Abstract
Purpose: Inter-arm systolic blood pressure differences (IASBPD) and inter-leg systolic blood pressure differences (ILSBPD) have arisen as potential tools to detect peripheral artery disease (PAD) and individuals at high cardiovascular risk. This study aims to evaluate the diagnostic accuracy of IASBPD and ILSBPD to detect PAD, and whether IASBPD or ILSBPD improves diagnostic accuracy of the oscillometric ankle-brachial index (ABI).
Materials and methods: In this prospective study, eligible for inclusion were consecutive adults, with at least one of the following cardiovascular risk factors: diabetes, dyslipidemia, hypertension, smoking habit or age ≥65. IASBPD, ILSBPD and ankle-brachial index (ABI) were measured in all participants through four-limb simultaneous oscillometric measurements and compared with Doppler ABI (reference test, positive cut-off: ≤ 0.9).
Results: Of 171 subjects included, PAD was confirmed in 23 and excluded in 148. Thirteen and 38 subjects had IASBPD and ILSBPD ≥10 mmHg, respectively. Pearson correlation with Doppler ABI of IASBPD and ILSBPD was 0.073 (P = .343) and −0.628 (P < .001), respectively. Diagnostic accuracy of an ILSBPD ≥10 mmHg to detect PAD was: sensitivity = 69.6% (95%CI = 48.6–90.5), specificity = 85.1% (79.1–91.2), diagnostic odds ratio (dOR) = 13.1 (4.8–35.5) and area under ROC curve (AUC) = 0.765 (0.616–0.915). IASBPD had an AUC = 0.532 (0.394–0.669), and oscillometric ABI had an AUC = 0.977 (0.950–1.000). The addition of ILSBPD to oscillometric ABI reduced dOR from 174.0 (38.3–789.9) to 34.4 (9.5–125.1). Similarly, the addition of IASBPD reduced dOR to 49.3 (14.6–167.0).
Conclusions: In a Primary Care population with ≥1 cardiovascular risk factors, ILSBPD showed acceptable diagnostic accuracy for PAD, whilst IASBPD accuracy was negligible. However, the combination of ILSBPD (or IASBPD) with oscillometric ABI did not improve the ability to detect PAD. Thus, oscillometer ABI seems to be preferable to detect PAD and individuals at high cardiovascular risk. ILSBPD could be uniquely recommended for the diagnosis of PAD when blood pressure measurements in upper limbs are not possible.
Introduction
Peripheral artery disease (PAD), a clinical indicator of widespread atherosclerosis, affects 16.8% of women and 19.8% of men in elderly population [Citation1]. Although PAD is highly prevalent, only one third of PAD cases have typical symptoms [Citation2,Citation3]. This fact, along with Doppler ankle-brachial index (ABI) limitations—the non-invasive gold standard in PAD diagnosis—means that up to 80% of PAD patients remain underdiagnosed and undertreated. An aggressive therapy in such silent cohort, which is at high cardiovascular risk, could improve morbidity and mortality [Citation4].
Usually defined as ≥10 mmHg, a high inter-arm systolic blood pressure difference (IASBPD), with a prevalence rising up to 19.6%, is a common finding in clinical settings [Citation5]. Its recognition has implications, not only for an accurate diagnosis and management of hypertension, but also as a proxy marker for PAD [Citation6]. Since the importance of bilateral brachial blood pressure measurements has been emphasized in routine clinical practice [Citation7,Citation8], IASBPD may be a feasible tool to diagnose PAD and patients at increased cardiovascular risk and mortality [Citation9,Citation10].
Automated blood pressure monitors based on oscillometry have shown great feasibility and good capacity to diagnose PAD [Citation11,Citation12]. Interestingly, they also allow the measurement of simultaneous IASBPD and inter-leg systolic blood pressure difference (ILSBPD). This is important, since a simultaneous technique when measuring IASBPD has shown a threefold increase in the prevalence of IASBPD in comparison to a consecutive technique [Citation13]. In addition, these different techniques also bias the association of a high IASBPD with cardiovascular morbidity and mortality [Citation6,Citation14,Citation15].
Like IASBPD, ILSBPD has proven to be closely related with PAD and may indicate high cardiovascular risk [Citation6]. A meta-analysis dating back to 2015 showed that a simultaneously measured IASBPD ≥10 mmHg predicted PAD with a sensitivity of 16.6% and a specificity of 91.9% [Citation6]. However, evidence regarding diagnostic accuracy and cut-offs of ILSBPD to detect PAD is needed. As lower limbs are more prone to be affected by PAD than upper limbs [Citation16], we hypothesized that ILSBPD could be a better predictor for PAD than IASBPD. To our knowledge, this is the first work analysing diagnostic accuracy and optimal cut-offs for simultaneously measured IASBPD and ILSBPD in comparison to the Doppler ABI in a Primary Care population. A secondary aim was to analyze whether the addition of either IASPBPD or ILSBPD to the oscillometric ABI could improve the capacity of the oscillometer to detect PAD.
Material and methods
Design and participants
This prospective observational study aimed to compare IASBPD, ILSBPD and oscillometric ABI (index tests) and Doppler ABI (reference test) to detect PAD, and it fulfils the Standards for Reporting of Diagnosis Accuracy Group (STARD) [Citation17,Citation18], (Supplemental Chart 1). The study includes 174 consecutive subjects from the Primary Care Center of Tragacete (Cuenca, Spain), recruited from January 2015 to May 2016. Inclusion criteria were age ≥65 or subjects with at least one of the following cardiovascular risk factors: diabetes, dyslipidemia, hypertension or smoking habit (current or former). Exclusion criteria were: (i) ulceration or edema in the leg, (ii) atrial fibrillation, (iii) inability to tolerate supine position, (iv) morbid obesity and (v) refusal to sign the informed consent. This study was approved by the Clinic Investigation Ethic Committee of the Health Area of Cuenca (Spain), REG: 2015jPI0815. All participants were informed of the aim and procedures of the study giving written informed consent according to the general recommendations of the Declaration of Helsinki [Citation19].
Statistical power
We hypothesized that a positive likelihood ratio (LR+) > 2.5 would have clinical value. In our study, following Simel’s equation and according to i) a sensitivity to detect PAD of an ILSBPD ≥10 mmHg of 69%, ii) a specificity of 85%, and iii) a prevalence of PAD of 13.5%, a sample size of 171 subjects could assure that the 95% confidence interval (CI) excludes a LR + above 2.9 [Citation20].
Variables
We recorded the following variables from electronic medical records or interviews: gender, age (years), most recent value of creatinine within last year (mg/dl), adjusted creatinine clearance (ml/min/1.73m2) [Citation21], tobacco (packs/year), hypertension, dyslipidemia and diabetes status. Additionally, we measured height (cm), weight (kg), body mass index (kg/m2), heart rate (beats/minute), waist and hip circumference (cm) and waist-hip ratio by standardized procedures.
Reference test (doppler ABI) and index tests (IASBPD, ILSBPD and oscillometric ABI)
All the measurements were performed in a randomized order by a unique nurse with experience in ABI determinations, after all participants rested supine for 10 minutes. In both techniques (Doppler and oscillometric), the lower ABI between right and left legs was chosen, thus considering subjects (not legs) as the unit of analysis. It avoids duplication of both IASBPD and ILSBPD within each subject.
Doppler ABI was performed using i) a Ultrasonic-Pocket-Doppler-Edan-Sonotrax-Basic® with an 8 MHz probe and ii) a sphygmomanometer Riester-diplomat-presameter® with appropriate cuffs, according to a standardized protocol [Citation22]. Doppler ABI calculation was: highest Doppler ankle systolic blood pressure (SBP) (dorsalis pedis or posterior tibial)/highest Doppler SBP between both arms. A Doppler ABI ≤0.9 was considered the reference test to diagnose PAD.
In oscillometric technique, two simultaneous and consecutive measurements on the four limbs were performed using four OMRON-M3® (HEM-7200E-Omron-Healthcare) with appropriate cuffs. The oscillometric ABI was calculated as: mean oscillometric SBP in the leg/mean oscillometric SBP in the arm with the highest pressure. The cut-off for oscillometric ABI was also 0.9.
Brachial and leg SBP were measured simultaneously by oscillometry in both arms and legs during ABI measurements, and summarized as the average between first and second measurements. IASBPD was calculated as: absolute value of (right arm SBP – left arm SBP). ILSBPD was calculated as: absolute value of (right leg SBP – left leg SBP). In the oscillometric technique, when neither of the two consecutive measurements recorded any pressure (i.e. oscillometric error), the pressure was considered “0 mmHg” [Citation12].
Statistical analyses
Normal distribution of variables was tested by both graphic (normal probability plot) and statistical (Kolmogorov-Smirnov test) procedures. Quantitative variables were compared using Student’s t-test and Mann-Whitney U-test in normal and non-normal distributions, respectively. Qualitative variables were compared using Pearson X2. A two-sided P-value ≤.05 was considered significant.
The correlation between Doppler ABI and both IASBPD and ILSBPD was estimated by Pearson correlation coefficient.
A new dichotomous combined variable (“IASBPD + oscillometric ABI”) was created to evaluate whether the addition of IASBPD to the oscillometric ABI improves the capacity of the oscillometer to detect PAD. The result was considered positive when either IASBPD or oscillometric ABI were positive, and negative when both were negative. Similarly, we established a variable “ILSBPD + oscillometric ABI”.
The diagnostic accuracy of the index tests (IASBPD, ILSBPD, oscillometric ABI, “IASBPD + oscillometric ABI” and “ILSBPD + oscillometric ABI’) was assessed using sensitivity, specificity, positive predictive value (PPV+), negative predictive value (PV–), (LR+), negative likelihood ratio (LR–), diagnostic odds ratio (dOR) and receiver operational characteristic (ROC) curves with 95% CIs. The area under ROC curves (AUC) were estimated through a nonparametric empirical approach, and the curves were compared using DeLong’s test [Citation23]. The best overall cut-offs were estimated using the Youden index. Statistical analyses were performed using IBM® SPSS® 20 and Medcalc® 15.2.2.
Results
From the 174 subjects (348 legs) that accepted to participate in the study, 3 subjects (6 legs) were excluded as having calcification (ABI >1.4) in both legs. Thus, 171 subjects (342 legs) were analyzed; mean age was 70.5 ± 13.6 years, and 87 (50.9%) were male. Seven subjects (4.1%) showed calcification in one leg. Two subjects (1.2%) had oscillometric errors in both legs, while 10 subjects (5.8%) had oscillometric errors in only one leg. and depict the flow chart of the study; depicts characteristics of the participants grouped by ILSBPD.
Figure 1. STARD flow chart of inter-arm systolic blood pressure difference (index test) to detect peripheral artery disease according to Doppler ankle-brachial index (reference standard). IASBPD: inter-arm systolic blood pressure difference, PAD: peripheral arterial disease.
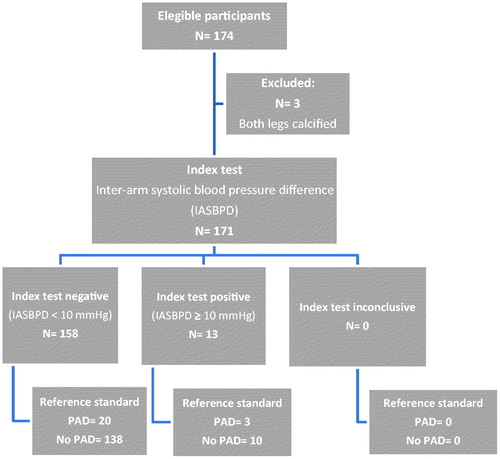
Figure 2. STARD flow chart of inter-leg systolic blood pressure difference (index test) to detect peripheral artery disease according to Doppler ankle-brachial index (reference standard). ILSBPD: inter-leg systolic blood pressure difference, PAD: peripheral arterial disease.
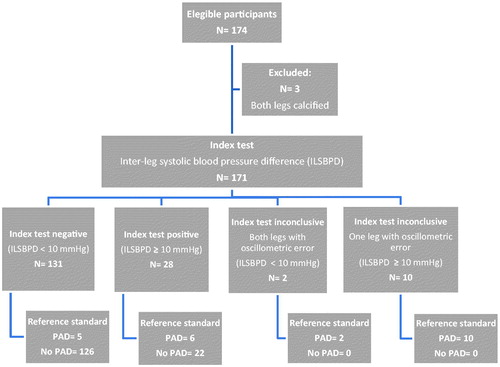
Table 1. Characteristics of the participants by inter-leg systolic blood pressure difference.
In our study, 13 (7.6%) and 1 (0.6%) out of 171 subjects had an IASBPD ≥10 and ≥15 mmHg, respectively. Similarly, 38 (22.2%), 23 (13.5%) and 11 (6.4%) out of 171 subjects had an ILSBPD ≥10, ≥ 15 and ≥20 mmHg, respectively.
Correlation of Doppler ABI with IASBPD and ILSBPD were 0.073 (P = .343) and −0.628 (P < .001), respectively.
depicts the diagnostic performance of IASBPD, ILSBPD, oscillometric ABI, “IASBPD + oscillometric ABI” and “ILSBPD + oscillometric ABI’) in comparison to Doppler ABI to detect PAD. For IASBPD, ILSBPD and oscillometric ABI, the AUCs for predicting PAD were 0.532 (95% CI: 0.394–0.669), 0.765 (95% CI: 0.616–0.915), and 0.977 (95% CI: 0.950–1.000), respectively, (). Differences of AUCs were: IASBPD-ILSBPD: 0.234 (95% CI: 0.015–0.452), P = .036; IASBPD-oscillometric ABI: 0.445 (95% CI: 0.303–0.587), P < .001 and ILSBPD-oscillometric ABI: 0.212 (95% CI: 0.069–0.354), P = .003. “IASBPD + Oscillometric ABI” had a dOR = 49.3 (95% CI: 14.6–167.0), whilst “ILSBPD + Oscillometric ABI” had a dOR = 34.4 (9.5–125.1). The best cut-off for oscillometric ABI was 1.02 (sensitivity = 95.7% and specificity = 91.9%).
Figure 3. Hierarchical receiver operating characteristic curves for inter-arm systolic blood pressure differences, inter-leg systolic blood pressure differences and oscillometric ABI according to Doppler ankle brachial index (reference standard). Legend. Area under ROC curves for inter-arm systolic blood pressure difference, inter-leg systolic blood pressure difference, and oscillometric ankle brachial-index were 0.532 (95% CI: 0.394–0.669), 0.765 (95% CI: 0.616–0.915) and 0.977 (95% CI: 0.950–1.000), respectively.
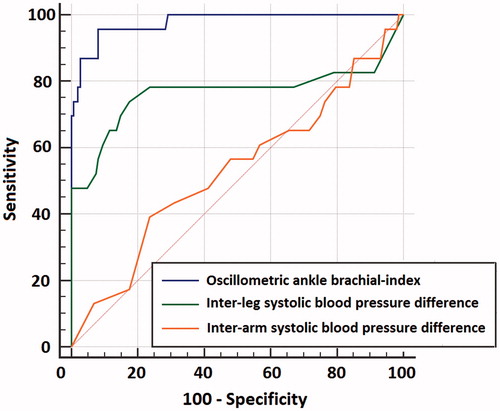
Table 2. Diagnostic performance of peripheral artery disease indicators as compared with Doppler ankle-brachial index.
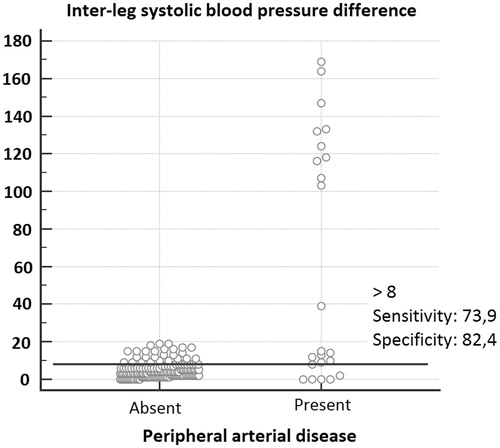
depicts interactive dot diagram for an ILSBPD ≥10 mmHg testing for PAD.
Figure 4. Interactive dot diagram for an inter-leg systolic blood pressure difference ≥10 mmHg testing for peripheral artery disease. Legend. Ten out of 10 unilateral leg oscillometric errors —with inter-leg systolic blood pressure differences ≥100 mmHg— were true positives for peripheral artery disease, increasing sensitivity from 54.6% to 69.6%.
Discussion
This study analyzed the diagnostic accuracy of IASBPD and ILSBPD to detect PAD when compared to Doppler ABI as the reference test in a Primary Care population. Our results support that ILSBPD has acceptable diagnostic performance to diagnose PAD whilst IASBPD shows negligible capacity. The addition of either IASBPD or ILSBPD to the oscillometric ABI did not improve the diagnostic accuracy of the oscillometer to detect PAD.
In our study, ILSBPD identified PAD with a sensitivity and specificity of 69.6% and 85.1%, respectively. With a dOR of 13.1, in our population, the odds for a positive test among subjects with PAD would be 13 times higher than the odds for a positive test among subjects without PAD. The dOR is not influenced by the prevalence and synthesizes in a single value the diagnostic performance of a test. Just one example in order to contextualize the magnitude of this value, this dOR value would almost double that reported by exercise electrocardiography testing for coronary artery disease [Citation24]. ILSBPD performed slightly better to confirm than to exclude the disease, with LR + close to 5.0 and specificity of 85.1%. Nevertheless, from a clinical perspective, and due to a relatively low prevalence of PAD, PV– would be better than PV+, in such a way that only approximately 5% of those testing negative in the test would have PAD condition (false negatives). As ILSBPD >10 mmHg seems to still have relatively low specificity and PV + compared to Doppler ABI, we suggest performing formal ABI in these patients. The best cut-off for ILSBPD in our study was 8.5 mmHg, which is close to that reported in a large study for ILSBPD testing for prevalent stroke [Citation25].
An important difference between ILSBPD and IASBPD is that the latter should be performed in routine clinical practice, since bilateral arm measurements are recommended to accurately diagnose hypertension [Citation7,Citation8]. Thus, IASBPD would be a more feasible tool than ILSBPD to diagnose PAD. However, although the relation of an increased simultaneously measured IASBPD with PAD has been established [Citation6], our study failed to prove it, with negligible capacity of an IASBPD ≥10 mmHg to detect PAD. The low estimates of sensitivity (13%) and specificity (93.2%) of an IASBPD ≥10 mmHg in our study are similar to those reported in a previous meta-analysis (sensitivity = 16.6%, specificity =91.9%) [Citation6].
Several meta-analyses have proved that sensitivity of oscillometric ABI is only moderate [Citation11,Citation12]. In the present study, oscillometric ABI showed excellent ability to ascertain PAD (specificity = 98%), and moderate-high sensitivity (78.3%). Despite the abovementioned acceptable diagnostic accuracy of ILSBPD, and considering the great feasibility of oscillometric ABI, perhaps the most relevant clinical questions would be whether: (1) ILSBPD is better than oscillometric ABI and (2) the addition of ILSPBPD improves the ability of oscillometric ABI to detect PAD. In this sense our data support that the diagnostic performance of oscillometric ABI was far better than ILSBPD. Moreover, combining oscillometric ABI with ILSBPD—considering PAD when either ILSBPD or oscillometric ABI are positive—did not improve the diagnostic accuracy of oscillometric ABI. The addition of ILSBPD to oscillometric ABI would certainly add two “true positives” (raising sensitivity from 78% to 87%), but at the expense of including 21 “false positives” (lowering specificity from 98% to 84%). As expected due to a negligible diagnostic accuracy, IASBPD neither improved the ability of the oscillometric ABI to detect PAD.
In simultaneous technique, two oscillometers are needed to perform ILSBPD; four are needed to perform oscillometric ABI. With a cost of 60–100 dollars per device, cost savings do not seem to justify the use of ILSBPD instead of oscillometric ABI. Moreover, oscillometric ABI can be calculated in almost the same time as ILSBPD [Citation12]. Although an ILSBPD ≥10 mmHg suggests PAD (and thus individuals at very high cardiovascular risk) with reasonable certainty, ILSBPD may be only indicated when performing oscillometric ABI is impossible due to the incapacity of measuring blood pressure in upper limbs (cases of lymphedema, amputation or deformity).
Our study did not correlate with anatomical imaging (e.g. angiography). However, the physiological reason behind the capacity of IASBPD and ILSBPD to detect PAD may be that atherosclerosis is habitually not symmetrically distributed between right and left limbs [Citation26]. Similarly, the more premature and severe atherosclerosis in lower limbs than in upper limbs [Citation16] could explain the superiority of ILSBPD against IASBPD in a Primary Care population. However, a spectrum effect leading to low sensitivities of ILSBPD in very high cardiovascular risk populations may be expected due to: (1) the presence of bilateral oscillometric errors (with ILSBPD = 0 mmHg) caused by bilateral severe PAD and (2) the presence of PAD, when the severity of the disease is comparable in both lower limbs. Hence, ILSBPD may perform better in Primary Care populations than in Vascular Service populations.
This study has some limitations that must be considered. Firstly, we used Doppler ABI as the reference standard. Although it is considered the non-invasive gold-standard, it has some limitations, especially regarding a lack of sensitivity [Citation27]. IASBPD and ILSBPD should be ideally compared with digital subtraction angiography; however, this technique is invasive and may be ethically unjustifiable in a population with neither revascularization expectations nor very high cardiovascular burden. Secondly, it was impossible to blind the measurements between the oscillometer and Doppler, due to the fact that there was a single examiner; thus, diagnostic review bias could be expected. However, the analysis of the mean values of Doppler ABI, oscillometric ABI, IASBPD and ILSBPD and likelihood ratios did not show statistically significant differences between both groups according to the order of measurement. Thirdly, we used a technique based in four automated devices working at the same time, which avoids intra-observer bias and most of the variability in sequential SBP measurements due to short-term fluctuations. However, our technique cannot warrant perfect simultaneity, especially due to beat to beat and respirophasic SBP fluctuations. Nevertheless, a previous meta-analysis suggests that simultaneous measurements with regular oscillometers can be appropriate to measure arm and ankle SBP [Citation28].
Conclusion
In a Primary Care population with ≥1 cardiovascular risk factors, ILSBPD showed acceptable diagnostic accuracy for PAD, whilst IASBPD accuracy was negligible. However, neither the addition of ILSBPD nor IASBPD improved the ability of oscillometric ABI to detect PAD. Thus, to detect PAD and individuals at high cardiovascular risk, oscillometric ABI seems to be preferable. ILSBPD could be useful when blood pressure measurements in upper limbs are not possible.
Supplemental_Chart_1_1_.docx
Download MS Word (20.5 KB)Acknowledgments
The authors thank M. Andrea Rodríguez-Pardo for English language assistance.
Disclosure statement
None declared.
References
- Diehm C, Schuster A, Allenberg JR, et al. High prevalence of peripheral arterial disease and co-morbidity in 6880 primary care patients: cross-sectional study. Atherosclerosis. 2004;172:95–105.
- Tendera M, Aboyans V, Bartelink ML, et al. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2851–2906.
- Fores Raurell R, Alzamora Sas MT, Baena Diez JM, et al. [Underdiagnosis of peripheral arterial disease in the Spanish population. ARTPER study]. Med Clin (Barc). 2010;135:306–309.
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary. Vasc Med. 2017;22:Np1–Np43.
- Clark CE, Campbell JL, Evans PH, et al. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens. 2006;20:923–931.
- Singh S, Sethi A, Singh M, et al. Simultaneously measured inter-arm and inter-leg systolic blood pressure differences and cardiovascular risk stratification: a systemic review and meta-analysis. JAm Soc Hypertens. 2015;9:640–650.
- Mansia G, De Backer G, Dominiczak A, et al. ESH-ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 2007;16:135–232.
- Williams B, Poulter NR, Brown MJ, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens. 2004;18:139–185.
- Aboyans V, Criqui MH, McDermott MM, et al. The vital prognosis of subclavian stenosis. J Am Coll Cardiol. 2007;49:1540–1545.
- Weinberg I, Gona P, O'Donnell CJ, et al. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. Am J Med. 2014;127:209–215.
- Verberk WJ, Kollias A, Stergiou GS. Automated oscillometric determination of the ankle-brachial index: a systematic review and meta-analysis. Hypertens Res. 2012;35:883–891.
- Herraiz-Adillo A, Cavero-Redondo I, Alvarez-Bueno C, Martinez-Vizcaino V, Pozuelo-Carrascosa DP, Notario-Pacheco B. The accuracy of an oscillometric ankle-brachial index in the diagnosis of lower limb peripheral arterial disease: a systematic review and meta-analysis. Int J Clin Pract. 2017; (Epub 29 Aug 2017).
- Clark CE, Taylor RS, Shore AC, et al. Prevalence of systolic inter-arm differences in blood pressure for different primary care populations: systematic review and meta-analysis. Br J Gen Pract. 2016;66:e838–e847.
- Clark CE, Taylor RS, Shore AC, et al. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379:905–914.
- Clark CE, Taylor RS, Butcher I, et al. Inter-arm blood pressure difference and mortality: a cohort study in an asymptomatic primary care population at elevated cardiovascular risk. Br J Gen Pract. 2016;66:e297–e308.
- Shadman R, Criqui MH, Bundens WP, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44:618–623.
- Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. Clin Chem. 2015;61:1446–1452.
- Cohen JF, Korevaar DA, Gatsonis CA, et al. STARD for Abstracts: essential items for reporting diagnostic accuracy studies in journal or conference abstracts. BMJ. 2017;358:j3751
- World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194.
- Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol. 1991;44:763–770.
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41.
- Aboyans V, Criqui MH, Abraham P, et al. Measurement and interpretation of the Ankle-Brachial Index: a scientific statement from the American Heart Association. Circulation. 2012;126:2890–2909.
- DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845.
- Yin X, Wang J, Zheng W, et al. Diagnostic performance of coronary computed tomography angiography versus exercise electrocardiography for coronary artery disease: a systematic review and meta-analysis. J Thorac Dis. 2016;8:1688–1696.
- Guo H, Sun F, Tian Y. OS 09-05 the interankle systolic blood pressure difference is an independent risk indicator of prevalent stroke in chinese adults: a cross-sectional study. J Hypertens. 2016;34(Suppl 1):e71.
- Muller-Buhl U, Klimm HD. Bilaterality and symmetry of peripheral arterial occlusive disease. 2003; p. 100–104.
- Dachun X, Jue L, Liling Z, et al. Sensitivity and specificity of the ankle–brachial index to diagnose peripheral artery disease: a structured review. Vasc Med. 2010;15:361–369.
- Verberk WJ, Kessels AG, Thien T. Blood pressure measurement method and inter-arm differences: a meta-analysis. Am J Hypertens. 2011;24:1201–1208.
