Abstract
Objective: We aimed to evaluate the prevalence, determinants and clinical impact of masked hypertension in offspring of patients with diabetes. Masked hypertension was defined according to guidelines as daytime ambulatory blood pressure monitoring “ABPM” ≥135/85 mmHg and clinic BP <140/90 mmHg.
Methods: 100 nondiabetic offspring of patients with diabetes and 60 offspring of healthy people were enrolled; 24-h ABPM was applied to evaluate mean 24-h systolic/diastolic blood pressure “BP”, daytime, nighttime and night dipping readings. Left ventricular parameters and coronary flow reserve of the left anterior descending artery (induced by adenosine 0.14 mg/kg/min) was calculated in all offspring.
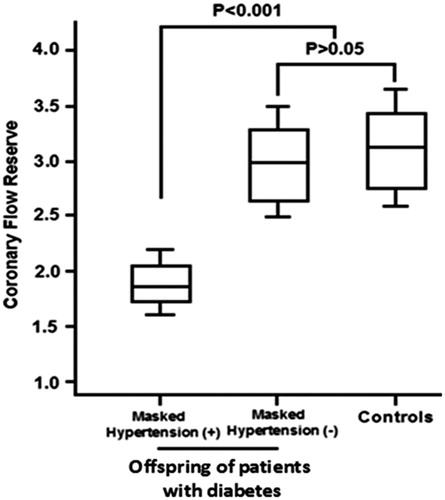
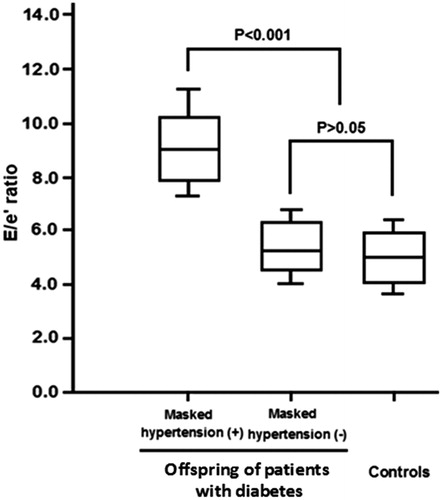
Results: 29% of offspring of patients with diabetes had masked hypertension compared to only 3.3% offspring in healthy people (p < 0.001). Compared with those without masked hypertension, offspring with masked hypertension had a significantly reduced coronary flow reserve (p < 0.001), significantly higher E/e' (p < 0.01), [a surrogate marker of left ventricular filling pressure], more microalbuminuria (p < 0.01), and higher values of high-sensitive C-reactive protein “CRP” (p < 0.001). Multivariate regression analysis showed that, fasting blood glucose, and high-sensitive CRP, were independently associated with masked hypertension, whilst daytime systolic BP and non-dipping systolic BP were the strongest predictors for masked hypertension. Logistic regression analysis revealed that masked hypertension was independently associated with reduced coronary flow reserve (p < 0.0001) and diastolic dysfunction (p < 0.001).
Conclusion: Masked hypertension is prevalent in offspring of patients with diabetes and significantly associated with reduced coronary flow reserve and left ventricular diastolic dysfunction. These findings suggest that offspring of patients with diabetes constitute a high risk group and deserve close follow up, mainly with the use of ABPM.
Introduction
Ambulatory blood pressure monitoring may add important information beyond office blood pressure measurement in patients with hypertension and diabetes [Citation1–3]. Nonetheless, scarce data are available as regard the prevalence of masked hypertension in offspring of patients with diabetes. Moreover, whether offspring of patients with diabetes with masked hypertension had impaired coronary circulation and cardiac function is not clearly studied and the clinical significance of masked hypertension in offspring of patients with diabetes is not well documented. Therefore, we investigated the prevalence of masked hypertension in offspring of patients with diabetes and examined its association with coronary circulation and left ventricular function.
Methods
Study population
This is a case-control study where we enrolled 100 nondiabetic offspring of patients with diabetes (49.6 ± 7.5 years old, 65% males) and 60 nondiabetic healthy offspring (controls) who had parents without “a known diagnosis of diabetes” with matched age and sex. Patients with a previous history of hypertension or were on antihypertensive medications, with coronary artery diseases, renal diseases, inflammatory diseases and people with history of diabetes or antidiabetic medications, or taking statins were excluded.
24-h ABPM
24-h ABPM was performed using a Spacelabs-90207 automatic cuff-oscillometric devices (Spacelabs, Inc. Redmond, WA, USA). The individuals were oriented to keep their regular activities and make a report discriminating the hours of each activity. For the purpose of ABPM, two different periods were defined. The daytime period was defined as the time period from 10:00 am to 8:00 pm, and nighttime was defined as a time period from midnight to 6:00 am. In addition, all readings obtained from 8 am until 8 pm, and from 8 pm until 8 am were obtained averaged to calculate mean 24-h BP readings. Measures of systolic BP higher than 260 mmHg and diastolic BP higher than 150 mmHg were excluded. The limit to detection of heart rate was between 200 and 20 bpm. The examination was accepted if at least 75% of the measures in 24 h were successfully executed. The nocturnal BP fall was calculated as ({diurnal systolic BP − nocturnal systolic BP} × 100/diurnal systolic BP). It was considered normal values of nocturnal systolic BP fall greater than 10% (dippers). Patients that showed pressure fall lower than this value were called “non-dippers”;. Systolic and diastolic brachial BP utilizing mercury sphygmomanometer were recorded as the average of two readings as previously recommended [Citation4]. Masked hypertension was defined by seated office BP <140/90 mmHg and daytime ABPM ≥135/85 mmHg. The absence of masked hypertension was defined as seated office BP <140/90 mmHg and ABPM BP <135/85 mmHg [Citation5].
Laboratory measurements
Fasting blood glucose was determined immediately before ingestion of 75 gram of glucose, followed 2 h later by determination of 2-h plasma glucose. Patients with fasting blood glucose >5.6 mmol/L fulfilled the criteria for impaired fasting glucose and those with 2-h oral glucose tolerance test level of 7.8–11.1 mmol/L fulfilled the criteria for impaired glucose tolerance based on the American Diabetes Association criteria. Total cholesterol, triglyceride, low density lipoprotein cholesterol and high-density lipoprotein cholesterol levels were determined by enzymatic methods using a Hitachi 7150 autoanalyzer (Hitachi, Tokyo).
Trans-thoracic echocardiographic examination
Two-dimensional, M-mode pulsed and color flow Doppler echocardiographic examinations (GE-Vivid 7; General Electric, Milwaukee, WI, USA) with a 2.5–5 MHz phased array transducer were performed. During echocardiography, continuous one-lead electrocardiographic recording was obtained. Left ventricular mass was calculated from end-diastolic M-mode or 2D-guided anatomic M-mode measurements of the ventricular septum, left ventricular internal diameter and posterior wall thickness, according to the method of Devereux, [Citation6] and indexed to height2.7 (g/m2.7; left ventricular mass index [Citation7]. Conventional and tissue Doppler interrogation of the mitral inflow and myocardial velocities was performed to assess diastolic mitral E, A waves and E/A ratio as well as septal mitral annulus to measure the peak systolic tissue velocity (S') and the early diastolic tissue velocity (e'). late diastolic tissue velocity (a'). E/e' ratio, the combination of mitral flow velocity and mitral annulus velocity, has been identified as the best parameter for diagnosis of diastolic dysfunction [Citation8].
Coronary flow reserve assessment
Coronary flow in the distal part of left anterior descending coronary artery was recorded with a high-resolution frequency transducer (5–7 MHz), guiding with color Doppler flow mapping, utilizing a sample volume (2.5 or 3.0 mm wide) positioned on the color signal in the left anterior descending. The resting baseline coronary flow was recorded first, followed by intra-venous adenosine, that was administered (0.14 mg/kg/min) to induce hyperemia and then spectral Doppler signals was recorded. The average of three cardiac cycles mean diastolic velocities were measured at baseline and peak hyperemic conditions from the Doppler signal recordings. Coronary flow reserve was defined as the ratio of hyperemic to basal mean diastolic velocities and a value <2.0 were considered pathological [Citation9,Citation10]. Inter- and intra-day variability of coronary flow reserve assessed by transthoracic color Doppler guided echocardiography has been evaluated and the variation in coronary flow reserve were 3.4% and 4.1% respectively.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments. The study protocol was approved by the clinical research ethics committees and an Informed consent was obtained from all individual participants included in the study.
Statistical analysis
Statistical analysis was performed by SPSS version 20 (SPSS Inc., Chicago, IL, USA). Data are presented as mean ± SD. Univariate correlates of a given variable were evaluated by least squares linear regression. For categorical variables count in percent is used. Distribution normality was assessed graphically. Separate multiple linear regression analyses were performed to study correlates of coronary flow reserve after adjusting for confounders [age, body mass index, family history of hypertension, smokers, clinic systolic and diastolic blood pressure, microalbuminuria, masked hypertension, nocturnal systolic blood pressure dipping, total cholesterol and triglycerides]. The null hypothesis was rejected at 2‐tailed p < 0.05.
Results
The demographic characteristics of offspring of patients with diabetes compared with control offspring are presented in . Family history of hypertension, smoking status, fasting blood glucose, and oral glucose tolerance test, were significantly different. 24-h ABPM demonstrated that 29 patients (29%) of the offspring of patients with diabetes had masked hypertension, versus two (3.3%) offspring only in the control group (p < 0.001). provides BP characteristics of offspring of patients with diabetes compared with control offspring. All ABPM parameters were significantly higher in offspring of patients with diabetes than control offspring, whilst the systolic and diastolic dipping were significantly lower (p < 0.001 and <0.05, respectively).
Table 1. Demographic characteristics of offspring of patients with diabetes versus offspring of non-diabetics (control).
Table 2. Blood pressure characteristics of offspring of patients with diabetes versus offspring non-diabetics (controls).
The comparison of echocardiographic characteristics between offspring of patients with diabetes and controls are presented in . Importantly the E/e' ratio was significantly higher in offspring of patients with diabetes than controls (p < 0.01). On the other hand, coronary flow reserve was significantly decreased in offspring of patients with diabetes than controls (p < 0.001).
Table 3. Echocardiographic characteristics of offspring of patients with diabetes versus control.
Offspring of patients with diabetes were furtherly subdivided into two subgroups: one group with masked hypertension (positive-MH) and another group without masked hypertension (negative-MH). lists the demographic data of offspring with masked hypertension compared with those without masked hypertension. We found that smoking (p < 0.03) fasting blood glucose level (p < 0.05), cholesterol level (p < 0.05), high- sensitive C-reactive protein (p < 0.001) and microalbuminuria (p < 0.01) were significantly higher in those with masked hypertension.
Table 4. Demographic characteristics of offspring of patients with diabetes with versus without masked hypertension.
BP characteristics of offspring with versus without masked hypertension are summarized in Table S1. Importantly offspring with masked hypertension had a significantly higher day and night systolic and diastolic BP (p < 0.01) as well as significantly higher nocturnal systolic non-dipping BP (p < 0.001). More so, offspring of patients with diabetes, who had masked hypertension had a significantly impaired left ventricular diastolic function [increased E/e' ratio] compared with those without masked hypertension (p < 0.01). Furthermore, coronary flow reserve was 1.83 ± 0.25 in offspring with masked hypertension, while it was 3.00 ± 0.29 in those without masked hypertension (p < 0.001) (Table S2).
We also found that coronary flow reserve in control group was significantly higher when compared with offspring with masked hypertension (p < 0.001); whilst it was comparable with offspring of patients with diabetes without masked hypertension (p > 0.05) ().
Figure 1. The coronary flow reserve in offspring of patients with diabetes with masked hypertension versus offspring without masked hypertension compared with control.
Meanwhile, the E/e' ratio was significantly higher in offspring of patients with diabetes with masked hypertension compared with offspring of patients with diabetes without masked hypertension and with control offspring (p < 0.001) ().
Figure 2. The E/e' ration value in offspring of patients with diabetes with masked hypertension versus offspring without masked hypertension.
With univariate regression analysis in offspring of patients with diabetes, the odds of having masked hypertension independently increased with family history of hypertension (p < 0.001), smoking (p < 0.01), high-sensitive C-reactive protein (p < 0.001), microalbuminuria (p < 0.05), fasting blood sugar (p < 0.003), left ventricular mass index (p < 0.01), E/e' ratio (p < 0.01) daytime systolic BP (p < 0.001) and nocturnal systolic dipping (p < 0.001). Whilst with multivariate analysis the presence of masked hypertension was independently and strongly predicted by daytime systolic BP (p < 0.001), nocturnal systolic dipping (p < 0.001) (Table S3).
Separate multiple linear regression analyses were performed to identify the determinants of CFR, and E/e' ratio. By these analyses, after adjusting for age, body mass index, smoking, total cholesterol, clinic systolic BP, nocturnal systolic non-dipping and masked hypertension, notably, masked hypertension was the strongest predictor associated with reduced coronary flow reserve (β coefficient = 0.59, p < 0.0001) and increased E/e' ratio (β coefficient = 0.29, p < 0.001) in offspring of patients with diabetes (Table S4).
Discussion
Our study shows a higher prevalence of masked hypertension in offspring of patients with diabetes compared with of parents without "a known diagnosis of diabetes”. Moreover, offspring of patients with diabetes had a reduced coronary flow reserve and left ventricular diastolic dysfunction (increased E/e; ratio) compared to control offspring. Notably, we found that even after adjustment for age, body mass index, family history of hypertension, smoking status, high-sensitive C-reactive protein, microalbuminuria, total cholesterol, masked hypertension was still significantly associated with impaired coronary flow reserve and diastolic dysfunction in offspring of patients with diabetes. More so, offspring with masked hypertension had a non-dipping systolic BP, higher C-reactive protein and cholesterol values compared with those without masked hypertension. Considered together, these findings suggest that there is a close association between masked hypertension and arterial fibrotic changes with increased wall stiffness.
Lurbe et al. [Citation11] demonstrated that, patients with masked hypertension had a higher ambulatory pulse rate, and were more than twice as likely to have a parental history of hypertension. Furthermore, patients with masked hypertension had an elevated nighttime BP and higher left ventricular mass compared to the normotensive controls, which suggest that on average their BP was truly elevated [Citation12]. The results showed that decreased nocturnal systolic BP dipping was significantly associated with the presence of masked hypertension. This may be explained by the assumption that offspring of patients with diabetes may have autonomic neuropathy as a result of chronic hyperglycemia. Foss et al. [Citation13] observed that the abnormal BP profile (the percentage change from day to night (Δ) of systolic BP and diastolic BP was significantly reduced) in offspring of patients with diabetes was associated with autonomic neuropathy.
Our study shows that smoking, high-sensitive C-reactive protein, fasting blood sugar, cholesterol level, daytime systolic BP and non-dipping nocturnal systolic BP were independently predictors associated with masked hypertension in offspring of patients with diabetes based on univariate analysis. On the other hand, fasting blood sugar, non-dipping nocturnal systolic BP, smoking and high- sensitive C-reactive protein were the independent predictors of masked hypertension in multivariate analysis.
Previous studies demonstrated that people with masked hypertension (68% men) had higher clinic BP, smoking, higher body mass index and higher levels of biomarkers reflecting adiposity, dyslipidemia, insulin resistance, and inflammation [Citation14].
Our study demonstrated that offspring with masked hypertension had a significant lower coronary flow reserve compared with those without masked hypertension. The synergism between masked hypertension and the presence of high blood glucose concentrations are the mix able to impair vascular endothelium in its function, thus predisposing to arterial fibrotic changes, with subsequent microvascular and cardiac dysfunction [Citation15]. These arguments suggest that masked hypertension in offspring of patients with diabetes may be related to endothelial dysfunction, inflammatory reaction and morphological structure alteration due to hyperglycemia.
We observed that E/e' ratio (a surrogate marker of left ventricular diastolic function) was significantly increased in offspring with masked hypertension compared with those without masked hypertension. These observations suggest that a clustering impact of masked hypertension and reduced coronary flow reserve on the myocardial function even in asymptomatic offspring of patients with diabetes.
Conclusion
The findings from the current study could provide novel insights into the association between masked hypertension and coronary flow and cardiac function in offspring of patients with diabetes. Masked hypertension is prevalent in offspring of patients with diabetes and it is associated with impaired coronary flow and left ventricular diastolic dysfunction. Family history of hypertension, high-sensitive C-reactive protein, microalbuminuria and non-dipping nocturnal systolic BP are independent predictors of masked hypertension in offspring of patients with diabetes. These results suggest a possible link between masked hypertension and other risk factors, putting offspring of patients with diabetes at high risk and prevail the importance of ABPM in risk stratification in offspring of patients with diabetes.
Suplemental_file.docx
Download MS Word (22.2 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. Br Med J. 2000;321:412–419.
- Turner, RC; Holman, RR; Matthews, DR, et al. Hypertension in Diabetes Study (HDS): II. Increased risk of cardiovascular complications in hypertensive type 2 diabetic patients. J Hypertens. 1993;11:319–325.
- Dolan E, Thijs L, Li Y, et al. Ambulatory arterial siffness index as a predictor of cardiovascular mortality in the Dublin Outcome Study. Hypertension. 2006;47:365–70.
- Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. The JNC 7 report. JAMA. 2003;289:2560–2572.
- Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24:52–58.
- Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458.
- de Simone G, Daniels SR, Devereux RB, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20:1251–1260.
- Kasner M, Westermann D, Steendijk P, et al. Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Doppler-conductance catheterization study. Circulation. 2007;116:637–647
- Hozumi T, Yoshida K, Ogata Y, et al. Noninvasive assessment of significant left anterior descending coronary artery stenosis by coronary flow velocity reserve with transthoracic color Doppler echocardiography. Circulation. 1998;97:1557–1562.
- Sicari R, Rigo F, Cortigiani L, et al. Additive prognostic value of coronary flow reserve in patients with chest pain syndrome and normal or near-normal coronary arteries. Am J Cardiol. 2009;103:626–31.
- Lurbe E, Torro I, Alvarez V, et al. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45:493–498.
- Diaz KM, Veerabhadrappa P, Brown MD, et al. Prevalence, determinants, and clinical significance of masked hypertension in a population-based sample of African Americans: the Jackson Heart Study. Am J Hypertens. 2015;28:900–908.
- Foss CH, Vestbo E, Froland A, et al. Autonomic neuropathy in nondiabetic offspring of type 2 diabetic subjects is associated with urinary albumin excretion rate and the ambulatory blood pressure. Diabetes. 2001;50:630–636.
- Brguljan-Hitij J, Thijs L, Li Y, et al; International database on ambulatory blood pressure in relation to cardiovascular outcome investigators. Risk stratification by ambulatory blood pressure monitoring across JNC classes of conventional blood pressure. Am J Hypertens. 2014;27:956–965.
- Thompson JES, Smith W, Ware LJ, et al. Masked hypertension and its associated cardiovascular risk in young individuals: the Africa-PREDICT study. Hypertens Res. 2016;39:158–165.
