Abstract
Purpose: This observational study investigated the association between serum osteocalcin level and blood pressure in a Chinese population.
Materials and methods: A total of 2241 subjects (909 men and 1,332 women; age, 24–78 years) from Shanghai communities were recruited. Subjects were divided into non-hypertensive and hypertensive groups according to diagnosis of hypertension based on the 1999 World Health Organization-International Society of Hypertension Guidelines. Serum osteocalcin levels were measured using an electrochemiluminescence immunoassay.
Results: Men in the hypertensive group showed lower serum osteocalcin level compared with those in the non-hypertensive group, [16.37 (13.34–20.11) ng/mL versus 17.01 (14.23–20.79) ng/mL, p = .039]. No difference in serum osteocalcin level was found between the two groups of women (p = .675). An inverse association was observed between serum osteocalcin level and systolic blood pressure (SBP) in men (p = .004), but serum osteocalcin level was not associated with diastolic blood pressure (DBP) in men (p = .472). No associations were detected between serum osteocalcin level and SBP or DBP in women (SBP: p = .108; DBP: p = .575). A multiple stepwise regression analysis showed an inverse association between serum osteocalcin level and SBP in men after adjusting for age, smoking status, family history of hypertension, and lipid and C-reactive protein levels (standardized β = –0.074, p = .023), but the association disappeared after adjustment for body mass index, waist circumference, blood glucose, and homeostasis model assessment of insulin resistance (p = .327).
Conclusions: Serum osteocalcin level was not independently associated with blood pressure in a Chinese population.
Introduction
Cardiovascular disease (CVD) is one of the most important diseases endangering health worldwide [Citation1]. High blood pressure has a close causal relationship with CVD. Each 20-mmHg increase in systolic blood pressure (SBP) or 10-mmHg increase in diastolic blood pressure (DBP) is associated with a greater than twofold increased risk of cardiovascular death, beginning at 115 mmHg SBP and 75 mmHg DBP [Citation2]. More than 290 million Chinese suffer from CVD, of whom 270 million suffer from hypertension, and nearly 2 million die prematurely due to high blood pressure each year [Citation3]. The pathogenesis of hypertension has not been completely clarified. Activation of sympathetic nervous system activity and the renin-angiotensin-aldosterone system are established mechanisms of hypertension; however, metabolic abnormalities closely correlated with inflammation have recently been recognized as trigger mechanisms for hypertension. Metabolic disorders can directly damage vessel endothelium, which has a profound effect on blood pressure through arterial sclerosis and vascular remodelling by inflammation and oxidative stress. Cytokines involved in energy metabolism and inflammatory pathways play a key role in the development of hypertension [Citation4].
Osteocalcin is a protein expressed and secreted into the blood by osteoblasts; it participates in the regulation of energy and in glucose and lipid metabolism [Citation5]. Osteocalcin is closely related to insulin resistance and is involved in the development of obesity, diabetes mellitus, and dyslipidaemia through common metabolic pathways [Citation6–8]. However, the relationship between serum osteocalcin level and blood pressure remains unclear. A cross-sectional study reported that the prevalence of hypertension increased gradually with a decrease in serum osteocalcin level [Citation9]. Another study found that serum osteocalcin level was inversely correlated with SBP and DBP [Citation10]. In contrast, Choi et al. found no association between serum osteocalcin level and SBP or DBP [Citation11]. These studies yielded inconsistent results, and no study has focused on the association between blood pressure and serum osteocalcin level in a Chinese population. Therefore, this study recruited subjects from Shanghai communities to explore the relationship between serum osteocalcin level and blood pressure.
Materials and methods
Subjects
Subjects were recruited from Shanghai communities between November 2013 and July 2014. All participants were instructed to complete a standardized questionnaire, including a history of present and past illnesses and medical therapies. Additionally, subjects taking any medication known to influence bone metabolism, those having a history of malignant tumours, and those with obvious liver, kidney, or thyroid dysfunction were excluded. Subjects in an active infectious condition were also excluded. Finally, 2241 participants with complete eligible data were enrolled in the study. This study protocol was approved by the Ethics Committee of Shanghai Jiao Tong University-Affiliated Sixth People’s Hospital, and all participants provided written informed consent.
Anthropometric and laboratory measurements
Subjects underwent a complete physical examination, including measurements of height, weight, and waist circumference (W). The standard measurement methods were described previously [Citation7]. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. After the subjects had been at rest for at least 10 min, blood pressure was measured with a mercury sphygmomanometer. Blood pressure was calculated as the mean of three measurements taken at 3-min intervals.
After a 10-hour overnight fast, blood samples were collected to measure fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), serum fasting insulin (FINS), serum total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), C-reactive protein (CRP), and osteocalcin levels. Subjects without a validated history of diabetes provided a 2-hour plasma glucose (2hPG) blood sample following a 75-g oral glucose tolerance test; subjects with diabetes underwent a 100-g carbohydrate (steamed bread meal) test to provide a 2hPG blood sample. The laboratory measurements were described previously [Citation7]. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as FINS (mU/L) × FPG (mmol/L)/22.5. Serum osteocalcin levels were measured using an electrochemiluminescence immunoassay (Roche Diagnostics, GmbH, Mannheim, Germany) on a Roche Elecsys 2010 (Elecsys module) immunoassay analyser. The intra–assay and inter–assay coefficients of variation 1.2% to 4.0% and 1.7% to 6.5%, respectively [Citation6].
Diagnostic criteria for hypertension and smoking
Based on the 1999 World Health Organization-International Society of Hypertension Guidelines, hypertension was defined as SBP ≥140 mm Hg and/or DBP ≥90 mm Hg, or receiving an antihypertensive treatment [Citation12]. Current smoking was defined as at least one cigarette per day for over half a year [Citation7].
Statistical analyses
All statistical analyses were performed using SPSS (Statistical Package for the Social Sciences) for Windows, Version 17.0 (SPSS Inc, Chicago, IL, USA). Data with a skewed distribution are presented as median with interquartile range (25–75%). The Wilcoxon rank-sum test for skewed variables was used to compare clinical parameters between the non-hypertensive and hypertensive groups. The χ2 test was used to compare categorical variables between the two groups. Spearman correlation analysis was conducted to determine the associations between blood pressure and the clinical parameters. Multiple stepwise regression analysis was performed to assess these associations after adjusting for potentially confounding factors. Two-tailed p-values <.05 were considered significant.
Results
Characteristics of the study participants
A total of 909 men and 1332 women [median age, 58.6(53.4–63.3) years; range, 24–78 years] were enrolled. The clinical characteristics of the study subjects are shown in . Subjects with hypertension were older and had higher BMI, W, SBP, DBP, FPG, 2hPG, HbA1c, FINS, HOMA–IR, TG, and CRP compared with those in the non-hypertensive group (all p < .01). The proportions of subjects with a family history of hypertension and of those who smoked, who received antidiabetic therapy, and who received lipid-lowering therapy were higher in the hypertensive than in the non-hypertensive group (all p < .05). However, the HDL-C level was lower in the hypertensive than in the non-hypertensive group (p < .01). No difference in the TC or LDL-C level was observed between the two groups (both p > .05).
Table 1. Clinical characteristics of study subjects stratified by hypertension.
Comparison of serum osteocalcin level between the groups
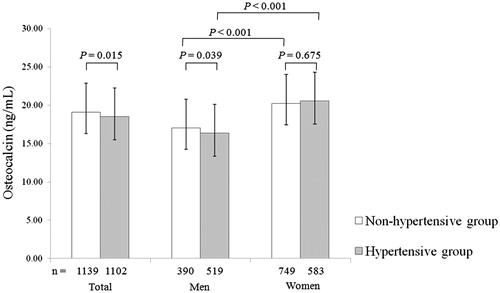
Overall, the serum osteocalcin level was lower in men than that in women [16.68 (13.66–20.46) ng/mL versus 20.42 (16.07–25.28) ng/mL, p < .01]. Serum osteocalcin level was lower in men than women in both groups (p < .01). Additionally, the serum osteocalcin level in men was lower in the hypertensive group than in the non-hypertensive group [16.37 (13.34–20.11) ng/mL versus 17.01 (14.23–20.79) ng/mL, p = .039], whereas the serum osteocalcin level in women did not differ between the groups [20.57 (16.22–25.00) ng/mL versus 20.22 (15.82–25.45) ng/mL, p = .675] ().
Association of serum osteocalcin level with SBP and DBP
Spearman’s correlation analysis revealed a significant negative correlation between the serum osteocalcin level and SBP in men (r = –0.095, p = .004). SBP was also positively correlated with age, BMI, W, FPG, 2hPG, HbA1c, FINS, HOMA-IR, TC, LDL-C, and CRP (all p < .05–0.01), (). However, the serum osteocalcin level was not associated with DBP (r = –0.024, p = .472) in men. No significant association was found between serum osteocalcin level and blood pressure in women (SBP: r = 0.044, p = .108; DBP: r = 0.015, p = .575).
Table 2. Correlations of SBP with various clinical and biochemical parameters in men.
To evaluate the independent relationship between serum osteocalcin level and SBP in men, we performed a stepwise multivariate regression analysis, in which SBP was designated as the dependent variable in three different models. In model 1, age, smoking status, family history of hypertension, antihypertensive therapy (angiotensin converting enzyme inhibitors, angiotensin receptor antagonists, β blockers, diuretics), antidiabetic therapy, lipid-lowering therapy (statins, fibrates) and serum osteocalcin level was assessed as independent variables. In this model, the serum osteocalcin level was independently associated with SBP (standardized β = –0.068, p = .038). The association between serum osteocalcin level and SBP remained in model 2 after adjusting for TC, LDL-C, and CRP (standardized β = –0.065, p = .046). However, in model 3, serum osteocalcin level was not associated with SBP, but age, BMI, 2hPG, antihypertensive therapy and family history of hypertension were independently associated with SBP after adjusting for BMI, W, FPG, 2hPG, HbA1c, and HOMA–IR (all p < .05, ).
Table 3. Multiple stepwise regression analysis showing the variables independently associated with SBP in men.
Discussion
The present study investigated the relationship between serum osteocalcin level and blood pressure in a Chinese population. No correlation was detected between serum osteocalcin level and blood pressure in women, whereas serum osteocalcin level and SBP were negatively correlated in men; however, this relationship disappeared after adjusting for multiple confounding factors.
Bezerra et al. reported a lower serum osteocalcin level in subjects with hypertension than in those without hypertension in a Brazilian study of 58 subjects (p = .013) [Citation13]. A simple correlation between serum osteocalcin level and SBP was found, but no correlation was observed between serum osteocalcin level and DBP [Citation13]. A Korean study of 114 men showed a lower serum osteocalcin level in the hypertensive group compared with the non-hypertensive group, but the serum osteocalcin level was not associated with SBP or DBP in men [Citation11]. The possible explanations for the inconsistent results include differences in populations and the small sample size of the studies. Another explanation may be that gender affects serum osteocalcin level. The present study included community individuals who were further divided according to gender in examining the association of serum osteocalcin level with blood pressure. We found only men in the hypertensive group had a lower serum osteocalcin level compared with those in the non-hypertensive group. Serum osteocalcin has a simple negative correlation with SBP, not with DBP in men. However, serum osteocalcin was not an independent risk marker for blood pressure after adjusting for blood glucose and body fat in men.
The correlation between osteocalcin and blood pressure is in line with a recent cross-sectional study performed in a total of 5647 Chinese individuals aged 45 years or older. The study demonstrated that the association of common polymorphism rs1800247 in osteocalcin gene with hypertension was affected by its interaction with HOMA-IR [Citation14]. Compared with the carriers of TT genotype, the carriers of CC genotype were associated with a decreased odds of hypertension, but this association was not significant in the subgroup with HOMA-IR >1.93 [Citation14]. Another study was controversial with above studies, performed in Italy, showing that serum osteocalcin was positively correlated with SBP in a cohort of 298 patients affected by overweight and obese, or hypertension, or both hypertension and type 2 diabetes [Citation15]. The correlation remained significant after adjusting for BMI, HbA1c and HDL–C. However, this correlation might be influenced by the use of drugs for hypertension, which has the potentiality to normalize blood pressure levels [Citation15].
Serum osteocalcin is involved in regulating glucose and lipid metabolism, and is closely related with obesity and other metabolic abnormalities. We reported previously that a decreasing trend in serum osteocalcin level was accompanied by increased visceral fat in 1,768 Chinese men [Citation7], and serum osteocalcin level was an independent risk marker for abdominal obesity [Citation7]. Lee et al. demonstrated that osteocalcin stimulates adiponectin, an insulin–sensitizing adipokine, in adipocytes [Citation16]. Thus, correcting the levels of free fatty acids and TG can lead to weight loss and a further protective effect against metabolic disturbances [Citation17]. Our previous study showed that serum osteocalcin level was inversely associated with hypertension after adjusting for age, smoking status, and CRP in 1,789 postmenopausal women [Citation7]. However, we found no relationship between osteocalcin and hypertension after further adjustment for central obesity, hyperglycaemia, and hypertriglyceridaemia [Citation7]. In the present study, serum osteocalcin level was independently associated with SBP when age, smoking status, family history of hypertension, drug treatment and serum osteocalcin level were assessed as independent variables in a model. The association remained after further adjustment for lipids and CRP. However, serum osteocalcin level was not correlated with SBP after eliminating the effects of blood glucose, BMI, and W. Thus, osteocalcin may have an indirect protective effect on elevated blood pressure, mediated by body fat and glucose metabolism.
Hypertension is strongly associated with endothelial function. Endothelial dysfunction induces the expression of vasoactive substances, which causes dysfunctional contraction or dilation of vessels to raise blood pressure. Osteocalcin is an osteoblast-derived protein that affects energy metabolism and improves endothelial function [Citation18–21]. Our previous animal study showed that exogenous osteocalcin administered to ApoE–KO mice fed a high fat diet for 12 weeks had a significant effect in reducing the mean blood pressure level and enhancing vascular endothelium-dependent relaxation of the aortic arch [Citation20]. Osteocalcin may have an endothelial-protective effect by mediating the phosphoinositide 3-kinase/Akt/endothelial nitric oxide synthase signalling pathway [Citation22]. Osteocalcin had beneficial effects in protecting human aortic endothelial cells from damage by free fatty acids via the insulin signalling pathway [Citation19].
We reported an independent relationship between serum osteocalcin level and carotid intima media thickness (C-IMT) in 1,319 postmenopausal women [Citation23]. However, the association between serum osteocalcin level and vascular disease might be weakened after eliminating metabolic factors. Following the study noted above, we controlled for the influence of blood glucose, lipids, and blood pressure, and found that serum osteocalcin level was not independently correlated with C-IMT in a metabolically healthy Chinese population [Citation24]. In agreement with that study, we also found that daily injections of osteocalcin were not associated with endothelium-dependent relaxation in mice eating a chow diet [Citation22].
The limitation in the present study was it only included subjects from Shanghai communities, and the results may have been affected by population and regional variables.
The present study found that serum osteocalcin level was not independently correlated with blood pressure in a Chinese population.
Disclosure statement
The authors declare no conflicts of interest.
Additional information
Funding
References
- van den Hoogen PC, Feskens EJ, Nagelkerke NJ, et al. The relation between blood pressure and mortality due to coronary heart disease among men in different parts of the world. Seven Countries Study Research Group. N Engl J Med. 2000;342:1–8.
- Lewington S, Clarke R, Qizilbash N, Prospective Studies Collaboration, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913.
- Yusuf S, Rangarajan S, Teo K, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371:818–827.
- Liao MH, Shih CC, Tsao CM, et al. RhoA/Rho-kinase and nitric oxide in vascular reactivity in rats with endotoxaemia. PLoS One. 2013;8:e56331
- Kindblom JM, Ohlsson C, Ljunggren O, et al. Plasma osteocalcin is inversely related to fat mass and plasma glucose in elderly Swedish men. J Bone Miner Res. 2009;24:785–791.
- Zhou M, Ma X, Li H, et al. Serum osteocalcin concentrations in relation to glucose and lipid metabolism in Chinese individuals. Eur J Endocrinol. 2009;161:723–729.
- Bao Y, Ma X, Yang R, et al. Inverse relationship between serum osteocalcin levels and visceral fat area in Chinese men. J Clin Endocrinol Metab. 2013;98:345–351.
- Bao Y, Zhou M, Lu Z, et al. Serum levels of osteocalcin are inversely associated with the metabolic syndrome and the severity of coronary artery disease in Chinese men. Clin Endocrinol (Oxf). 2011;75:196–201.
- Yang R, Ma X, Pan X, et al. Serum osteocalcin levels in relation to metabolic syndrome in Chinese postmenopausal women. Menopause. 2013;20:548–553.
- Pérez-Castrillón JL, Justo I, Silva J, et al. Bone mass and bone modelling markers in hypertensive postmenopausal women. J Hum Hypertens. 2003;17:107–110.
- Choi BH, Joo NS, Kim MJ, et al. Coronary artery calcification is associated with high serum concentration of undercarboxylated osteocalcin in asymptomatic Korean men. Clin Endocrinol. 2015;83:320–326.
- Kjeldsen SE, Farsang C, Sleigh P, et al. World Health Organization; International Society of Hypertension. 1999 WHO/ISH hypertension guidelines–highlights and esh update. J Hypertens. 2001;19:2285–2288.
- Bezerra dos Santos Magalhães K, Magalhães MM, Diniz ET, et al. Metabolic syndrome and central fat distribution are related to lower serum osteocalcin concentrations. Ann Nutr Metab. 2013;62:183–188.
- Ling Y, Gao X, Lin H, et al. A common polymorphism rs1800247 in osteocalcin gene is associated with hypertension and diastolic blood pressure levels: the Shanghai Changfeng study. J Hum Hypertens. 2016;30:679–684.
- De Pergola G, Triggiani V, Bartolomeo N, et al. Independent relationship of osteocalcin circulating levels with obesity, type 2 diabetes, hypertension, and HDL cholesterol. EMIDDT. 2016;16:270–275.
- Lee NK, Sowa H, Hinoi E, et al. Endocrine regulation of energy metabolism by the skeleton. Cell. 2007;130:456–469.
- Bullen JW Jr, Bluher S, Kelesidis T, et al. Regulation of adiponectin and its receptors in response to development of diet-induced obesity in mice. Am J Physiol Endocrinol Metab. 2007;292:E1079–E1086.
- Gössl M, Mödder UI, Atkinson EJ, et al. Osteocalcin expression by circulating endothelial progenitor cells in patients with coronary atherosclerosis. J Am Coll Cardiol. 2008;52:1314–1325.
- Flammer AJ, Gössl M, Widmer RJ, et al. Osteocalcin positive CD133+/CD34-/KDR + progenitor cells as an independent marker for unstable atherosclerosis. Eur Heart J. 2012;33:2963–2969.
- Fernández-Real JM, Izquierdo M, Ortega F, et al. The relationship of serum osteocalcin concentration to insulin secretion, sensitivity, and disposal with hypocaloric diet and resistance training. J Clin Endocrinol Metab. 2009;94:237–245.
- Kanazawa I, Yamaguchi T, Yamamoto M, et al. Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2009;94:45–49.
- Dou J, Li H, Ma X, et al. Osteocalcin attenuates high fat diet-induced impairment of endothelium-dependent relaxation through Akt/eNOS-dependent pathway. Cardiovasc Diabetol. 2014;13:74.
- Yang R, Ma X, Dou J, et al. Relationship between serum osteocalcin levels and carotid intima-media thickness in Chinese postmenopausal women. Menopause. 2013;20:1194–1199.
- Luo Y, Ma X, Hao Y, et al. Relationship between serum osteocalcin level and carotid intima-media thickness in a metabolically healthy Chinese population. Cardiovasc Diabetol. 2015;14:82.