Abstract
Purpose: Since the publication of the 2017 ACC/AHA hypertension guideline, few studies have analyzed the epidemiology and management of hypertension across many heterogeneous subgroups in the US.
Materials and Methods: We analyzed the data collected by the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2016. Participants greater than 20 years of age, who had valid blood pressure measurements, were included in the study. A comprehensive analysis of 14 population subgroups was done to systematically examine how hypertension awareness, treatment, and control varied by subpopulations.
Results: Our study included 45,557 participants with a mean age of 47.1 years, 48.3% were male and 51.7% were female. 47.8% participants had hypertension, of which 59.9% were aware of their diagnosis. Among the participants who were aware of their hypertension, 90.3% were prescribed medication(s) to lower blood pressure, of which 39.2% had achieved control. Multivariate analysis showed age, gender, Race/ethnicity, annual family income, education level, BMI, waist to height ratio, diabetes, and previous cardiovascular events to be independent risk factors for hypertension. Lower likelihoods of awareness and treatment were associated with male sex, younger age, Mexican ethnicity, participants without health insurance, absence of previous cardiovascular events, diabetes, obesity, or smoking. Overall, hypertension control rate was suboptimal across most of subgroups (<40%).
Conclusion: Based on the 2017 ACC/AHA guideline, almost half of the US adult population has hypertension. The suboptimal number of people with controlled blood pressure is pervasive in all subgroups and warrants greater efforts in prevention, as well as more effective treatment.
Introduction
Hypertension is a major risk factor for cardiovascular diseases. Blood pressure (BP) control is crucial in the prevention of adverse cardiovascular outcomes [Citation1]. As most hypertensive patients can be asymptomatic, timely and adequate prevention, detection, and control of hypertension poses an important public health challenge.
Since the 1960s, the National Health and Nutrition Examination Survey (NHANES), conducted by the National Center for Health Statistics, has been the principal means to track progress in preventing, treating, and controlling hypertension. It has also been the benchmark for the National High Blood Pressure Education Program and related health objectives for the nation [Citation2,Citation3]. Prior studies from national examination surveys demonstrated an increase in hypertension prevalence from 1988–1994 to 1999–2000, followed by stable prevalence from 1999–2000 to 2009–2010. Overall awareness, treatment, and control among adults with hypertension also improved during the same time interval [Citation4–7]. However, in the United States, hypertension has caused up to 50% of death from CHD, stroke, end stage renal disease (ESRD), as stated by various sources [Citation8–11].
In November 2017, the American College of Cardiology/American Heart Association Task Force (ACC/AHA) published the new guideline for high blood pressure in adults, which is an update of the “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure” (JNC 7) published in 2003 [Citation12]. According to the new guideline, one critical change is the new definition of hypertension where systolic blood pressure 130 mmHg or above and/or diastolic blood pressure 80 mmHg or above, is considered the new reference values for hypertension. Muntner and Colleagues evaluated the potential impact to U.S. population of the new 2017 guideline by utilizing data collection in NHANES from 2011 to 2014 in a recent article, which concluded “Compared with the JNC 7 guideline, the 2017 ACC/AHA guideline results in a substantial increase in the prevalence of hypertension but a small increase in the percentage of U.S. adults recommended antihypertensive medication” [Citation13]. To better understand the potential impact of the new guideline to different populations with various risk factors, we expanded data collection in NHANES from 1999 to 2016, and we analyzed the prevalence, awareness, and control of hypertension in 14 subgroups based on potential risk factors which may contribute to hypertension (age, gender, race, marital status, education, family income, previous cardiovascular event, diabetes, chronic kidney disease, body mass index (BMI), waist to height ratio, health insurance coverage, smoke history, and alcohol use).
Materials and methods
Participants
NHANES is a survey research program conducted by the Centers for Disease Control and Prevention to assess the health and nutritional status of adults and children in the United States. It is composed of cross-sectional, nationally representative health and nutrition surveys of the U.S. civilian, non-institutionalized population. In order to represent the U.S. population, a complex, stratified, multistage probability cluster sampling design is used in the survey. Selected subpopulations are oversampled, thereby providing a larger sub-sample size to yield more reliable estimates for these groups. The NHANES data are available to public online through the website of the Centers for Disease Control and Prevention of the United States (https://www.cdc.gov/nchs/nhanes).
In the current study, adult participants (≥20 years) from 1999 to 2016 who had valid blood pressure measurement were included. A total of 45,557 adult participants were available for full analyses. Informed consent was obtained from all participants by the NHANES in accordance with section 308(d) of the Public Health Service Act (42 U.S.C. 242m), and the protocol was approved by the institutional review board of the National Center for Health Statistics.
Data collection and variables
Blood pressure measurements were done in the mobile examination center by trained physicians following a standard protocol. Three consecutive BP readings are obtained from each participant after resting quietly in a seated position for 5 min. The systolic blood pressure (SBP) and diastolic blood pressure (DBP) averages in the NHANES examination section were calculated and used for identifying hypertension. If a BP measurement is interrupted or incomplete, a fourth attempt may be made. For more details on the procedures for measuring BP, please refer to the Physician Examination Procedures Manual located on the NHANES website. (https://wwwn.cdc.gov/Nchs/Data/Nhanes/2015-2016/Manuals/2015_Physician_Examination_Procedures_Manual.pdf)
Hypertension was defined as an average of SBP at least 130 mm Hg, or an average of DBP of at least 80 mmHg, or self-reported taking of medications for hypertension. Among hypertensive adults, hypertension awareness and treatment were defined as self-reported diagnosis of hypertension and taking prescription drugs for hypertension, respectively. Control was defined as an average of SBP less than 130 mm Hg and an average of DBP less than 80 mm Hg; participants not meeting these criteria were considered uncontrolled.
By exploring the NHANES data related to participants’ sociodemographic characteristics, health behaviors, and medical history, we evaluated previously mentioned 14 risk factors. BMI was calculated as weight in kilograms divided by height in meters squared. Waist to height ratio was calculated as waist circumference in centimeter divided by height in centimeter.
Statistical analysis
Our study estimated the prevalence of hypertension among all participants, as well as awareness, treatment, and control of hypertension among hypertensive participants. To systematically examine how the above varied by subpopulations, we did a comprehensive analysis of population subgroups. These were defined 14 selected characteristics: age (20–29, 30–39, 40–49, 50–59, 60–69, 70–79 or ≥ 80 years), gender (male or female), race/ethnicity (Mexican American, White or Black), marital status (Single/widowed/divorced/separated/never married or married/live with partner), education (elementary/middle school, high school or college and above), annual family income (<$20,000, $20,000–$44,999, $45,000–$74,999 or over $75,000), previous cardiovascular events (yes or no), diabetes (yes or no), chronic kidney disease (estimated glomerular filtration rate (eGFR) <30 mL/min/1.73 m2, 30 ≤ eGFR < 60 mL/min/1.73 m2, 60 ≤ eGFR < 90 mL/min/1.73 m2, or eGFR ≥ 90 mL/min/1.73 m2), BMI (BMI < 18.5 kg/m2, 18.5 ≤ BMI < 25 kg/m2, 25 ≤ BMI < 30 kg/m2 or BMI ≥ 30 kg/m2), waist to height ratio (ratio <0.5 or ratio ≥ 0.5), health insurance (yes or no), smoking history (smoked <100 cigarettes in life or smoked ≥100 cigarettes in life), alcohol use (had less than 12 alcohol drinks a year or had at least 12 alcohol drinks a year).
To account for the complex, stratified, multistage probability sampling design in the NHANES survey, SAS version 9.4’s (Cary, North Carolina) Procedural survey methodology was applied. Univariate analysis with Rao-Scott Chi-square test was conducted to identify potential significant factors; while multivariate logistic regression models were performed to assess the most important factors. A p-value of less than .05 was considered statistically significant.
Results
Our study included 45,557 adult participants with a mean age of 47.1 years. Among the participants, 21,999 (48.3%) were male with mean age at 46.3 years and 23,558 (51.7%) were female with mean age at 47.8 years.
Overall, based on the new 2017 guideline, 23,783 (47.8%) participants had hypertension. Multivariate analysis showed age, gender, Race/ethnicity, annual family income, education level, BMI, waist to height ratio, diabetes, and previous cardiovascular events to be independent risk factors for hypertension. More than half of the participants (59.9%, 15,039) with hypertension were aware of their diagnosis. Among the participants who were aware of their hypertension, 13,795 (90.3%) were prescribed medications to lower their blood pressure. Among those who were receiving anti-hypertensive medications, 4,813 (39.2%) participants’ blood pressure was well controlled under 130/80 mmHg ().
Table 1. Univariate analysis of individual characteristics associated with prevalence, awareness, treatment, and control of hypertension.
Age
Age is a strong variable associated with prevalence, awareness, treatment, and control of hypertension as analyzed in current study (). Multivariate analysis revealed that the odds ratio (OR) of hypertension prevalence increases about 6% for every 1 year increase in age (OR 1.06, 95% CI 1.06–1.07, p < .0001), the OR of awareness increases about 3% for every 1 year increase in age (OR 1.03, 95% CI 1.03–1.04, p < .0001), and the OR for those receiving treatment increases about 6% for every 1 year increase in age (OR 1.06, 95%CI 1.05–1.06, p < .0001). However, the OR of controlled hypertension while on treatment decreases about 1% for every 1-year increase in age (OR 0.99, 95% CI 0.99–0.99, p < .0001) ().
Figure 1. Prevalence, awareness, treatment, and control of hypertension among participants in different age group.
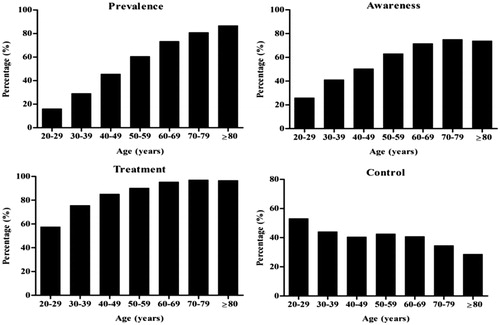
Table 2. Individual characteristics associated with prevalence, awareness, treatment, and control of hypertension.
Gender
Gender is significantly associated with prevalence, awareness and treatment of hypertension. Compared with adult females, adult males have significantly higher prevalence of hypertension (OR 1.59, 95% CI 1.47–1.71, p < .0001). They are less aware of their hypertension (OR 0.70, 95% CI 0.64–0.77, p < .0001) and less likely to receive anti-hypertensive treatment (OR 0.66, 95% CI 0.55–0.79, p < .0001). However, the overall control rate between male and female is not significantly different ().
Race/ethnicity
Race/ethnicity also plays an important role in hypertension. As compared with non-Hispanic Whites, Mexican-Americans are less likely to have hypertension (OR 0.71, 95% CI 0.66–0.77, p < .0001). Also, they are less aware of their hypertension (OR 0.77, 95% CI 0.71–0.84, p < .0001). Nevertheless, their treatment receiving rate and control rate are not significantly different compared with the non-Hispanic White group. Non-Hispanic Blacks have overall higher prevalence, awareness and are receiving more treatment for hypertension (OR 1.59, 95% CI 1.48–1.70, p < .0001, OR 1.45, 95% CI 1.36–1.55, p < .0001, and OR 1.40, 95% CI 1.22–1.60, p < .0001, respectively) as compared to non-Hispanic Whites. However, the overall control rate of hypertension for non-Hispanic Black is significantly lower as compared to non-Hispanic White (OR 0.81, 95% CI 0.75–0.88, p < .0001) ().
Education level
In our study, we found education level to be affecting the prevalence of hypertension. Those with college level education or above have less incidence of hypertension as compared to those with lower education level (OR 0.92, 95% CI 0.87–0.97, p = .0013). However, regardless of the education level, the awareness of the diagnosis and the chance to receive anti-hypertensive medications are the same for both groups. Interestingly, we found those with college or higher-level education, tend to have better control of their hypertension (OR 1.06, 95% CI 0.98–1.14, p = .1386) ().
Family income
There is higher prevalence and awareness of hypertension amongst families with annual income less than $20,000, as compared to families with higher annual income (more than $75,000) (OR 1.14, 95% CI 1.05–1.23, p = .0015, and OR 1.11, 95% CI 1.02–1.21, p = .0125, respectively). There is no significant difference in receiving anti-hypertensive treatment between these two groups. However, families with lower income had significantly lower hypertension control rate (OR 0.90, 95% CI 0.83–0.98, p = .0177) ().
Previous cardiovascular disease history
People with prior cardiovascular disease are more likely to be hypertensive; also they are more likely to be aware of their hypertension and receiving treatment as opposed to those without prior cardiovascular disease (OR 1.52, 95% CI 1.30–1.78, p < .0001, OR 3.08, 95% CI 2.66–3.56, p < .0001, and OR 2.06, 95% CI 1.50–2.81, p < .0001, respectively). However, the hypertension control rate is the same when compared to those with or without previous cardiovascular disease ().
Diabetes mellitus
Those with diabetes have significantly higher hypertension prevalence, awareness as well as treatment receiving rate as compared to the non-diabetic group (OR 1.79, 95% CI 1.38–2.31, p < .0001, OR 2.16, 95% CI 1.65–2.83, p < .0001, and OR 4.73, 95% CI 2.59–8.64, p < .0001, respectively). There is no difference observed regarding control rate ().
Obesity
Not surprisingly, obesity is closely correlated with hypertension. Using normal BMI (18.5 ≤ BMI <25 kg/m2) as reference, BMI ≥ 30 kg/m2 is significantly associated with increasing hypertension prevalence and awareness (OR 2.02, 95%CI 1.84–2.22, p < .0001 and OR 1.78, 95%CI 1.57–2.02, p < .0001, respectively), but not treatment and control rate. BMI < 18.5 kg/m2 is associated with significantly decreased hypertension prevalence when compared to normal BMI (OR 0.64, 95%CI 0.52–0.80, p < .0001). However, there is no difference regarding awareness, treatment and control rate. Noteworthy, there is no difference regarding prevalence, awareness, treatment and control rate between people who are overweight (25 ≤ BMI <30 kg/m2) and those with normal BMI ().
As another indicator for obesity, a waist to height ratio of equal or greater than 0.5 is associated with significantly higher hypertension prevalence and awareness (OR 1.36, 95% CI 1.20–1.53, p < .0001, and OR 1.38, 95% CI 1.17–1.64, p = .0002, respectively), however, there is no difference found regarding treatment and control rate ().
Health insurance
Our data showed people without health insurance are less aware of their hypertension when compared to those with insurance (OR 0.696, 95% CI 0.614–0.789, p < .0001). Nonetheless, there is no difference found for hypertension prevalence, as well as overall treatment and control rate between these two groups ().
Smoking status
According to NHANES, smokers were defined as those who self-reported as having smoked more than 100 cigarettes in their entire life, and non-smokers were those who self-reported as having smoked less than 100 cigarettes in their entire life. We found smokers to be more likely aware of their hypertension and to have better hypertension control rate as compared to non-smokers who have hypertension (OR 1.18, 95%CI 1.10–1.27, p < .0001, and OR 1.20, 95% CI 1.09–1.33, p = .0005, respectively). However, there is no difference in treatment receiving rate, and there is no difference regarding hypertension prevalence between these two groups ().
Others
Among aforementioned 14 selected characteristics, we found marital status, current kidney function and alcohol use not to be associated with hypertension prevalence, awareness, treatment or control in multivariate analysis.
Discussion
As Burnier and colleagues predicted in an editorial published on Blood Pressure in 2018, the 2017 ACC/AHA guideline could make major paradigm shifts regarding the prevalence, awareness, treatment and control of hypertension [Citation14]. According to our results, almost half of the US adult population has hypertension. Compared with recent reports from other countries, hypertension awareness and treatment receiving rates are high in US [Citation15,Citation16]. In general, 3 out of 5 people are aware of their hypertension, and 9 out 10 are receiving pharmaceutical treatment. However, only 2 out of 5 people who are hypertensive have their blood pressure under control while on medication(s).
Similar to a previous report [Citation17], we did observe that although the overall awareness and treatment of hypertension was lower among young adults compared with middle-aged or older adults, when treated, young adults were more likely to achieve blood pressure control. In fact, in subgroup analysis, the young adults between 20 and 29-years achieved more than 50% control rate. The best-tolerated and safest approach to controlling blood pressure in young adults may be lifestyle modifications, such as reduced sodium intake, weight loss and physical activity. However, our study suggests starting treatment earlier for young adults who fail lifestyle modifications, in order to achieve better blood pressure control. Also, better blood pressure control during young age may subsequently prevent more comorbidities resulting from long standing hypertension when those adults reach their middle or older age.
We also observed sex-related differences in prevalence, awareness, and treatment among US adults, with males having substantially higher prevalence of hypertension and lower awareness and treatment as compared to their female counterparts. However, higher awareness and treatment observed in females did not translate into better blood pressure control. Those differences could be partly due to higher number of clinic and/or hospital visits by females [Citation18,Citation19], which suggests that for males without access to care or infrequent preventive care visits, hypertension awareness, treatment, and control may only be improved outside of traditional clinical settings, such as school or worksite-based health screening [Citation20].
We observed the necessity to conduct more basic studies as well as more clinical trials pertaining to blood pressure control in African Americans. This subgroup has the highest prevalence, awareness and treatment rate compared to other race/ethnicities, however, their hypertension control rate remains the lowest. Our study also showed the low awareness in Mexican Americans is likely contributing to the overall lower treatment rate in this group of ethnicity. There is need to improve the awareness of hypertension in Mexican Americans through media education, outpatient office visit, community educational programs and etc.
Although smoking has been shown to be a major cause of cardiovascular disease [Citation21–24], it is not clear if smoking is also a risk factor for hypertension [Citation25]. Our study showed no difference in hypertension prevalence amongst smoker and non-smoker groups. However, because NHANES define “smoker” as who has smoked more than 100 cigarettes during their lives, the smoking variable used by the NHANES to identify smokers may not be representative of the general US adult population.
Families with the lowest income had the highest prevalence but the lowest control of hypertension as compared to the group with higher income. A change is needed to address hypertension in low-income population and efforts should be made to improve treatment in this group. Efforts need to include the need for screening and education, augmented by strategies that ensure providing adequate social support, treatment and access to affordable medications [Citation26,Citation27].
Considerations should be given to the limitations of our study. First, in the NHANES, blood pressure was measured during a single visit, which may result in misclassification of some of the participants. Second, hypertension awareness, medication use, sociodemographic characteristics, health behaviors, and medical history were based on self-report and potentially subject to recall bias. Third, our study only evaluated medication use for blood pressure control. Lifestyle modifications, such as low sodium intake or physical activity, were not examined in the present analysis.
Conclusion
Based on the 2017 ACC/AHA guideline, almost half of the US adult population has hypertension. Every 3 out of 5 people are aware of their hypertension and 9 out of 10 are receiving pharmaceutical treatment. However, only 2 out of 5 people who are hypertensive have their blood pressure under controlled while on medication(s). The suboptimal number of people whose blood pressure is under control is pervasive in all subgroups of the US adult population and warrants greater efforts in prevention, as well as better screening and more effective and affordable treatment.
Disclosure statement
We report there are no potential conflicts of interest.
References
- Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383:1899–1911.
- Burt VL, Cutler JA, Higgins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26:60–69.
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252.
- Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA 2003;290:199–206.
- Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA 2010;303:2043–2050. Epub 2010/05.
- Guo F, He D, Zhang W, et al. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606.
- Yoon SS, Gu Q, Nwankwo T, et al. Trends in blood pressure among adults with hypertension: United States, 2003 to 2012. Hypertension. 2015;65:54–61.
- Ford ES. Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the United States. Circulation 2011;123:1737–1744.
- Cheng S, Claggett B, Correia AW, et al. Temporal trends in the population attributable risk for cardiovascular disease: the Atherosclerosis Risk in Communities Study. Circulation 2014;130:820–828.
- Willey JZ, Moon YP, Kahn E, et al. Population attributable risks of hypertension and diabetes for cardiovascular disease and stroke in the northern Manhattan study. J Am Heart Assoc. 2014;3:e001106.
- Saran R, Li Y, Robinson B, et al. US Renal Data System 2014 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2015;66:Svii, S1–S305.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199–2269.
- Muntner P, Carey RM, Gidding S, et al. Potential U.S. Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline. J Am Coll Cardiol. 2018;71:109–118.
- Burnier M, Oparil S, Narkiewicz K, et al. New 2017 American Heart Association and American College of Cardiology guideline for hypertension in the adults: major paradigm shifts, but will they help to fight against the hypertension disease burden? Blood Press. 2018;27:62–65.
- Islam JY, Zaman MM, Haq SA, et al. Epidemiology of hypertension among Bangladeshi adults using the 2017 ACC/AHA Hypertension Clinical Practice Guidelines and Joint National Committee 7 Guidelines. J Hum Hypertens. 2018;32:668–680.
- Khera R, Lu Y, Lu J, et al. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ. 2018;362:k2357.
- Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70:736–742.
- Paulose-Ram R, Gu Q, Kit B. Characteristics of U.S. adults with hypertension who are unaware of their hypertension, 2011-2014. NCHS Data Brief. 2017;(278):1–8.
- Ostchega Y, Hughes JP, Wright JD, et al. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens. 2008;21:159–165.
- Gooding HC, McGinty S, Richmond TK, et al. Hypertension awareness and control among young adults in the national longitudinal study of adolescent health. J Gen Intern Med. 2014;29:1098–1104.
- Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34:509–515.
- Leone A. Toxics of tobacco smoke and cardiovascular system: from functional to cellular damage. CPD. 2015;21:4370–4379.
- Tibuakuu M, Kamimura D, Kianoush S, et al. The association between cigarette smoking and inflammation: The Genetic Epidemiology Network of Arteriopathy (GENOA) study. PloS One. 2017;12:e0184914.
- Sugiura T, Dohi Y, Takase H, et al. Oxidative stress is closely associated with increased arterial stiffness, especially in aged male smokers without previous cardiovascular events: a cross-sectional study. J Atheroscler Thromb. 2017;24:1186–1198.
- Virdis A, Giannarelli C, Neves MF, et al. Cigarette smoking and hypertension. Cpd. 2010;16:2518–2525.
- Willard-Grace R, Chen EH, Hessler D, et al. Health coaching by medical assistants to improve control of diabetes, hypertension, and hyperlipidemia in low-income patients: a randomized controlled trial. Ann Fam Med. 2015;13:130–138.
- Mills KT, Rubinstein A, Irazola V, et al. Comprehensive approach for hypertension control in low-income populations: rationale and study design for the hypertension control program in Argentina. Am J Med Sci. 2014;348:139–145.
