Abstract
Aim: Tricuspid regurgitation (TR) with the maximum velocity >2.8m/s has been newly integrated into the diagnostic criteria for left ventricular (LV) diastolic dysfunction. Although the maximum velocity of TR within the normal range (TR < 2.8m/s) is frequently detected in hypertensive patients and is associated with enlarged left atrial (LA) volumes, the influence of TR < 2.8m/s on LV diastolic dysfunction remains unknown in uncomplicated hypertension.
Methods: Echocardiography was performed to assess the mitral annular velocity (e’), E/e’, LV mass, and LA phasic volumes and emptying fractions (total, passive, and active) in 100 patients with uncomplicated hypertension with TR within the normal range and in 77 of those without measurable TR. Patients were defined as having normal, inclusive, or dysfunction of LV diastolic function, according to how many parameters met the cut-off levels (maximum LA volume index >34ml/mm2, e’<7 cm/s, and E/e’>15). Pulmonary artery systolic pressure (PASP) was estimated by the formula; PASP =4 (maximum velocity of TR)2 + 5 mmHg.
Results: The maximum velocity of TR or PASP saw a positive correlation, and LA total or passive emptying fractions saw an inverse correlation with LV diastolic dysfunction in hypertensive patients with TR < 2.8. In contrast, pulse pressure and LV mass saw positive correlation in hypertensive patients without TR. A stepwise ordinal logistic regression analysis indicated that PASP and LA passive emptying fractions were associated with LV diastolic dysfunction in hypertensive patient with TR < 2.8m/s.
Conclusion: The presence of TR may be related to the development of LV diastolic dysfunction in hypertensive patients with TR <2.8m/s.
Introduction
Tricuspid regurgitation (TR), utilized for estimating pulmonary artery systolic pressure (PASP), has been recognized as a risk factor in patients with left sided heart diseases such as heart failure with preserved left ventricular (LV) systolic function [Citation1]. Recently, the diagnostic criteria for LV diastolic dysfunction with normal LV ejection fraction has been updated, and for the first time, the presence of TR >2.8m/s has been regarded as being pathophysiological, and integrated into the diagnostic criteria [Citation2].
Although TR within the normal range (TR < 2.8m/s) is frequently detected even in routine echocardiography of patients without significant left-sided heart diseases, however, the involvement of TR within the normal range in the development of LV diastolic dysfunction remains unclear in hypertensive patients without significant heart diseases. Indeed, a general population with very low prevalence of heart failure and coronary artery disease showed that measurable PASP was detected in 69% of a total of 2042 subjects with a median PASP of 26 mmHg (equivalent with TR of 2.3 m/s) [Citation3]. Furthermore, a clinical study revealed that TR was detected in 71% of 450 patients with uncomplicated hypertension, and a majority of them (n = 255, 69%) had the maximum velocity of TR < 2.5 m/s [Citation4].
In addition, TR within the normal range (<2.8m/s) can affect left ventricular diastolic properties including left atrial (LA) volume, as identified in the clinical study of hypertensive patients, the maximum velocity of TR was independently related to age, LV morphology and LV filling pressure [Citation4].
Left atrial volume is a key indicator for LV diastolic dysfunction with normal ejection fraction [Citation5], and plays a major role in maintaining optimal cardiac output and can react to increased LV filling pressure [Citation6]. LA volume consists of 3 phases; reservoir, conduit, and booster pump volumes [Citation6]; The reservoir volume is governed by pulmonary vein inflow during early ventricular systole, the conduit volume is determined by pulmonary vein inflow during early ventricular diastole, and the booster function reflects atrial contractility during late ventricular diastole to augment ventricular filling [Citation7]. These left atrial phasic volumes could be altered in patients with hypertension [Citation8].
From these findings discussed above, we hypothesized that TR within the normal range may be associated with the development of LV diastolic dysfunction in uncomplicated hypertensive patients without significant heart diseases, possibly through interaction with LA phasic volume and/or function. To test this hypothesis, we compared echocardiographic parameters of LV diastolic properties and LA phasic volumes and functions in uncomplicated hypertensive patients with TR within the normal range (<2.8m/s) and those without measurable TR.
Methods
Study patient
Patients with uncomplicated hypertension were enrolled in this study from December 2013 to April 2017. They were outpatients who were on blood pressure lowering medications, and were referred to the unit of echocardiography to evaluate target organ damages due to hypertension. Prior to recruitment, we excluded patients with chronic atrial fibrillation. A total of 242 uncomplicated hypertensive patients on sinus rhythm were selected.
We excluded patients with systemic chronic illnesses that might affect pulmonary circulation such as chronic obstructive pulmonary disease, known collagen diseases such as rheumatoid arthritis, and malignant disorders (n = 11). Patients were also excluded if they had significant left-sided heart diseases such as previous myocardial infarction or cardiac surgery (n = 11), hypertrophic cardiomyopathy (n = 2), aortic valve stenosis with aortic jet velocity >2.5 m/s (n = 1), or mitral regurgitation of greater than moderate degree (n = 35). Even in the absence of these left sided heart diseases, patients with tricuspid regurgitation >2.8m/s (n = 5) were excluded as the possibility of pulmonary hypertension due to undiagnosed systemic disease could not be denied. Thus, a total of 65 patients were excluded, and there were 100 hypertensive patients with TR within the normal range (<2.8m/s) and the remaining 77 patients were without measurable TR.
The study protocol was in accordance with the Helsinki Declaration, and approved by the ethical committee of our hospital. Participants gave their informed consent.
Echocardiography
Participant of this study underwent transthoracic echocardiography using a commercially available instrument (Vivid 7, General Electric, Vingmed, Norway). Two-dimensional and M-mode measurements were made according to the recommendations of the American Society of Echocardiography. Peak aortic jet velocity was measured using pulse wave and continuous Doppler echocardiography. Aortic and mitral regurgitations were assessed by color Doppler imaging. Mild mitral regurgitation was determined if the color-flow area of mitral regurgitation was <20% of LA size on 4-chamber view [Citation9], and patients were excluded if they exceeded the cut-off level.
The presence or absence of TR was examined with a special care by scanning the parasternal short axis views and the apical four chamber view. The maximal TR velocity was assessed by continuous-wave Doppler. PASP was estimated by Doppler echocardiography from the systolic right ventricular to right atrial pressure gradient using the modified Bernoulli equation (4 times the peak tricuspid regurgitant velocity squared) [Citation10]. Right atrial pressure, assumed to be 5 mm Hg, was then added to the calculated gradient to yield PASP [Citation10], since the study participants were in the stable stage without significant left sided heart diseases.
Left ventricular diameter at diastole (LVDd), left ventricular diameter at systole (LVDs), interventricular septal diameter (IVS) and left ventricular posterior wall thickness at diastole (LVWT) were measured. Left ventricular mass was calculated using an anatomically validated formula recommended by the American Society of Echocardiography [Citation11]. Left ventricular mass = 1.04 × 0.8 × [LVDd + IVS + LVWT)3 – (LVDd)3] and indexed by body surface area (LV mass index g/m2).
The early peak mitral peak flow velocity (E) and the late diastolic peak flow velocity (A) by pulse wave Doppler, and the early diastolic mitral annular velocity (e’) by tissue Doppler imaging were recorded. In the present study, we regarded the ratio of E/e’ as an index of LV filling pressure [Citation12], e’ as an index of the LV early relaxation or LV stiffness [Citation13]. For the assessment of right ventricular systolic function, right ventricular contours were traced at end-diastole and at end-systole to calculate two dimensional fractional area change (%) on the apical four chamber view [Citation14].
Left atrial (LA) volume was calculated using biplane area-length method as previously described [Citation15]: LA volume = (0.85 × 4-chamber × 2-chamber area/[4-chamber length + 2-chamber length/2], and indexed by body surface area (BSA).
LA volumes were measured at 3 different points; at the end of ventricular systole (Maximum LA volume), just before atrial contraction (LA volume before atrial contraction), and at the end of ventricular diastole (Minimum LA volume). From these LA volumes at 3 different time points, the following parameters of atrial phasic volume and function were calculated and indexed by body surface area as follows:
LA total emptying volume = maximum LA volume – minimum LA volume
LA passive emptying volume = maximum LA volume – LA volume before atrial contraction (reservoir volume)
LA active emptying volume = LA volume before atrial contraction – minimum LA volume (booster pump volume)
LA conduit volume = LV stroke volume – LA total emptying volume.
LA total emptying fraction = LA total emptying volume/maximum LA volume
LA passive emptying fraction= (maximum LA volume – LA volume before atrial contraction)/maximum LA volume
LA active emptying fraction = (LA volume before atrial contraction – minimum LA volume)/LA volume before atrial contraction
Echocardiograms were recorded by a sonographer, and these measurements above were performed by single experienced echo-cardiologist. The intra-observer reproducibility was tested using Bland-Altman method. There was no significant difference between 2 independent measurements. Mean difference of LA volume and 95% CI = 1.17 and −0.61 to 2.97. Intraclass correlation coefficient =0.952. The off-line analysis of echocardiography was performed using a software EchoPAC PC (General Electric, Vingmed, Norway).
Blood pressure measuring
Brachial blood pressure was measured using sphygmomanometer at sitting position. Since arterial stiffness [Citation16] and pulse pressure [Citation17] were involved in the development of LV diastolic dysfunction in mild hypertension, parameters of arterial load were also examined. Pulse pressure was calculated as systolic blood pressure (SBP) – diastolic blood pressure (DBP). Systemic arterial compliance was calculated as stroke volume indexed by body surface area divided by right brachial pulse pressure, as previously validated [Citation18].
Assessment of serum biomarkers and estimation of glomerular filtration rate
Blood samples were drawn to measure BNP (Shionoria, Shionogi, Japan) and creatinine. BNP (Shionoria, Shionogi, Japan using radio immune assay) was measured by chemiluminescent enzyme immunoassay using a Lumipulse G1200 analyzer (Fuji Rebio, Japan). Creatinine was measured by enzymatic assays, on a TBA 120 FR analyzer (Toshiba).
Glomerular filtration rate (GFR) was estimated using the Modification of Diet in Renal Disease (MDRD) equation: we adopted the format of MDRD equation with a constant of 175 that is traceable to an isotope dilution mass spectrometry (ID-MS) [Citation19]. Matsuo et al. reported that the new Japanese coefficient was 0.808 (95% confidence interval, 0.728 to 0.829) for this IDMS-MDRD Study equation [Citation20]. Estimated GFR (ml/min/1.73 m2) = 175 × [serum creatinine]−154 × [age]−0.203 ×0.742 (if female) × 0.808 (race factor). Body surface area (BSA) was calculated using DeBois and DeBois method as described in the report by Devereux et al. [Citation21]: BSA = 0.007184 × [height 0.725] × [weight 0.425].
Statistical analysis
Data was expressed as means ± standard deviation. P < 0.05 was regarded as being statistically significant. The distribution of BNP was rightly skewed, then the variable was log-transformed for further analysis.
Hypertensive patients with within the normal range (<2.8m/s) and those without measurable TR, respectively, were divided into 3 categories consisting of normal diastolic function, inconclusive, and diastolic dysfunction according to the updated diagnostic criteria for the evaluation of LV diastolic dysfunction by echocardiography [Citation2]. The presence of left ventricular dysfunction was defined if more than half of these parameters met the cut-off values; septal E/e’ ≧15, septal e’ <7 cm/s, LA volume/BSA >34 ml/mm2, and tricuspid regurgitation >2.8 m/s. (However, in this study, patients with tricuspid regurgitation >2.8m/s were excluded). Patient was defined as inconclusive if the half of these parameters met the cut-off values, and was regarded as normal if more than half of these parameters did not meet the cut-off values.
Comparisons between patients with LV diastolic dysfunction and those without LV diastolic dysfunction either in 100 hypertensive patients with TR within the normal range (<2.8m/s) or in 77 of those without measurable TR were determined using non parametric Willcoxon’s rank sum test for continuous variables, and chi-square analysis for categorical variables.
Comparisons between normal diastolic function, inclusive function, and LV diastolic dysfunction were also investigated using non parametric Kruskal Wallis test for continuous variables, and chi-square analysis for categorical variables.
A correlation with LV diastolic dysfunction was defined when each parameter had an increase or decrease in a stepwise manner with statistically significance. Post-hoc test was performed using Willcoxon’s test with P < 0.01.
Since this study was of an exploratory design, sample size was not calculated prior to the initiation of this study. However, we preformed post–hoc power calculation with α error =0.05, β error =0.2. Two-sided P < 0.05 was considered to be significant. The statistical power for maximum TR regurgitant velocity was 0.85 (the minimum number of patients 55), and that for LA total emptying fraction was 0.855(the minimum number of patients 56) in hypertensive patients with TR within the normal range (<2.8m/s). The statistical power for LV mass/BSA was 0.88 (the minimum number of patients 39) and that for GFR was 1.00 (the minimum number of patients 14) in hypertensive patients without measurable TR. Our sample populations were 100 of hypertensive patients with TR within the normal range (<2.8m/s), and 77 of those without measurable TR. Both of them met the minimum number of patients required for each analysis.
Since our sample size (clinical outcome) was not large enough to implement multivariate logistic regression analysis, we performed stepwise ordinal logistic regression analysis with forward selection, entering the three categories of LV diastolic function (none, inclusive, and dysfunction) as the dependent variable. Demographic or clinical factors were chosen as explanatory variables which saw a correlation with LV diastolic dysfunction. Age, gender, log PASP, passive LA emptying fraction, GFR, and log BNP were selected as explanatory variables in hypertensive patients with TR within the normal range (<2.8m/s). As for hypertensive patients without measurable TR, we entered age, gender, pulse pressure, LV mass/BSA, GFR, log BNP as explanatory variables in the same model.
The JMP version 9 (SAS institute, Cary, NC, USA) statistical package was used for data analyses.
Results
Comparisons of clinical and echocardiographic findings between hypertensive patients with TR within the normal range (<2.8m/s) and hypertensive patients without measurable TR
provides comparisons of clinical and echocardiographic findings between hypertensive patients with TR within the normal range (<2.8m/s) and those without measurable TR. Hypertensive patients with TR within the normal range (<2.8m/s) had higher levels of LV stroke volume/BSA and conduit volume/BSA, and BNP levels than those without measurable TR. As for vascular properties, pulse pressure levels were not different between the two groups, but systemic arterial compliance (LV stroke volume/BSA/pulse pressure) was higher in hypertensive patients with TR within the normal range (<2.8m/s) than in those without measurable TR.
Table 1. Clinical characteristics and Left ventricular diastolic dysfunction in hypertensive patients without TR and hypertensive patients with TR within normal range (<2.8m/s).
In spite of these differences in LV volume load and arterial compliance between the two groups, there were no differences in the prevalence of LV diastolic dysfunction defined by the criteria between hypertensive patients with TR within the normal range (<2.8m/s) (10.0%) and those without measurable TR (15.5%). Moreover, the prevalence of E/e’ >15, e’ <7, or maximum LA volume/BSA >34, as well as LA phasic volumes and functions, saw no difference between the two groups.
Comparisons of LV diastolic properties between hypertensive patients with TR within the normal range (<2.8m/s) and in those without measurable TR
summarized comparisons among 3 groups classified by the diagnostic criteria for LV diastolic dysfunction either in hypertensive patients with TR within the normal range (<2.8m/s) or in hypertensive patients without measurable TR. There were no differences in the use of ACEI/ARB, calcium channel blocker, and β blockers among the three groups (none, inclusive, dysfunction) classified by the diagnostic criteria for LV diastolic dysfunction either in hypertensive patients without measurable TR nor in those with TR within the normal range (<2.8m/s). We do not prescribe thiazide or diuretics routinely to patients without heart failure, therefore, there were no patients on diuretics in the current study. The prevalence of severe hypertension, defined by the use of more than 2 different types of anti-hypertensive medication to achieve the optimal BP levels, was also not different among the three groups.
Table 2. Clinical characteristics and echocardiographic findings of hypertensive patients with TR within normal range (<2.8 m/s) classified by the diagnostic criteria for LV diastolic dysfunction.
Table 3. A: Stepwise ordinal logistic regression analysis in hypertensive patients without measurable TR.
B: Stepwise ordinal logistic regression analysis in hypertensive patients with TR within the normal range (2.8m/s).
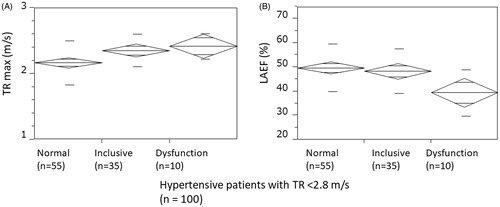
BNP levels were associated with a positive correlation with LV diastolic dysfunction in both two groups. In hypertensive patients with TR within the normal range (<2.8m/s), LA active volume/BSA, the maximum velocity of TR (), and PASP showed a positive correlation with LV diastolic dysfunction, while LA total emptying fraction () and in LA passive emptying fraction revealed an inverse correlation with LV diastolic dysfunction.
Figure 1 (A) Mean (diagonal box) and standard deviation (horizontal bar) of the maximum velocity of tricuspid regurgitation among 3 groups of patients classified by the criteria for LV diastolic dysfunction (normal, inclusive, or dysfunction) in hypertensive patients with TR within normal range (<2.8m/s). The maximum velocity of tricuspid regurgitation saw a positive correlation with LV diastolic dysfunction. (P < 0.05 by non parametric Willcoxon’s rank sum test.). (B). Mean (diagonal box) and standard deviation (horizontal bar) of total LA emptying fraction (LAEF) among 3 groups of patients classified by the criteria for LV diastolic dysfunction (normal, inclusive, or dysfunction) in hypertensive patients with TR within normal range (<2.8m/s). LA total emptying fraction saw an inverse correlation with LV diastolic dysfunction. (P < 0.05 by non parametric Willcoxon?s rank sum.
In contrast, older age, higher pulse pressure, lower GFR, and higher LV mass/BSA saw a correlation with LV diastolic dysfunction, but none of LA phasic volumes and functions indicated a correlation with LV diastolic dysfunction in hypertensive patients without measurable TR.
The stepwise ordinal logistic regression analysis revealed that PASP, log BNP, and LA passive emptying fraction were associated with LV diastolic dysfunction in hypertensive patients with TR within the normal range (<2.8m/s) (), whereas GFR, LV mass/BSA, and log BNP were selected as the determinants in hypertensive patients without measurable TR ().
Discussion
The current study revealed three major findings; (1) Although the presence of tricuspid regurgitation (TR) within the normal range (<2.8m/s) did not interfere in the diagnostic criteria for LV diastolic dysfunction, the maximum velocity of TR showed a correlation with the progression of LV diastolic dysfunction in hypertensive patients with TR within the normal range (<2.8m/s). (2) In hypertensive patients with TR within the normal range (<2.8m/s), the LA total and passive emptying fractions (LA reservoir function) saw inverse correlation with LV diastolic dysfunction. (3) On the other hand, pulse pressure (arterial load), higher LV mass (hypertrophy), and lower GFR (renal dysfunction) were related to the trend in hypertensive patients without TR.
From these findings, it could be hypothesized that the presence of TR in the normal range (PASP <35mmHg or TR <2.8m/s) may be associated with impaired LA contractile function, which leads to the development of LV diastolic dysfunction.
Tricuspid regurgitation within the normal range (<2.8m/s) is associated with LV diastolic dysfunction in uncomplicated hypertension
Tricuspid regurgitation within the normal range (<2.8m/s) appears to have a considerable clinical impact, since it was prevalent in a study of general population [Citation3] and also in a clinical study of patients with mild hypertension [Citation4]. The current study indicated that the maximum velocity of TR (or pulmonary artery systolic pressure estimated by TR = PASP) levels showed a correlation with LV diastolic dysfunction in hypertensive patients with TR within the normal range (2.8m/s).
This finding suggests that elevated PASP may be closely related to elevation in LV filling pressure (E/e’) and/or enlargement of LA volumes even in hypertensive patients with TR within the normal range (or the absence of pulmonary hypertension). In general, PASP is determined by the amount of blood flowing through the pulmonary vessels (cardiac output), the intrinsic properties of the vasculature (resistance, compliance, and impedance), and the left atrial pressure downstream of the pulmonary circuit (left ventricular diastolic pressure and left atrial compliance) [Citation3].
Indeed, the result of current study is compatible with the previous study of general population which indicated PASP below the range of pulmonary hypertension (median and IQR = 26, 24 -30 mm Hg in PASP, or corresponding to =2, 2.17-2.5 m/s in TR) could be dependent on pulse pressure (arterial stiffness or LV afterload), E/e’ (LV filling pressure), and the left atrial pressure downstream of the pulmonary circuit (left ventricular diastolic pressure and left atrial compliance) [Citation3].
Nevertheless, the prevalence of LV diastolic dysfunction, consisting of E/e’>15, e’ <7, and LA volume/BSA > 34, was not different between hypertensive patients with TR within the normal range (<2.8m/s) and those without TR. This discrepancy is likely to be due to the fact that there was no distinction of PASP levels between patients with inclusive dysfunction and patients with LV diastolic dysfunction, but PASP levels in both of them were greater than that in patients with normal function.
Renal impairment, arterial load, and LV hypertrophy may contribute to the development of LV diastolic dysfunction in hypertensive patients without measurable TR
In contrast to hypertensive patients with TR within the normal range (<2.8m/s), hypertensive patients without measurable TR had a correlation with LV diastolic dysfunction in older age, female gender, higher levels of pulse pressure and LV mass, or reduced levels of GFR. These findings were compatible with the results of previous studies regarding the relationship between LV diastolic dysfunction and arterial stiffness; Pulse pressure, as a marker of arterial stiffness [Citation22], correlated positively with LA volume in hypertensive patients [Citation23], and was related to LV mass in older population with isolated hypertension [Citation24]. The association between pulse pressure/cardiac index (an inverse ratio of systemic arterial compliance) with LV diastolic dysfunction was noted in patients with reduced GFR (chronic kidney disease) [Citation25]. From findings above, it could be presumed that LV diastolic dysfunction may develop at the stage where LV can no longer accommodate the burden of afterload produced by arterial stiffness and renal impairment in hypertensive patients without measurable TR.
Diminished LA early diastolic (reservoir) function may contribute to the development of LV diastolic dysfunction in hypertensive patients with TR <2.8m/s
In the current study, both LA total emptying fraction and LA passive emptying fraction had a correlation with LV diastolic dysfunction in hypertensive patients with TR within the normal rage (<2.8m/s). In a stepwise ordinal logistic regression analysis, LA passive emptying fraction, PASP, and log BNP were associated with a correlation with LV diastolic dysfunction. The finding suggests that LA early diastolic contractile function may be diminished in parallel with the progression of LV diastolic dysfunction independent of neuro-hormonal activation, as LA remodeling is related to LV remodeling [Citation6]. Otherwise, it would be possible that LA contractile function decreases in the presence of severe LA dilation when the optimal Frank-Starling relationship is exceeded [Citation6]
Study limitation
A previous study indicated that systolic BP and pulse pressure were predictors of the future development of LV diastolic dysfunction in a middle-aged hypertensive population [Citation26]. However, anti-hypertensive medication could modify the influence of higher blood pressure on LV diastolic function [Citation27]. As far as our study is concerned, anti-hypertensive medication does not seem to influence the prevalence of LV diastolic dysfunction. Nevertheless, the effect of blood pressure lowering on the LV diastolic function remains unknown [Citation28]. Therefore, a prospective study would be warranted to compare the effect of blood pressure lowering on LV diastolic properties between hypertensive patients with TR within the normal range and those without measurable TR.
Clinical implication
Our proposal for clinical practice would be as follows; the coexistence of TR within the normal range (<2.8m/s) may serve as a marker for the future incidence of LV diastolic dysfunction in hypertensive patients. For such patients, it would be beneficial to repeat echocardiography for early detection of LV diastolic dysfunction. These patients with TR would require intensive treatment for lowering blood pressure to the optimal level, in order to prevent the deterioration of LV diastolic function.
Conclusions
In hypertensive patients with tricuspid regurgitation within the normal range (<2.8m/s), the hemodynamic severity of TR (or PASP) was related to the transition of LV diastolic function from normal to dysfunction. Diminished LA passive emptying (early diastolic) function may be involved in this pathogenesis.
Acknowledgements
We thank Mr. James Apthorpe for his advice and help in editing English writing.
Disclosure statement
We have no conflict of interest
References
- Georgiopoulou VV, Kalogeropoulos AP, Borlaug BA, et al. Left ventricular dysfunction with pulmonary hypertension: Part 1: epidemiology, pathophysiology, and definitions. Circ Heart Fail. 2013;6:344–354.
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314.
- Lam CS, Borlaug BA, Kane GC, et al. Age-associated increases in pulmonary artery systolic pressure in the general population. Circulation. 2009;119:2663–2670.
- Abergel E, Tache A, Cohen A, et al. Determinants of right ventricular pressure in mild hypertension. J Hypertens. 2001;19:2055–2061.
- Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–133.
- Rosca M, Lancellotti P, Popescu BA, et al. Left atrial function: pathophysiology, echocardiographic assessment, and clinical applications. Heart. 2011;97:1982–1989.
- Hoit BD. Left atrial size and function: role in prognosis. J Am Coll Cardiol. 2014;63:493–505.
- Eshoo S, Ross DL, Thomas L. Impact of mild hypertension on left atrial size and function. Circ Cardiovasc Imaging. 2009;2:93–99.
- Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16:777–1802.
- Lam CS, Roger VL, Rodeheffer RJ, et al. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009;53:1119–1126.
- Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463.
- Nagueh SF, Middleton KJ, Kopelen HA, et al. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30:1527–1533.
- Paulus WJ, Tschope C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–2550.
- Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713.
- Tsang TS, Barnes ME, Gersh BJ, et al. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002;90:1284–1289.
- Russo C, Jin Z, Palmieri V, et al. Arterial stiffness and wave reflection: sex differences and relationship with left ventricular diastolic function. Hypertension. 2012;60:362–368.
- Triantafyllidi H, Ikonomidis I, Lekakis J, et al. Pulse pressure determines left atrial enlargement in non-dipper patients with never-treated essential hypertension. J Hum Hypertens. 2007;21:897–899.
- Briand M, Dumesnil JG, Kadem L, et al. Reduced systemic arterial compliance impacts significantly on left ventricular afterload and function in aortic stenosis: implications for diagnosis and treatment. J Am Coll Cardiol. 2005;46:291–298.
- Vickery S, Stevens PE, Dalton RN, et al. Does the ID-MS traceable MDRD equation work and is it suitable for use with compensated Jaffe and enzymatic creatinine assays? Nephrol Dial Transplant. 2006;21:2439–2445.
- Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–992.
- Devereux RB, de Simone G, Arnett DK, et al. Normal limits in relation to age, body size and gender of two-dimensional echocardiographic aortic root dimensions in persons >/=15 years of age. Am J Cardiol. 2012;110:1189–1194.
- Safar ME, Plante GE, Mimran A. Arterial stiffness, pulse pressure, and the kidney. Am J Hypertens. 2015;28:561–569.
- Jaroch J, Rzyczkowska B, Bociaga Z, et al. Arterial-atrial coupling in untreated hypertension. Blood Press. 2015;24:72–78.
- Pini R, Cavallini MC, Bencini F, et al. Cardiac and vascular remodeling in older adults with borderline isolated systolic hypertension: the ICARe Dicomano Study. Hypertension. 2001;38:1372–1376.
- Lee WH, Hsu PC, Chu CY, et al. Associations of pulse pressure index with left ventricular filling pressure and diastolic dysfunction in patients with chronic kidney disease. Am J Hypertens. 2014;27:454–459.
- Perkiomaki JS, Mottonen M, Lumme J, et al. Predictors of development of echocardiographic left ventricular diastolic dysfunction in the subjects aged 40 to 59 years (from the Oulu Project Elucidating Risk of Atherosclerosis Study)). Am J Cardiol. 2015;116:1374–1378.
- Wachtell K, Bella JN, Rokkedal J, et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment: The Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) Study. Circulation. 2002;105:1071–1076.
- Palmieri V, Russo C, Bella JN. Treatment of isolated left ventricular diastolic dysfunction in hypertension: reaching blood pressure target matters. Hypertension. 2010;55:224–225.
