Abstract
Background: Home blood pressure monitoring (HBPM) became a standard in the management of hypertension. However, there are few data concerning the utilisation of blood pressure (BP) monitors in daily clinical practice.
Aim: The aim of this analysis was to show: (1) how frequently hypertensive patients are equipped with BP monitors, (2) how often they perform regular HBPM and running BP diaries, (3) what are the correlates of utilisation of BP monitors, in a large real-life cohort of hypertensives examined for the efficacy of antihypertensive therapy.
Patients and methods: The survey was conducted by 570 physicians among 14,200 hypertensive patients, of whom 12,289 (6163 women; mean age 63 ± 12 years) declared use of antihypertensive medicines. Each patient was asked whether at home is having and using regularly or occasionally BP monitor and running BP diary. BP control was assessed based on the mean of two attended office BP measurements.
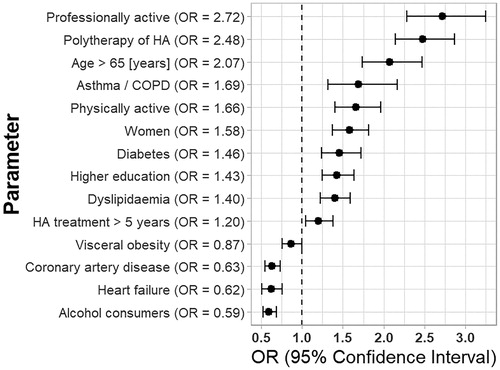
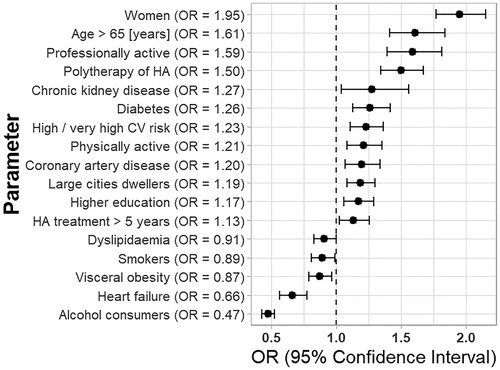
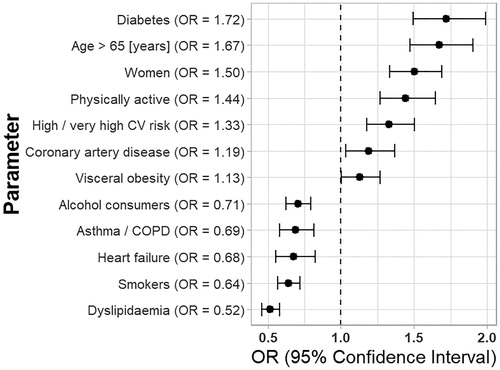
Results: Among patient equipped with BP monitors (87.2%), 73.4% were conducting HBPM regularly, while 26.6% occasionally, and 66.9% were running BP diaries. Controlled BP was achieved by 34.5% (32.9% men and 36.1% women; p < .001), more frequently by equipped with BP monitors (34.9 vs 31.7%, p < .001). Female sex, education, professional activity, active lifestyle, older age, hypertensive polytherapy, longer than 5-year therapy for hypertension, and coexistence of diabetes were factors increasing, while alcohol consumption, visceral obesity and heart failure decreasing the probability of being equipped with BP monitor and running BP diary. Regular HBPM were more frequently among women, physically active, older, diabetics, viscerally obese and patients with coronary artery disease.
Conclusions: (1) The majority of hypertensive Poles are already equipped with BP monitors, (2) three-fourth patients perform regular HBPM and two-third run BP diaries, (3) there is still a need to promote utilisation of BP monitors among younger, poorly educated hypertensive males.
Introduction
Home blood pressure monitoring (HBPM) is recommended [Citation1] as one of the methods that may improve control of hypertension by self-titration of antihypertensive medication [Citation2], and medication adherence [Citation3]. It was shown that HBPM better than conventional office blood pressure measurements (OBPM) predicts cardiovascular morbidity and mortality [Citation4]; however, the evidence that blood pressure (BP) self-monitoring may decrease cardiovascular mortality in hypertensive patients is missing.
The availability of good quality BP monitors on the market and their acceptance by patients and practising physicians increases in daily clinical practice. The lack of their reimbursement by health care systems does not seem to be any barrier in purchasing of the devices for the majority of patients, at least in developed countries. Overall, this method is better accepted by patients then ambulatory blood pressure monitoring in the management of hypertension [Citation5].
In the US, according to the HealthStyles survey performed in 2005 and 2008, the percentage of hypertensive adults regularly using HBPM increased from 40.1% to 45.8% [Citation6]. In the same period of time, a survey performed by 500 general practitioners among French patients revealed that the percentage of HBPM users increased from 70% in 2004 to 92% in 2009, but only one-fifth were using the monitors nearly systematically [Citation7].
There are limited data concerning factors affecting utilisation of BP monitors by hypertensive patients. In the United States, pharmacy customers with antihypertensive drugs prescription and lower-income or poor education level were lesser users of BP monitors [Citation8]. The list of lesser BP monitors users was extended by Ayal et al [Citation6] to youngest adults (aged 18 to 34 yrs), Non-Hispanic blacks, and those with lower income (<$40,000).
Till now, there is a lack of data concerning the utilization of BP monitors in Poland. A recent large survey (2017–2018) performed by 570 physicians, analysed the efficacy of hypertension therapy in outpatients included a question concerning the utilization of HBMP. This made feasible to analyse the association between sociodemographic characteristics and the use of BP monitors in daily clinical practice.
The aim of this analysis was to show: (1) how frequently hypertensive patients are equipped with BP monitors, (2) how often patients perform regular HBPM and running BP diaries, (3) what are the correlates of utilization of BP monitors, in a large real-life cohort of hypertensives examined for the efficacy of antihypertensive therapy.
Materials and methods
The survey was carried out from February do December 2017 by 570 family doctors, internal medicine and cardiologists or physicians during specialisation, on a group of 14,200 outpatients treated for hypertension. Doctors were recruited throughout Poland via the Internet among previous participants of other epidemiological studies organized by Europharma, the study organizer.
Only pharmacologically treated patients who agreed for the participation in the survey were included. The exclusion criterion was the inability to obtain answers to questions in the questionnaire. As the study did not meet the criterion of a medical experiment, the approval of the Bioethical Committee was not required. The survey was conducted anonymously, without proceeding patients' personal data by the study organizer.
Survey procedures
The role of participating physicians was to fill out the study questionnaire based on an interview and data from the medical history.
The questionnaire included data concerning: patients age, gender, educational level, place of residence, professional activity, smoking status, alcohol consumption, physical activity, selected anthropometric measures (body weight, height, waist circumference), two attended OBPM, period of time of treatment for hypertension, current antihypertensive medication (monotherapy/polytherapy/exact list of antihypertensive medications groups), co-morbidities, calculated cardiovascular risk (low, moderate, high, very high), having BP monitor at home, carrying out regularly or occasionally HBPM, running BP diary (recording BP values).
Data analysis
The BP control was assessed on the basis of the mean values of systolic and diastolic BP in two attended office measurements (OBPMs). The values of less than 140/90 mmHg were scored as controlled BP in accordance with the recommendations of the European Society of Hypertension and of the European Society of Cardiology (ESC) [Citation1]. A cardiovascular risk score was defined according to Polish recommendations (Polish version of Systematic Coronary Risk Evaluation – Pol-SCORE 2015) [Citation9] developed on the basis of the recommendations of ESC from 2012 [Citation10].
Utilisation of BP monitors was analysed based on self-reported data. Regular use was defined as self-performing at least one BP measurement per day.
Coronary artery disease (CAD) was defined as a history of acute myocardial infarction, percutaneous coronary intervention, coronary artery bypass graft, or the occurrence of symptoms of angina pectoris. Peripheral artery disease (PAD) and asthma/chronic obstructive pulmonary disease – COPD were assessed based on symptoms and medical records. Heart failure was diagnosed based on clinical sign and symptoms and included patients with a preserved ejection fraction of the left ventricle. Chronic kidney disease (CKD) was defined as the occurrence of estimated glomerular filtration rate below 30 ml/min/1.73m2 and/or proteinuria over 300 mg/24 hrs.
Statistical analysis
Among 14,200 patients there were 1911 subjects (976 men and 935 women) – 13.5%, without specified antihypertensive medication. This group was excluded from the analysis. Therefore, the final analysis included 12,289 subjects. Interval data were expressed as mean ± standard deviation, while qualitative data were shown as numbers with percentage. Interval data in two groups were compared with the Student’s t-test for independent data. Qualitative data were compared with χ2 test. Correlates of the utilisation of blood pressure monitors were analysed with univariable and stepwise backward multivariable logistic regression. Results were presented as odds ratio (OR) with 95% confidence interval and corresponding p-value. Factors significant in univariable analysis were included in the initial multivariable model. Statistical analysis was performed using STATISTICA 13.0 PL (Tibco Software Inc, Palo Albo, U.S.), StataSE 12.0 (StataCorp LP, TX, U.S.) and R software (R Core Team (2013). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/). Statistical significance was set at a p-value below .05. All tests were two tailed.
Results
Study group characteristics
The analysed group included 12,289 hypertensive patients (6126 men and 6163 women) receiving antihypertensive drugs (). Of those, 34.5% had controlled hypertension. There were markedly more men than women with vocational and higher education, “blue collars”, smokers, alcohol consumers, obese, with high and very high cardiovascular risk, suffering from dyslipidaemia, arteriosclerosis (both coronary and peripheral artery disease), while significantly more women than men leaving in rural areas, retired, sedentary, suffering from visceral obesity and diabetes. In addition, fewer men than women were achieving BP control (32.9 vs. 36.1%, p < .001). The controlled BP were more frequently observed in younger, better educated, large city dwellers, non-smokers, alcohol consumers, living actively, with normal weight, and low cardiovascular risk score. Each of analysed co-morbidity, except pulmonary diseases (asthma/COPD), was associated with the lesser achievement of controlled hypertension ().
Table 1. Study group characteristics’.
Table 2. Frequency of controlled hypertension and utilization of blood pressure monitors in relation to sociodemographic and clinical factors.
Utilisation of BP monitors and running BP diaries by patients
There were 87.2% patients equipped with BP monitors, of which 73.4% were regularly performing HBPM, and 66.9% were running BP diaries. More women than men were equipped with the monitors (89.7 vs 84.8%, p < .001; OR = 1.59) and were performing HBPM regularly (79.1 vs 67.4%; p < .001; OR = 1.53), as well as, running BP diaries (74.8 vs 58.5%; p < .001; OR = 1.95) – and .
Controlled BP was achieved more frequently by equipped with BP monitors (34.9 vs 31.7%, p < .001), and by patients performing HBPM occasionally than regularly (38.4 vs 33.6%, p < .001). There was no difference between patients running and not-running diaries concerning the frequency of controlled hypertension (34.7 vs 35.3%, p = .57).
Correlates of BP monitors utilization
Most frequently equipped with BP monitors were older adults (87.7%), better educated (93.8% with higher education), “white collars” (92.3%), small cities dwellers (90.5%), nondrinkers (89.6%), physically active (90%) with normal weight (90.2%). Very high (93.4%) cardiovascular risk score, CKD (92.9%), diabetes (89.7%), asthma/COPD (86.8%), and antihypertensive polytherapy (89.3%) were also more frequently equipped (). There was no association between controlled hypertension and owning BP monitor.
The univariable logistic regression odds ratios (ODs) are shown in Supplementary Table 1, while the results of stepwise backward multivariable logistic regression analysis on . Professional activity (OR = 2.72; 95% CI: 2.28–3.25, p < .001), older (OR = 2.07: 1.73–2.47, p < .001), living actively (OR = 1.66: 1.40–1.96, p < .001), women (OR = 1.58: 1.37–1.82, p < .001), better educated – secondary/higher (OR = 1.43: 1.40–1.96, p < .001) were independent socio-demographic associates of more frequent owning BP monitors. An inverse effect had only alcohol consumption (OR = 0.59: 0.52–0.68, p < .001). Co-morbidity had diverse effect. Asthma/COPD, diabetes and dyslipidaemia had positive, while visceral obesity, CAD and HF a negative effect ().
Correlates of regular HBPM performance
Among BP monitors holders, the performance of regular HBPM was related to age, gender, smoking status, alcohol consumption, physical activity, CV risk score, the period of antihypertensive therapy, and co-morbidities ( and Supplementary Table 1). It was performed most frequently by older (80%), retired (80.2%), women (79.1%), non-smokers (76.5%), non-drinkers (77.2), physically active (75.9%), with high CV risk (77.4%), treated for hypertension less than a year (87.1%) or longer than 5 years (74.3%), suffering from diabetes (79.0%) and peripheral artery disease (77.8%).
The univariable logistic regression odds ratios are shown in Supplementary Table 1, while the results of multivariable analysis on . Older age (OR = 1.67: 1.47–1.90, p < .001), women gender (OR = 1.50: 1.33–1.69, p < .001), active lifestyle (OR = 1.44: 1.27–1.65, p < .001) and high/very high CV risk (OR = 1.33: 1.17–1.50, p < .001) were independent socio-demographic associates of regular HBPM. An inverse effect had alcohol consumption (OR = 0.71: 0.62–0.79, p < .001) and smoking addiction (OR = 0.64: 0.57–0.72, p < .001).
Figure 2. Odds ratios with 95% confidence intervals of regular home blood pressure monitoring among patients equipped with blood pressure monitors. Results of stepwise backward multivariable logistic regression analysis. COPD: Chronic obstructive pulmonary disease; CV: Cardiovascular; OR: Odds ratio.
Co-morbidity had either positive (diabetes, CAD, visceral obesity) or negative (asthma/COPD, HF, dyslipidemia) correlates of regular HBPM utilisation ().
Correlates of running BP diaries
Two-third of BP monitors holders were running BP diaries, most frequently by older (72.1%), retired (72.2%), women (74.8%), large city dwellers (70.2%), non-drinkers (72.7%), with high CV risk (71.0%), treated for hypertension less than a year (82.2%), suffering from diabetes (73.2%) and coronary artery disease (72.4%).
The univariable logistic regression odds ratios are shown in Supplementary Table 1, while the results of multivariable analysis on . Women gender (OR = 1.95: 1.77–2.15, p < .001), older age (OR = 1.61: 1.41–1.84, p < .001), active lifestyle (OR = 1.21: 1.08–1.35, p < .01), dwelling in a large city (OR = 1.19: 1.08–1.30, p < .001), higher education (OR = 1.17: 1.06–1.29, p < .01), high/very high CV risk (OR = 1.23: 1.11–1.36, p < .001), hypertension treatment for longer than 5 years and polytherapy of hypertension (OR = 1.50: 1.34–1.67, p < .001) were independent socio-demographic associates of running BP diaries. Alcohol consumption (OR = 0.47: 0.43–0.52, p < .001) and smoking addiction (OR = 0.89: 0.81–0.99, p < .05) were inverse associates.
Co-morbidities were either positive (diabetes, CAD) or negative (HF, visceral obesity, dyslipidaemia) correlates of regular HBPM running BP diaries ().
Discussion
Our analysis demonstrated that 87.2% treated hypertensive patients (Caucasians) in the years 2017 – 2018 in Poland were equipped with BP monitors not reimbursed by the health care system. The frequency is somehow lower than showed in French hypertensives (92%) a decade ago [Citation7]. Despite the high utilization of BP monitors in our study only 34.5% of all subjects had controlled hypertension. The rate of controlled BP in our study was higher than shown in the most recent polish population-based studies. According to NATPOL 2011, the rates among treated were 20.5% in men and 24.7% in women, aged 18–79 years [Citation11]. In the PolSenior study (performed among older adults between 2009 and 2011), in treated individuals the percentages of controlled hypertension was were increasing with age, from 28.4 to 28.5% in aged 65–69 years to 34.1–38.4 aged >90 years [Citation12]. Therefore, we can conclude that the last decade in Poland brought improvement in the therapy of hypertension.
Of note patients equipped with BP monitors in our study, more often by 10%, achieved good control of hypertension than not equipped once (34.9 vs 31.7%). Probably, they had the opportunity to tailor their pharmacotherapy, and more safely improve BP control aim at the target.
It may seem strange that patients performing regular HBPM were less frequently obtaining controlled hypertension than those making it only occasionally (33.6 vs 38.4%), but regular HBPM is not indicated in patients with stable, controlled BP [Citation13]. Such patients should measure BP at least once a week (preferably 2 times in the morning and 2 times before bedtime) every 3 months [Citation13]. In addition, patients with resistant hypertension and “white coat effect”, less often achieving controlled hypertension but require HBPM [Citation14,Citation15]. Therefore, it cannot be concluded that regular HBPM does not improve the management of hypertension.
We also tested whether running BP diaries are associated with better BP control. However, similar percentages of controlled BP were found in patients running and not running BP diaries. It is in line with our recent study showing that only patients consulting BP reading with physicians are obtaining benefit from HBPM [Citation16], by breaking therapeutic inertia of physician, defined as unchanged medication despite elevated BP [Citation17]. In addition, it was shown that HBPM has to be combined with patient education, at least concerning the BP measurement protocol to obtain accurate results, the timing of readings, and the specific, lower BP targets for HBPM than OBPM [Citation18,Citation19]. To improve control of hypertension by self-titration of antihypertensive medication, the patient has to be informed about self-management of abnormal BP values. It seems that greater patient involvement in the treatment of unstable hypertension, like diabetics on insulin therapy, is an important way to improve BP control. This group of patients is quite challenging for physicians to prescribe a well-suited pharmacotherapy and is a place for self-management of very low and high BP values. Self-management of abnormal BP values requires patient education concerning acceptable dose reduction scale, dose delays or omission to take a dose. Patients have to acquire extensive knowledge, including after-effects of modified drugs doses, how fast they can expect their RR to get back to the normal values and what they should do with the other drugs. The training is time-consuming and demanding, suitable for cooperating patients, willing to take tips from physicians, and not suitable for patients with dementia.
The social pattern of BP monitors utilisation was analysed in few cohorts. It was already shown that individuals with lower income (not analysed in our study) [Citation6,Citation8], poor education level [Citation8,Citation20] and adults aged 18 to 34 years [Citation6] less utilise BP monitors. Our study analysed a large number of potential factors and had sufficient statistical power to extended the list of correlates of BP monitors utilisation. Our study demonstrates that younger, men, poorly educated adults, smokers, drinkers, viscerally obese, living a sedentary lifestyle, suffering from CAD, PAD, HF less frequently utilize HBPM. Having in mind lower frequency of controlled hypertension in the majority of these subgroups (men, poorly educated adults, smokers, sedentary and with CAD, PAD, HF), we can indicate that they may most benefit from education concerning HBPM. Especially important seems the education of young men, paying low attention to their health, as they may most benefit from HBPM and effective treatment of hypertension. Certainly, these patients are more challenging for physicians.
Although we did not analyse income, we showed that professional activity was the strongest correlate of owning BP monitor but not performing HBPM. This observation indirectly supports that income may have some role in making a decision to purchase a BP monitor. For the patients with the lowers income, reimbursement by National Health Service could be useful.
The pattern of factors of regular HBPM and running BP diaries was quite similar. Women, older adults, diabetics, physically active, individuals with high/very high CV risk, suffering from diabetes, and CAD, were more frequently performing regular HBPM and running the diaries. In addition patients on polytherapy, treated for HA for longer than 5 years, suffering from CKD and living in large cities were more willing to run BP diary, but not to perform regular HBPM. It seems that these factors (except the place of residence) may characterize a part of patients with greater fluctuation of BP.
Study limitations
The method of patients recruitment by physicians – consecutive patients – might cause overrepresentation of hypertensive patients with unstable hypertension, more often using medical services. Therefore the true prevalence of controlled hypertension may be superior. In addition, patients with dementia might not be enrolled due to inability to obtain answers to questions included in the questionnaire. The above-mentioned reasons, as well as the participation of cardiologists (resulting in the selection of hypertension co-existing with CAD and HF), caused that the cohort is not fully representative of the Polish population. In addition, the results cannot be generalized to Non-Caucasians, and possibly even other countries with different health care systems. The Polish Health Care System does not reimburse costs of BP monitors, but among others, guarantee free access to primary and specialistic outpatient care, and partially subsidises the purchase of antihypertensive drugs.
Conclusions
(1) The majority of hypertensive Poles are already equipped with BP monitors, (2) three-fourth patients perform regular HBPM and two-third run BP diaries, (3) there is still a need to promote utilisation of BP monitors among younger, poorly educated hypertensive males.
Supplementary_Table_1.docx
Download MS Word (14.4 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Williams B, Mancia G, Spiering W, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Press. 2018;27(6):314–340.
- McManus RJ, Mant J, Haque MS, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312(8):799–808.
- Jo SH, Kim SA, Park KH, et al. Self-blood pressure monitoring is associated with improved awareness, adherence, and attainment of target blood pressure goals: prospective observational study of 7751 patients. J Clin Hypertens. 2019;21(9):1298.
- Ward AM, Takahashi O, Stevens R, et al. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30(3):449–456.
- Nasothimiou EG, Karpettas N, Dafni MG, et al. Patients' preference for ambulatory versus home blood pressure monitoring. J Hum Hypertens. 2014;28(4):224–229.
- Ayala C, Tong X, Keenan NL. Regular use of a home blood pressure monitor by hypertensive adults – healthstyles, 2005 and 2008. J Clin Hypertens. 2012;14(3):172–177.
- Boivin JM, Tsou-Gaillet TJ, Fay R, et al. Influence of the recommendations on the implementation of home blood pressure measurement by French general practitioners: a 2004–2009 longitudinal survey. J Hypertens. 2011;29(11):2105–2115.
- Poon IO, Etti N, Lal LS. Does the use of home blood pressure monitoring vary by race, education, and income? Ethn Dis. 2010;20(1):2–6.
- Zdrojewski T, Jankowski P, Bandosz P, et al. A new version of the cardiovascular risk assessment system and risk charts calibrated for the Polish population. Kardiol Pol. 2015; 73:958–961.
- European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2012; 33:1635–1701.
- Zdrojewski T, Bandosz P, Rutkowski M, et al. Prevalence, detection and effectiveness of hypertension treatment in Poland: results of the NATPOL 2011 study. Arterial Hypertension. 2014; 18:116–117.
- Zdrojewski T, Wizner B, Więcek A, et al. Prevalence, awareness, and control of hypertension in elderly and very elderly in Poland: results of a cross-sectional representative survey. J Hypertens. 2016;34(3):532–538.
- Pickering TG, White WB, Giles TD, et al. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2010;4(2):56–61.
- Muxfeldt ES, Barros GS, Viegas BB, et al. Is home blood pressure monitoring useful in the management of patients with resistant hypertension? Am J Hypertens. 2015;28(2):190–199.
- Bonafini S, Fava C. Home blood pressure measurements: advantages and disadvantages compared to office and ambulatory monitoring. Blood Press. 2015;24(6):325–332.
- Chudek J, Owczarek AJ, Olszanecka-Glinianowicz M, et al. Consulting readings of home blood pressure monitoring with doctor increases the effectiveness of antihypertensive therapy in daily clinical practice. Cardiol Cardiovasc Med. 2019; 3:290–302.
- Agarwal R, Bills JE, Hecht TJ, et al. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57(1):29–38.
- Carter EJ, Moise N, Alcántara C, et al. Patient barriers and facilitators to ambulatory and home blood pressure monitoring: a qualitative study. Am J Hypertens. 2018;31(8):919–927.
- Kronish IM, Kent S, Moise N, et al. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. J Am Soc Hypertens. 2017;11(9):573–580.
- Wang Y, Wang Y, Gu H, et al. Use of home blood pressure monitoring among hypertensive adults in primary care: Minhang community survey. Blood Press Monit. 2014;19(3):140–144.