Abstract
Purpose: Hypertension guidelines recommend measuring blood pressure (BP) on both arms, since an abnormal inter-arm difference (IAD) in BP is associated with an increased risk of vascular abnormalities and cardiovascular (CV) disease. We tested whether an automatic oscillometric BP monitor allowing simultaneous both arm BP measurement might be effective for screening of subjects with potential vascular disease.
Materials and methods: 220 consecutive subjects from an unselected sample of individuals of a small Italian community were screened using an automated upper-arm electronic BP monitor (Microlife WatchBP Office). Seated BP was measured in triplicate at 1 min interval. Demographic and clinical data were collected prior to any BP measurement. An average IAD difference >20 mmHg for systolic (S) and/or >10 mmHg for diastolic (D) BP was considered abnormal.
Results: In 9 subjects (4.1%) an abnormal IAD was found, with lower BPs measured in the non-dominant arm (147 ± 28/78 ± 9 vs. 154 ± 15/92 ± 11 mmHg dominant, p<.01). Subjects with a significant IAD were significantly older (71 ± 8 vs. 57 ± 15 years, p=.005), had a greater body mass index (BMI: 32 ± 7 vs. 25 ± 4 kg/m2, p=.0001), higher BP levels (154 ± 15/92 ± 11 vs. 133 ± 18/80 ± 10 mmHg, p=.001) and were more likely to report obesity (56 vs. 13%, p=.001), a history of hypertension (67 vs. 35%, p=.044) or cardiovascular disease (33 vs. 10%, p=.034) than subjects with normal IAD. In a multivariate analysis, a higher BMI [odds ratio (95% confidence interval): 1.29 (1.11, 1.51)] and SBP [1.06 (1.01, 1.10)] were significantly associated with a larger risk of an abnormal IAD (p=.001 and p=.012, respectively).
Conclusions: An abnormal IAD in BP is associated with a larger prevalence of CV risk factors and CV disease. Our study confirms that simultaneous both arm BP measurement must always be accomplished in subjects at risk for or with established CV disease.
Introduction
Simultaneous double arm blood pressure (BP) measurement is recommended by numerous guidelines to be performed at each first visit and an inter-arm difference (IAD) of at least 15–20 mmHg for systolic (S) BP and 10 mmHg for diastolic (D) BP is considered worth of further investigation [Citation1–5]. This is because significant IAD may indicate the presence of congenital heart disease, peripheral vascular disease, unilateral neurological, musculoskeletal abnormalities, or aortic dissection [Citation6]. However, also when IAD has no pathological background, double-arm measurement may still be important, as office measurements performed at the arm with the lowest BP can lead to a misdiagnosis and undertreatment of hypertension [Citation7]. In addition, to verify the effectiveness of antihypertensive therapy it is of clinical importance that BP is measured in the same arm on all sequential occasions. Despite the wide recognition of the importance of IAD assessment the methodology for its determination differs among guidelines or is not even reported. The lack of a clear description about the preferred method has led to a wide variation in IAD assessment, outcome and interpretation with undesirable consequences [Citation7]. For instance, it raised a debate about its usefulness as some questioned the relevance of the relationship between IAD and cardiovascular risk and claimed that overestimation of the IAD could lead to unnecessary referral to a specialist and cause an unnecessary burden for healthcare. Although, recent studies seem to have proven the relationship between IAD and cardiovascular risk [Citation6,Citation8,Citation9] it is out of question that more insight is needed, particularly on the best methodology to be used to assess IAD in BP.
As a matter of fact, although the importance of taking double arm measurement simultaneously is emphasized by guidelines, there is no univocal recommendation on how many measurements must be obtained and how to best perform the measurement. Considering that there is clinical evidence that a simultaneous method and repeated pairs of measurements avoids IAD overestimation [Citation7] clinical healthcare could benefit from a more structured recommendation. Multiple measurements may reduce the white coat effect and simultaneous measurement diminishes the effect of increased BP variability on mean level estimation due to sequential readings. In order to try to address the several open questions on the methodology and clinical impact of simultaneous double arm BP measurement, in the present study we tested whether an automatic oscillometric BP monitor allowing automated triplicate simultaneous BP measurements on both arms might be effective to simplify and make more feasible the assessment of IAD in the general population in order to make more effective the screening of subjects with potential vascular disease. The novelty of this study is the approach based on automated simultaneous BP measurement and the community setting where the measurements were collected.
Methods
Study design and participants
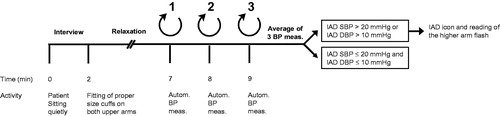
The study design envisaged a community-based screening campaign focusing on BP measurement and the collection of basic information on main cardiovascular risk factors. The study population consisted of an unselected sample of subjects aged ≥18 years, living in two small villages (Besnate and Solbiate Arno) in the Northern area of Italy, close to the city of Varese, in the Lombardy region. Examinations took place in mobile units located in the villages’ main squares. A questionnaire was administered to all subjects and BP was measured by non-healthcare operators, previously trained by a physician who coordinated and supervised all the on-field activities. The following information was collected in each subject: age, gender, height, body weight, family history for cardiovascular diseases, habits in relation to smoking and drinking, personal clinical history for cardiovascular diseases (ischemic heart disease, myocardial infarction, heart failure, stroke, peripheral artery disease or kidney disease), presence and treatment of arterial hypertension, diabetes mellitus and dyslipidaemia. At the end of the interview, BP was measured simultaneously at both upper arms by a validated, automatic, electronic sphygmomanometer (Microlife WatchBP Office AFIB, Microlife AG, Switzerland). Recommendations from current guidelines were followed [Citation1–3]. Three consecutive BP readings were taken at 1-minute interval time with the subject in the sitting position having rested for at least 5 minutes. Cuffs of the appropriate size for the subject’s upper arm were used (small size cuffs for upper arm circumferences between 17 and 22 cm, medium size cuffs for upper arm circumferences between 22 and 32 cm and large size cuffs for upper arm circumference between 32 and 42 cm). A sketch of the methodology employed for BP measurement is shown in .
Figure 1. Diagram summarizing the process of blood pressure (BP) measurement in the study. IAD: Inter-Arm Difference; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure.
The research was conducted according to the principles of the Declaration of Helsinki. Since this was a health awareness campaign no approval by any Ethics Committee was required according to the Italian regulations. Prior to the examination participants were asked to give written informed consent for the collection and anonymized analysis of their clinical data, according to the Italian Personal Data Protection Code. All visits took place between June 2013 and June 2015. The design of the study did not envisage any subjects’ follow-up.
All data collected at the time of the examination were recorded on a paper sheet. The individuals’ data were then entered in an electronic database to allow pooled analysis.
Statistical analysis
Data analysis was performed by grouping the subjects according to a normal or abnormal IAD (primary analysis) and according to a normal and significant IAD (secondary analysis). An abnormal IAD was defined when SBP was >20 mmHg and/or DBP >10 mmHg [Citation2,Citation3,Citation5]. A significant IAD was defined as ≥10 mmHg for either SBP or DBP [Citation1].
Other secondary analyses included: i) the abnormal IAD according to the dominant vs. non-dominant arm, ii) the prevalence of hypertension diagnosis according to the arm selected for the measurement (dominant vs. non-dominant, right vs. left). Given the observational nature of the study no sample size estimation was done. No methodology for replacing missing data was implemented since all subjects provided valid data. Main demographic and clinical data of each study subgroup were summarized by calculating the mean (±SD) in case of continuous variables and the absolute (n) and relative (%) frequency in case of categorical variables. Differences across groups were evaluated by analysis of variance or Chi-square test, depending on the type of variable. A stepwise forward logistic regression analysis was used by entering in the analysis IAD (normal vs. abnormal; non-significant vs. significant) as dependent variable and age, weight, body mass index (BMI), SBP and DBP, obesity (yes vs. no), known arterial hypertension (yes vs. no) and previous cardiovascular diseases (yes vs. no) as independent variables. Results were presented as odds ratio and 95% confidence interval. A linear regression analysis was run by entering as dependent variable continuous IAD and independent variables the same factors used for the logistic regression analysis. A p value of <.05 was considered significant. Data analysis was performed using IBM SPSS Statistics ver. 20 for Windows.
Results
Abnormal inter-arm difference in BP
A total of 220 subjects were enrolled: all of them provided the relevant information and were included in the analysis. In 9 (4.1%) subjects an abnormal IAD was detected. Absolute average IAD values were 5.0 ± 5.2 mmHg for SBP and 2.8 ± 3.4 mmHg for DBP, respectively. As expected the difference was larger for individuals with an abnormal IAD (15.0 ± 14.7/13.2 ± 7.7 mmHg vs. 4.6 ± 3.9/2.4 ± 2.2 mmHg normal IAD difference; p=.0001 for SBP and DBP).
Demographic, anthropometric and clinical data of the participants, grouped by normal and abnormal IAD are presented in . Subjects with an abnormal IAD were older (71.4 ± 8.4 vs. 56.9 ± 15.3 years, p=.005), had a greater BMI (31.6 ± 6.7 vs. 25.4 ± 4.0 kg/m2, p=.0001) and higher BP levels (154.1 ± 15.2/91.6 ± 10.9 vs. 133.4 ± 18.2/80.2 ± 9.8 mmHg; p=.001 for SBP and DBP), were more often obese (55.6 vs. 13.3%, p=.001) and were more likely to display a positive history for arterial hypertension (66.7 vs. 35.1%, p=.044) or cardiovascular disease (33.3 vs. 10.4%, p = 0.034) than those with a normal IAD.
Table 1. Demographic and clinical characteristics of the subjects enrolled in the study without or with abnormal inter-arm difference (IAD) in blood pressure (BP). P-values refer to the statistical significance of the difference between the two study subgroups. Abnormal IAD was defined as a SBP IAD >20 mmHg and/or a DBP IAD >10 mmHg.
When variables that resulted significantly different between the two study groups in the univariate analysis were entered in a stepwise forward logistic regression analysis, a larger BMI and a higher SBP were found significantly associated with a greater risk of an abnormal IAD (). The linear regression analysis considering IAD as a continuous rather than a category variable returned the same results: the BP level was significantly associated with the IAD level, whereas a history of cardiovascular disease was associated with a larger IAD for SBP and a large BMI or body weight with a larger IAD for DBP ().
Table 2. Results of the multivariate analyses testing the relationship between inter-arm difference (IAD) as a discrete variable or as a continuous variable with statistically significant determinants. Data are reported as odds ratio and 95% confidence interval for the logistic regression analysis (IAD as a discrete variable) and as regression coefficients and 95% confidence interval for the linear regression analysis (IAD a continuous variable).
Significant inter-arm difference in BP
There were 37 (16.8%) subjects who had an IAD ≥10 mmHg. These subjects were on average older (65.9 ± 12.9 vs. 55.9 ± 15.3 years, p=.0001), had a greater BMI (28.2 ± 5.6 vs. 25.1 ± 3.8 kg/m2, p=.001) and higher BP levels (149.2 ± 17.2/85.0 ± 11.9 vs. 131.2 ± 17.3/79.8 ± 9.5 mmHg; p=.0001 for SBP and p=.004 for DBP), were more often obese (35.1 vs. 10.9%, p=.001) and were more likely to display a positive history for arterial hypertension (54.1 vs. 32.8%, p=.014) than those with a normal IAD.
Similarly to what observed when subjects were categorized according to an abnormal IAD, the risk of a significant IAD increased in case of a larger BMI and a higher SBP in a multivariate analysis ().
Dominant vs. non-dominant arm
In the majority of subjects (209, 95.0%) the right arm was the dominant arm. In the whole sample, both SBP and DBP values were on average larger in the dominant than in the non-dominant arm, also when subjects were grouped by normal vs. abnormal IAD in BP, respectively ().
Figure 2. Blood pressure values in subjects without and with abnormal inter-arm difference (IAD) in blood pressure and in the whole study population. Data are presented as mean values and ± standard deviation for systolic (SBP) and diastolic blood pressure (DBP). P-values refer to the statistical significance of the difference between subjects without and with abnormal inter-arm blood pressure difference.
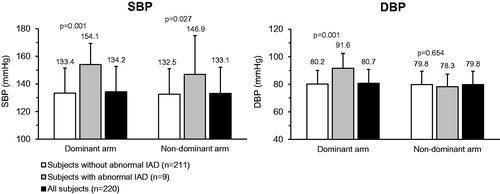
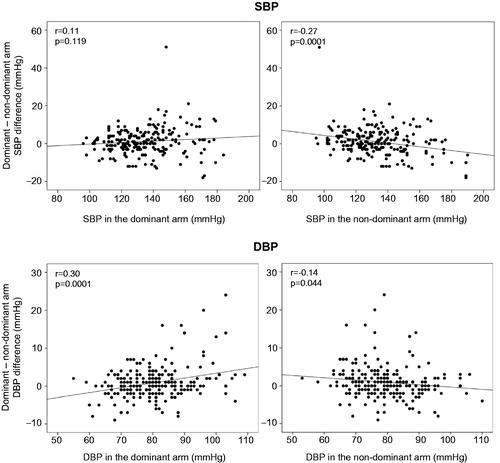
However, in one-third of subjects (38.6% SBP and 34.5% for DBP) the BP of the non-dominant arm prevailed on that of the dominant one. The difference in BP between the dominant vs. the non-dominant arm was positively related to the absolute level of BP in the dominant arm and negatively related to the absolute level of BP in the non-dominant arm ().
Figure 3. Scatterplots showing the relation between individual absolute values of systolic blood pressure (SBP) and diastolic blood pressure (DBP) in the dominant and non-dominant arm (x-axis) and the corresponding difference between the two arms (y-axis). Correlation coefficients (r) and p-values are reported for each comparison.
Definition of hypertension according to the measuring arm
In total there were 22 subjects who had normal BP (<140/90 mmHg) on one arm whereas BP on the other arm was elevated (SBP ≥140 or DBP ≥90 mmHg). When dominant vs. non-dominant arms were considered, 17 (7.7%) of subjects had elevated BP values on the dominant arm only and 5 (2.3%) on the non-dominant arm only. When the right vs. left arm was considered, 16 subjects (7.3%) had elevated BP on the right arm only and 6 (2.7%) on the left arm only. Sixty-nine (31.4%) subjects displayed elevated BP values on both arms.
On average SBP was slightly, but significantly (p=.038) higher in the right-arm (134.2 ± 18.7 mmHg) than in the left-arm (133.2 ± 18.9 mmHg), whereas DBP was almost identical in the two arms (80.4 ± 9.9 vs. 80.0 ± 9.9 mmHg, right vs. left arm, p=.169). In case of categorization according to dominant and non-dominant arm both SBP and DBP levels were slightly but significantly larger in the dominant arm (SBP: 134.2 ± 18.5 vs. 133.1 ± 19.1 mmHg, p=.026; DBP: 80.7 ± 10.1 vs. 79.8 ± 9.7 mmHg, p=.002).
Discussion
In the present study we tested the feasibility of simultaneous double arm automated blood pressure measurement for detection of potential upper arm vascular abnormalities in an unselected adult population in the community. Our approach was easily managed by trained non-healthcare operators and allowed detecting abnormal (>20 mmHg SBP and/or >10 mmHg DBP) IAD in 4% and significant (≥10 mmHg for either SBP or DBP) IAD in 17% of the screened subjects. Our results add to previous small case studies performed with the same automated device [Citation10–12] and suggest that the proposed screening model may be feasible and effective. They also confirm earlier findings that IAD is related to cardiovascular risk factors, thus being a predictor of cardiovascular events and associated with cardiovascular disease [Citation6,Citation9].
In addition, the fact that, in the present study, an abnormal IAD was generally due to lower BP values in the non-dominant arm recommends measuring BP always in both arms, at least in one occasion. This is emphasized by the fact that there were 22 subjects (10%) who had elevated BP (≥140/90 mmHg) in one arm but not in the other. Of these, 17 subjects (77%) had hypertensive values detected on the dominant arm. Based on the above findings one might consider measuring BP at the dominant instead of the non-dominant arm during routine clinical practice. Currently most doctors prefer to measure BP at the non-dominant arm [Citation5], which may lead to underestimation in BP, and according to our figure, may cause misdiagnosis of hypertension.
The present study should be seen within the context of its strengths and limitations. This is a population screening study and thus gives a good overall impression of the IADs within an Italian community and an unselected population. The measurements were performed according to the guidelines, using a validated BP monitor [Citation1,Citation2]. As the triple measurements are taken automatically the procedure is standardized and minimally influenced by observer bias. Although, the present study entails a community screening, it cannot be excluded that some sort of selection has taken place as those who are more aware of the importance of BP measurements (e.g. elderly or treated patients) are usually keener to participate to these surveys. As participants most likely did not expect that their BP would be measured that day, the preparation might not have been optimal in the sense that they might have been smoking, had a full bladder, just ate or drunk some coffee. On the other hand, subjects may have been less affected by a white coat effect that is partly triggered by a clinical environment. Previous accidents or arm injuries may have affected the accuracy of BP measurement and IAD in BP. Unfortunately we did not collect this information, though no subjects participating in this study spontaneously reported such abnormalities or were they visually evident. Finally, though we used appropriate cuff sizes for the arm of each individual we did not measure arm circumference or record the type of cuff used. Thus we could not assess the relation between arm circumference and IAD in BP.
The procedure of double-arm BP measurement has a significant influence on outcome [Citation7]. For instance, manual BP measurement led to a two times higher prevalence of significant IAD (≥10 mmHg) than when automated devices were used [Citation7]. A similar higher prevalence of significant IAD was seen for sequential measurement as compared to simultaneous measurement (relative risk 4.4 vs. 2.2) [Citation7]. In another study IAD assessed simultaneously with the same device used in our study was compared with IAD assessed with a manual device and measurements taken in sequential order [Citation10]. Results showed that the automated simultaneous method led to a lower average mean IAD (3.8 vs. 4.9 mmHg), a lower SD (3.1 vs. 4.1 mmHg) and a lower prevalence of IAD of more than 20 mmHg (3% vs. 9) than the sequential manual performance. Van der Hoeven et al. [Citation12] found in their study in 240 hospital patients that absolute systolic IADs were smaller for simultaneous (6.2 ± 6.7/3.3 ± 3.5 mm Hg) compared with sequential BP measurement (7.8 ± 7.3/4.6 ± 5.6 mm Hg, p<.01 for both). This led the authors to conclude that simultaneous BP measurement reduces the order effect, the first measurement is usually higher than the second, and therefore the average from plural simultaneous measurements is the preferred method for assessing IAD. This conclusion was confirmed by other studies [Citation7,Citation10], and indicates that simultaneous double-arm BP measurement would lead to less subjects being unnecessarily referred to a cardiovascular consultant for further investigation. In our study, BP measurements were automatically performed in triplicate with a device that complies with the guidelines [Citation13]. This means that the procedure is standardized and does not take extra efforts from the observer, except for the extra cuff position. Although clinical guidelines recommend double-arm measurement for a long time it is only since 2013 that simultaneous measurement is recommended [Citation1]. Finally, where others demonstrated that IAD assessed by mean of sequential BP measurement has poor reproducibility [Citation14] Krogager et al. found in their study among 339 hospital outpatients good reproducibility using the same double-cuff device employed in our study [Citation11]. In addition, the researchers concluded that a single set of simultaneous triplicate measurements using the device is sufficient for detecting an IAD of 10 mmHg or more [Citation11].
There were 22 subjects (10%) with elevated BP on one arm and normal BP on the other. Considered that most observers measure subjects at the non-dominant arm [Citation5] this would mean, for the current situation, that 17 (77%) of the 22 subjects were erroneously diagnosed as being normotensive. However, if these subjects would be measured at the dominant arm only the elevated BP value might lead to ABPM assignment which is generally performed at the non-dominant arm for practical reasons. It may not come as a surprise that the 22 subjects had an average systolic BP value that was close to the hypertension threshold value (141 mmHg). From a previous review in masked and white coat hypertension it was shown that those who have BP values around the threshold (i.e. 140 mmHg) are most vulnerable to erroneous diagnosis [Citation15].
Conclusion
The present study showed that abnormal and significant IADs found with an automated BP monitor taking triplicate simultaneous double-arm BP measurements are significantly related to several cardiovascular risk factors. Therefore, this approach is an effective tool to screen for potential vascular disease. Present data showed that 4% of an unselected adult population have an abnormal IAD indicating referral to a cardiovascular consultant. In addition,17% of the subjects had a significant IAD (≥10 mmHg) related to increased cardiovascular risk. The present study underscores the importance of performing double-arm measurements not only for revealing potential important cardiovascular risks factors but also for improving the diagnosis of hypertension in general. In the present study 10% of the subjects appeared to have elevated BP at one arm (commonly the dominant arm) but not the other. Not performing double arm measurement may therefore lead to a failure in detecting important cardiovascular risk factors, including the diagnosis of hypertension. For obtaining a reliable IAD it is recommended to perform measures at both arms simultaneously and determine the IAD from the average of multiple measurements. Finally, based on the results of the present study it might be considered to measure BP at the dominant arm instead of the generally preferred non-dominant arm for routine clinical BP measurement.
Disclosure of interest
SO received lecture fees from Colpharma Ltd., the Italian distributor of Microlife AG, and is scientific consultant of Biotechmed Ltd. provider of telemedicine services. WJV is an employee of Microlife AG.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available, but they are available from the corresponding author on reasonable request.
Acknowledgements
We are grateful for the logistic support provided by the following volunteers who helped collecting the data during the screening campaign: Lara Brianese, Armando De Falco, Edoardo Ghirardi, Daniela Ghiringhelli, Antonio Miranda, Andrea Niglia, Federica Pagliarin, Massimo Protasoni, Alberto Riganti, Andrea Zerbi.
Additional information
Funding
References
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104.
- Parati G, Omboni S, Palatini P, et al. Italian society of hypertension guidelines for conventional and automated blood pressure measurement in the office, at home and over 24 hours. High Blood Press Cardiovasc Prev. 2008;15(4):283–310.
- O'Brien E, Asmar R, Beilin L, et al. European society of hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21(5):821–848.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71(6):e13–e115.
- National Clinical Guideline Centre (UK). Hypertension: The clinical management of primary hypertension in adults: update of clinical guidelines 18 and 34 [Internet]. London: Royal College of Physicians (UK); 2011. Available from ttp://www.ncbi.nlm.nih.gov/books/NBK83274/
- Clark CE, Taylor RS, Shore AC, et al. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379(9819):905–914.
- Verberk WJ, Kessels AG, Thien T. Blood pressure measurement method and inter-arm differences: a meta-analysis. Am J Hypertens. 2011;24(11):1201–1208.
- Weinberg I, Gona P, O'Donnell CJ, et al. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. Am J Med. 2014;127(3):209–215.
- Clark CE, Campbell JL, Powell RJ. The interarm blood pressure difference as predictor of cardiovascular events in patients with hypertension in primary care: cohort study. J Hum Hypertens. 2007;21(8):633–638.
- Lohmann FW, Eckert S, Verberk WJ. Interarm differences in blood pressure should be determined by measuring both arms simultaneously with an automatic oscillometric device. Blood Press Monit. 2011;16(1):37–42.
- Krogager C, Laugesen E, Rossen NB, et al. Evaluation of interarm blood pressure differences using the Microlife WatchBP Office in a clinical setting. Blood Press Monit. 2017;22(3):161–165.
- van der Hoeven NV, Lodestijn S, Nanninga S, et al. Simultaneous compared with sequential blood pressure measurement results in smaller inter-arm blood pressure differences. J Clin Hypertens (Greenwich). 2013;15(11):839–844.
- Stergiou GS, Lin CW, Lin CM, et al. Automated device that complies with current guidelines for office blood pressure measurement: design and pilot application study of the Microlife WatchBP Office device. Blood Press Monit. 2008;13(4):231–235.
- Handler J, Zhao Y, Egan BM. Impact of the number of blood pressure measurements on blood pressure classification in U.S. adults: NHANES 1999–2008. J Clin Hypertens (Greenwich). 2012;14(11):751–759.
- Verberk WJ, Thien T, de Leeuw PW. Masked hypertension, a review of the literature. Blood Press Monit. 2007;12(4):267–273.
