatory and oscillometric methods were met.
In available literature, in which the absolute difference between BP measurements taken with automatic devices in terms of the reference auscultatory method during AFib were reported, in order to check the agreement of methods according to the ESH-IP protocol, at least 65% of the carried measurements differed by less than 5 mm Hg in four out of 8 validations of automatic devices for the systolic BP [Citation8,13,Citation14], and only in 2 validations for diastolic BP [8,Citation14].
In our study, the percentage of effective BP measurements by using SpaceLabs 90207 in patients with AFib was 88% which corresponds to previously published data ranging from 80% to 94% [Citation8,Citation9,Citation24]. While testing a device for a 24-hour BP measurement using the auscultatory method with an R-wave gated ECG, 86% of satisfactory measurements were obtained [Citation8].
In our study the heart rate during AFib indicated by the SpaceLabs 90207 device was significantly lower than determined on the basis of ECG recording. However, restoring sinus rhythm did not show any significant impact on accuracy of heart rate detection with the oscillometric device.
Amongst studies assessing precision of automatic devices with AFib, only two refer to differences between the heart rate frequency measured by oscillometric devices and auscultatory method at the heart apex or ECG monitoring. In patients with AFib, this difference was found to be 5.3 ± 13.7 beats per minute for Omron HEM 711 AC (Omron Healthcare, INC., Vernon Hills, IL, USA), and 10.2 ± 21.2 for Welch-Allyn 52 000 (Welch Allyn, Inc. Nellcor Puritan Bennett™; Skaneateles Falls, NY, USA). In the control group of patients with sinus rhythm, there was a notably smaller discrepancy in detection of heart rate - 0.3 ± 5.4 and 0.1 ± 4.7 beats per minute for the two devices mentioned above, respectively [Citation7].
Significant difference between the automated device (Welch-Allyn Vital Signs Monitor 300; Welch Allyn, Beaverton, OR, USA) and cardiac monitor heart rate measurements (−3.91 ± 12.0 beats per minute) was found also in patients with AFib in study by Anastas [Citation11].
It is worth noticing that in our study the assessment of heart rate was done through analyzing a continuous ECG recording, which certainly increases the precision of reading, especially in the group of patients with AFib. Moreover, the precision of heart rate values is most likely influenced by a relatively long time of detection — required by the algorithm implemented in the SpaceLabs 90207 device — involving the entire cuff deflation time.
Strengths and limitations
An important asset of our study is the fact that the measurements performed with the use of both the sphygmomanometer and the automatic device were carried out simultaneously on the same arm, with the Y-tube connection used. It allowed assessment of BP in a simultaneous way by means of two different measurement methods which previously has been performed only in two available studies [Citation7,Citation14].
Until now, the majority of published studies which compared manual and automatic devices were carried out in relatively small groups. Although only 49 patients with AFib were qualified according to the protocol, the significance of our study was greatly increased by performing 10 measurements in each of the examined patients, whereas in previous studies BP measurements were taken up to 4 times. Another advantage of our study appears to be the fact that the measurements were repeated in a subgroup of the same patients before and after regaining sinus rhythm.
A possible limitation of this study is the lack of complete fulfillment of the AAMI/ESH-IP protocol, however, it should be noted that our study was not meant to be a validation procedure, and as such it did not include e.g. an interobserver-variability analysis. By protocol, all measurements were carried out by one experienced doctor, whose skills and accuracy in BP measurement were confirmed by multi-stethoscope testing.
It has to also be underscored that default cuff deflation rate of SpaceLabs 90207 device is set at 4 mm Hg/s which exceeds a recommended deflation rate for auscultatory measurements of BP in patients with AFib (2 mm Hg/s) [Citation19]. This, however, was mitigated by a multiple replications of the simultaneous measurements in each subject which is more accurate as compared to sequential recordings, especially in AFib. However, a minor systematic error may not be completely excluded.
Lastly, the tested device is by definition dedicated to ambulatory BP measurements. It is impossible to simultaneously compare out-of-office BP readings of SpaceLabs 90207 with human-operated, stationary mercury manometer using auscultatory method as it was designed in our study. We are aware of the fact that the results of our comparisons may not precisely match the out-of-office readings, however, we decided to give high priority to employing best-known, non-invasive referral method for the BP measurements, i.e. auscultatory mercury sphygmomanometer [Citation19].
Conclusion
The direct comparisons of BP readings allowed to conclude that diastolic blood pressure tended to be slightly overestimated when assessed with SpaceLabs 90207 in patients with both, AFib and SR, which was not a case for systolic BP. When the results were confronted with available ESH-IP, and AAMI requirements, all referral criteria were met except for one. Taken together, our results suggest acceptable BP readings dispersion of SpaceLabs 90207 in BP monitoring of patients with both AFib and SR.
Disclosure statement
The authors declare no conflicts of interest relevant to this work.
Authors completed the work as a part of their statutory academic activity for Medical University of Gdańsk, Poland. Authors declare no third party financial support.
References
- Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–2962.
- Bjorck S, Palaszewski B, Friberg L, et al. Atrial fibrillation, stroke risk, and warfarin therapy revisited: a population-based study. Stroke. 2013;44:3103–3108.
- Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837–847.
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–1357.
- Manolis AJ, Rosei EA, Coca A, et al. Hypertension and atrial fibrillation: diagnostic approach, prevention and treatment. Position paper of the Working Group “Hypertension Arrhythmias and Thrombosis” of the European Society of Hypertension. J Hypertens. 2012;30:239–252.
- Gosselink AT, Blanksma PK, Crijns HJ, et al. Left ventricular beat-to-beat performance in atrial fibrillation: contribution of Frank-Starling mechanism after short rather than long RR intervals. J Am Coll Cardiol. 1995;26:1516–1521.
- Lamb TS, Thakrar A, Ghosh M, et al. Comparison of two oscillometric blood pressure monitors in subjects with atrial fibrillation. Clin Invest Med. 2010;33:E54–E62.
- Stewart MJ, Gough K, Padfield PL. The accuracy of automated blood pressure measuring devices in patients with controlled atrial fibrillation. J Hypertens. 1995;13:297–300.
- Lip GY, Zarifis J, Beevers M, et al. Ambulatory blood pressure monitoring in atrial fibrillation. Am J Cardiol. 1996;78:350–353.
- Jani B, Bulpitt CJ, Rajkumar C. Blood pressure measurement in patients with rate controlled atrial fibrillation using mercury sphygmomanometer and Omron HEM-750CP deice in the clinic setting. J Hum Hypertens. 2006;20:543–545.
- Anastas ZM, Jimerson E, Garolis S. Comparison of noninvasive blood pressure measurements in patients with atrial fibrillation. J Cardiovasc Nurs. 2008;23:519–524.
- Vázquez-Rodríguez B, Pita-Fernández S, Regueiro-López M, et al. Concordance between automatic and manual recording of blood pressure depending on the absence or presence of atrial fibrillation. Am J Hypertens. 2010;23:1089–1094.
- Stergiou GS, Destounis A. Accuracy of automated oscillometric blood pressure measurement in patients with atrial fibrillation. J Hypertens. 2011;29:e2. [1A.04]
- Farsky S, Benova K, Krausova D, et al. Clinical blood pressure measurement verification when comparing a Tensoval duo control device with a mercury sphygmomanometer in patients suffering from atrial fibrillation. Blood Press Monit. 2011;16:252–257.
- Maselli M, Giantin V, Corrado D, et al. Reliability of oscillometric blood pressure monitoring in atrial fibrillation patients admitted for electric cardioversion. J Clin Hypertens. 2015;17:558–564.
- Stergiou GS, Kollias A, Destounis A, et al. Automated blood pressure measurement in atrial fibrillation: a systematic review and meta-analysis. J Hypertens. 2012;30:2074–2082.
- O’Brien E, Mee F, Atkins N, et al. Accuracy of the SpaceLabs 90207 determined by the British Hypertension Society protocol. J Hypertens 1991;9:573–574.
- Sphygmomanometers for Ambulatory Blood Pressure Measurement. [Cited 2017 Jul 19] Available at: http://www.dableducational.org/sphygmomanometers/devices_3_abpm.html#Ref2
- O’Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848.
- Lin LI-K. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–268.
- O’Brien E, Atkins N, Stergiou G, et al. European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit. 2010;15:23–38.
- O’Brien E, Petrie J, Littler W, et al. The British Hypertension Society protocol for the evaluation of automated and semi-automated blood pressure measuring devices with special reference to ambulatory systems. J Hypertens. 1990;8:607–619.
- Nonivasive sphygmomanometers. Part 2:Clinical validation of automated measurement type. American National Standards Institute. ANSI/AAMI/ISO 81060-2. AAMI; [Cited 2017 Jul 19] available at: http://webstore.ansi.org
- Almeida L, Amado P, Vasconcelos N, et al. Is ambulatory blood pressure monitoring reliable in hypertensive patients with atrial fibrillation? Rev Port Cardiol Orgão of Soc Port Cardiol Port J Cardiol off J Port Soc Cardiol. 2001;20:647–650. [Abstract]
