Abstract
Purpose: To describe current antihypertensive treatment in very old hypertensive patients according to sex and comorbidity.
Materials and methods: We used the Stockholm regional healthcare data warehouse (Vårdanalysdatabasen) providing information on all healthcare consultations, diagnoses, hospitalizations, dispensed prescription drugs, sex and age in 2.1 million people living in the greater Stockholm region, Sweden. This cross-sectional analysis identified 12,436 individuals with a diagnosis of hypertension, who were 90 years or older.
Results: Mean age was 92.6 ± 2.6 years, 75% were women; and 34% of women and 24% of men had no diagnoses of concomitant diabetes or cardiovascular disease. The number of dispensed drug classes was similar (2.1 ± 1.4) in women and in men. Women more often used angiotensin receptor blockers and beta-blockers, while men more frequently used ACE inhibitors and calcium channel blockers (all p < .05). Compared to men, women with concomitant diabetes or heart failure used less ACE inhibitors or angiotensin receptor blockers (52 vs. 60% and 49 vs. 55%, respectively; all p < .01and adjusted for age and comorbidity), which is contrary to current recommendations.
Conclusion: Our findings suggest that antihypertensive treatment is common also in very old patients. Given the rapidly ageing population and circumstantial evidence in favour of maintaining well-tolerated antihypertensive therapy in very old patients, prospective well-designed outcome studies are warranted.
Introduction
Hypertension is common, with an estimated prevalence of approximately 27% in the adult Swedish population defined as ≥140 and ≥90 mm Hg systolic and diastolic, respectively, or ongoing antihypertensive treatment [Citation1], and similar rates in other countries [Citation2,Citation3]. The prevalence increases with increasing age. It has been clearly demonstrated that blood pressure reduction by antihypertensive drug therapy substantially reduces the risk of non-fatal and fatal cardiovascular events [Citation4–6]. The benefit of antihypertensive treatment appears to be similar in women and men [Citation7,Citation8]. Emerging evidence suggests that anti-hypertensive treatment reduces cardiovascular events substantially also in the very old [Citation9,Citation10]. Of note, there is circumstantial evidence for maintaining treatment in hypertensive patients 85 years of age and beyond [Citation9,Citation10]. Thus, we need more information on the use, tolerability and efficacy of treatment of the very old to reduce the risk of cardiovascular morbidity particularly stroke and heart failure [Citation11–13].
Many countries have an ageing population. In Sweden, the current life expectancy for 2016 was 84 and 81 years in women and men, respectively, and for 2060, it is expected to be 89 and 87, respectively [Citation14]. Indeed, about half of the Swedish population born in 2017 will reach an age above 94 years in women and 92 years in men. Thus, we can anticipate a large and rapidly growing population of very old patients in need of antihypertensive treatment. Primary health care is the basis of healthcare systems in many countries including Sweden, and the majority of patients with hypertension are treated in primary health care [Citation15]. Multimorbidity goes along with an ageing population, and to improve health in patients with multimorbidity is a major challenge for primary health care [Citation16,Citation17]. However, we still lack knowledge about effective treatment strategies in very old primary healthcare patients with hypertension, and few studies have reported on treatment, drug use, and comorbidity in these patients.
Furthermore, antihypertensive drug treatment has changed during the last decades for several reasons. The introduction of newer drug classes and subsequent changes in guideline recommendations [Citation18–20], patents expiring and subsequent generic substitution at much lower cost, and decisions by authorities on which drugs are included in the national reimbursement scheme and regional formularies [Citation21] may have major impact on the choice of antihypertensive drugs prescribed.
To gain more information on current treatment of hypertension in the very old, we performed a large retrospective study using the data from the largest administrative health data register in Sweden (Vårdanalysdatabasen, VAL; the Stockholm regional healthcare data warehouse) [Citation22,Citation23] comprising more than 2.1 million inhabitants, to describe treatment in hypertensive patients 90 years of age or older, in relation to sex, and comorbidity.
Methods
Study population
There were 292,623 persons 20 years or older with a recorded primary or secondary diagnosis of hypertension (ICD-10: I10, I13, or I15) anytime between 2009 and 2013 in the greater Stockholm region, Sweden [Citation22]. For the current cross-sectional report, we identified all 12,436 patients who were residents in the region, 90 years old or above and alive and on 31 December 2013. Individuals who had moved to the Stockholm region during 2009–2013 were excluded.
The prevalence of hypertension diagnosed was calculated from census data obtained from Statistics of Sweden divided by the population, and stratified for 10 years age intervals for the same geographic region.
The drug classes recorded (with corresponding Anatomic Therapeutic Chemical classification system (ATC) codes) were angiotensin-converting enzyme inhibitors (ACE-inhibitors; C09A), angiotensin receptor blockers (ARB; C09C), beta-blockers (C07), calcium channel blockers (CCB; C08) and diuretics (C03A, C03B, C03C, C03D, C03E); amiloride was considered as a diuretic whereas mineralocorticoid receptor antagonists (MRA) were recorded separately. Other antihypertensive drugs (CO2) were mostly doxazosin and moxonidine. Fixed drug combinations (C07F, C09B, C09D) were considered as two separate drug classes.
The Regional Ethical Review Board in Stockholm approved the study.
Data sources
The population of Stockholm County represents more than one-fifth of the entire population in Sweden (9,644,864 people on 31 December 2013 at the time of the study). The Stockholm regional healthcare data warehouse provides information about all healthcare consultations including hospitalizations, diagnoses and procedures, and sex and age. It contains encrypted, anonymized data linked through each patients unique identifier (personal identification number) [Citation24] of each patient. The regional data warehouse contains all consultations in primary and secondary care (defined as specialist outpatient care) and all hospitalizations with diagnoses (according to ICD-10) and procedures. The information from hospitals corresponds to the information in the National Patient Register, managed by the National Board of Health and Welfare, which includes hospital discharges on a national level since 1964 and which is well validated [Citation25]. In addition, the regional register contains data on consultations with diagnoses recorded in primary care, since 2004. We collected information on asthma/COPD, diabetes, cardiovascular comorbidity (ICD-10): diabetes mellitus (E10-11), previous stroke/transient ischaemic attack (I60-69 or G45), ischaemic heart disease (I20-25), congestive heart failure (I50), atrial fibrillation or flutter (hereafter termed atrial fibrillation; I48) and asthma/COPD (J40-45).
Data on dispensed prescription medicines correspond to the national Prescribed Drug Register held by the National Board of Health and Welfare which contains data on all prescription drugs dispensed in Sweden since July 2005, the age and gender of the patient, prescriber category, amounts and dosages, expenditures and reimbursement [Citation26]. It has a high validity as more than 99% of all prescriptions are recorded with unique identifiers of each patient. Using the national Prescribed Registry, we collected data on dispensed prescriptions of antihypertensive drugs in 2013. In Sweden, a prescription is valid for one full year.
Statistical methods
Mean values ± SD and proportions were used to describe the study population. Differences between groups were assessed by the Student’s t-test or the Mann–Whitney U test for continuous variables, and the χ2 test for categorical variables as appropriate. Age was adjusted for by analysis of covariance. Covariates adjusted for in univariable regression analyses were age and comorbidity. A probability (p)<.05 was considered significant. The statistical analyses were performed using the STATA software, version 13.1 (College Station, TX, USA).
Results
Patient demographics
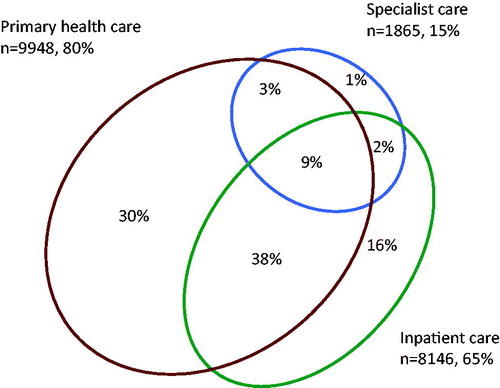
There were 12,436 patients with a recorded diagnosis of hypertension aged 90 (range 90–109) years or above; 9362 (75%) were women. The mean age of those alive in 2013 was 92.6 ± 2.6 (range 90–109) years. With an estimated 22,376 people aged 90 years or above living in the region 31 December 2013, the approximate prevalence of diagnosed hypertension in this age group was 71% in women and 65% in men. Their age distribution and prevalence according to age group are shown in . A large majority of all the patients attending health care had their diagnosis of hypertension documented in primary health care, and approximately one-third of the patients were recorded in primary health care only ().
Figure 1. Prevalence of diagnosed hypertension according to age and sex. The solid line represents the total number of women and dashed men with hypertension per age group. Dark bars represent women and light bars men.
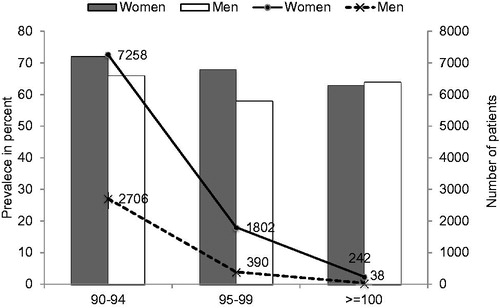
Figure 2. Proportion of patients attending different caregivers. There is an overlap between primary health care, specialist ambulatory care and inpatient care. Data for 12,436 patients with a recorded diagnosis of hypertension in Stockholm County Council anytime during the years 2009–2013, who were alive at the end of 2013.
In men, diabetes, ischaemic heart disease, and atrial fibrillation were the most common comorbidities (). Approximately, 34% of the women and 24% of the men were free of comorbidity. More than one comorbidity was present in 24% in women and 33% in men. For example, documented concomitant ischaemic heart disease and diabetes were both present in 4% of the women and 6% of the men; and, concomitant ischaemic heart disease and heart failure were both present in 12% of the women and in 16% of the men.
Table 1. Comorbidity in hypertensive patients 90 years old and above.
Drug treatment
In women, the most commonly dispensed antihypertensive drug classes were diuretics, beta-blockers, CCB, and ACE inhibitors. In men, the most common drugs were diuretics, beta-blockers, ACE inhibitors, and CCB (). The use of MRA was 6% in women and 5% in men. Very few (0.3% of women and 1% of men) received other antihypertensive drug classes (i.e. C02), mostly doxazosin (90%) and moxonidine (8%) in combination with other antihypertensive treatment. The numbers of drug classes were the same in women and in men (2.1 ± 1.4).
Table 2. The most common drug classes according to sex.
Women were more often treated with beta-blockers, ARB, and CCB, whereas men were more often treated with ACE inhibitors (). In men, the number of drugs appeared to decrease with age for all drug classes, whereas in women the changes with increasing age were small (data not shown).
Compared to patients with no cardiovascular disease or diabetes, the use of beta-blockers was more common in patients with ischaemic heart disease, atrial fibrillation and heart failure (63, 63 and 59%, respectively) (). ACE inhibitors and ARB were more common in hypertensive patients with heart failure and diabetes. Thus, ACE inhibitors or ARB were used in 49% in women and in 55% in men with concomitant heart failure (p < .01 between women and men, adjusted for age and comorbidity), and in 52% in women and 60% in men with diabetes (p < .01 between women and men, adjusted for age and comorbidity). The use of MRA and diuretics were more common in patients with concomitant heart failure and atrial fibrillation.
Table 3. Drug classes according to comorbidity.
The most common drug combinations in women were beta-blockers and diuretics, diuretics and CCB, and beta-blockers and CCB; and in men beta-blockers and diuretics, diuretics and ACE inhibitors, and beta-blockers and ACE inhibitors. The use of combination therapy with more than two drug classes was common, and 65% of the patients received 3 or more antihypertensive drugs.
Discussion
This study is more than 12,400 patients 90 years and older appears to be the first large study in very old hypertensive patients in real-life providing contemporary information on drug use and comorbidity. We show that 80% of these patients attend primary health care for the treatment of their hypertensive disease. Thus, it is most appropriate to study this age group in a primary healthcare setting.
We found that approximately one-third of the very old patients with hypertension in our study were free of cardiovascular comorbidity, diabetes, or COPD. Overall, women had less cardiac, cerebrovascular and diabetes comorbidity, while the presence of COPD was similar in women and men. These results are in general agreement with our findings in middle-aged and older hypertensive patients [Citation22]. However, in those patients, COPD was more common in women than in men, which might be attributed to smoking being more common in women. Furthermore, stopping ongoing antihypertensive treatment in the very old appears to be associated with worse prognosis [Citation11] and other results [Citation10] suggest that antihypertensive treatment may provide an improved prognosis also in the very old.
This study is the first to report on dispensed drugs in this very old age group. This gives a better reflection of medications actually being taken by the patients than only information of prescribed drugs. The use of diuretics and beta-blockers was very common. These findings could be explained by the fact that antihypertensive medication was initiated several years back at a time when these drug classes were considered first-line drugs, and changes in prescription patterns are slow if treatment is well tolerated and acceptable blood pressure control is achieved. Indeed, the use of beta-blockers and diuretics in newly initiated antihypertensive treatment is rapidly decreasing in Sweden [Citation27,Citation28]. While the use of ARB drugs was similar in women and men, ACE inhibitors were more common in men. The results indicate that concomitant cardiovascular disease and diabetes influence the choice of antihypertensive drug classes, as expected. However, compared to men, fewer women with concomitant diabetes or heart failure were taking ACE inhibitors/ARB drugs, despite these drug classes being recommended first-line drugs in both women and men for diabetes and heart failure with reduced systolic left ventricular function [Citation20].
A strength of this study is the extensive validated database used, comprising close to 12,400 patients 90 years or above with hypertension, and representing real-life data from unselected patients from care providers in primary and secondary health care [Citation22,Citation23]. We used data that automatically extracted from the records avoiding selection bias in patients or physicians, and included information on dispensed drugs, which reflects treatment better than prescribed antihypertensive drugs. Thus, there was no selection bias in patients or physicians due to any voluntary participation. There are also important limitations to consider. We only reached patients attending care with a recorded diagnosis of hypertension and people with unrecognized disease were not included. Patients and diagnoses from private caregivers and nursing homes are missing in the regional database used in our study, and could account for approximately 20% [Citation29]. However, most of these people would be included by other means because they have been hospitalized or have had consultations in public health care, and their medications are available in the Prescribed Drug Registry [Citation26]. The physicians in charge of the treatment of these patients were responsible for the diagnoses. The validity of the Swedish National Patient Registry is high [Citation25] but the accuracy of diagnoses in primary care is less well studied. When patients are admitted to hospital the accuracy of comorbidity diagnostics is considerably higher. We did not have access to blood pressure recordings in the individual patients, as this information is not available in the administrative health data register of the Stockholm region, the available information on dispensed drugs does not allow us to differentiate between patients on combinations of several drugs and those switching from one drug to another within the same time span. Frailty confers a risk for complication and for mortality, and dementia is associated with both frailty and with complications. Both combinations are common in very old and may be confounder for antihypertensive treatment [Citation30,Citation31]. Unfortunately, we do not have information available on functional status in this study population. Finally, our results were obtained 2009–2013 and the treatment of very old patients with hypertension may have changed today, given current guideline recommendations for broader treatment in the very old [Citation20].
In conclusion, this study provides unique data from more than 12,400 hypertensive patients 90 years and older, an age group not well described before. Approximately, one-third of the patients were free from cardiovascular co-morbidity and most patients were attending primary care. Given the rapidly ageing population and circumstantial evidence in favour of maintaining well-tolerated antihypertensive therapy in very old patients [Citation12], these findings warrant prospective randomized controlled outcome studies to establish optimal treatment in the very old hypertensive patient.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Kahan T, de Faire U, Hedblad B, et al. Moderately elevated blood pressure: a systematic literature review. Stockholm: The Swedish Council on Technology Assessment in Health Care; 2004–2007. p. 1–195.
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2016;389(10064):37–55.
- Wolf-Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289(18):2363–2369.
- Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957–967.
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.
- Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285–2295.
- Ljungman C, Mortensen L, Kahan T, et al. Treatment of mild to moderate hypertension by gender perspective: a systematic review. J Womens Health. 2009;18(7):1049–1062.
- Turnbull F, Woodward M, Neal B, et al. Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. Eur Heart J. 2008;29(21):2669–2680.
- Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–1898.
- Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure-lowering treatment on cardiovascular outcomes and mortality: 13 – benefits and adverse events in older and younger patients with hypertension: overview, meta-analyses and meta-regression analyses of randomized trials. J Hypertens. 2018;36(8):1622–1636.
- Beckett N, Peters R, Leonetti G, et al. Subgroup and per-protocol analyses from the hypertension in the very elderly trial. J Hypertens. 2014;32(7):1478–1487.
- Corrao G, Rea F, Monzio Compagnoni M, et al. Protective effects of antihypertensive treatment in patients aged 85 years or older. J Hypertens. 2017;35(7):1432–1441.
- Warwick J, Falaschetti E, Rockwood K, et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the Hypertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13:78.
- Swedish National Statistics. 2016. [cited 2017 May 10]. Available from: http://www.scb.se/hitta-statistik/statistik-efter-amne/levnadsforhallanden/levnadsforhallanden/undersokningarna-av-levnadsforhallanden-ulf-silc/pong/tabell-och-diagram/halsa/halsa–fler-indikatorer-19802015/
- Wandell P, Carlsson AC, Wettermark B, et al. Most common diseases diagnosed in primary care in Stockholm, Sweden, in 2011. Fam Pract. 2013;30(5):506–513.
- Lehnert T, Heider D, Leicht H, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420.
- McPhail SM. Multimorbidity in chronic disease: impact on health care resources and costs. Risk Manag Healthc Policy. 2016;9:143–156.
- National Clinical Guideline Centre. National Institute for Health and Clinical Excellence: Guidance. Hypertension: the clinical management of primary hypertension in adults: update of clinical guidelines 18 and 34. London: National Clinical Guideline Centre, Royal College of Physicians (UK); 2011.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–e248.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Pressure. 2018;27(6):314–340.
- Wettermark B, Godman B, Neovius M, et al. Initial effects of a reimbursement restriction to improve the cost-effectiveness of antihypertensive treatment. Health Policy. 2010;94(3):221–229.
- Wallentin F, Wettermark B, Kahan T. Drug treatment of hypertension in Sweden in relation to sex, age, and comorbidity. J Clin Hypertens. 2018;20(1):106–114.
- Zarrinkoub R, Wettermark B, Wandell P, et al. The epidemiology of heart failure, based on data for 2.1 million inhabitants in Sweden. Eur J Heart Fail. 2013;15(9):995–1002.
- Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, et al. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659–667.
- Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11(1):450.
- Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register – opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16(7):726–735.
- Holmquist C, Hasselstrom J, Bengtsson Bostrom K, et al. Improved treatment and control of hypertension in Swedish primary care: results from the Swedish primary care cardiovascular database. J Hypertens. 2017;35(10):2102–2108.
- Qvarnstrom M, Kahan T, Kieler H, et al. Persistence to antihypertensive drug classes: a cohort study using the Swedish Primary Care Cardiovascular Database (SPCCD). Medicine. 2016;95(40):e4908.
- Forslund T, Wettermark B, Wandell P, et al. Risk scoring and thromboprophylactic treatment of patients with atrial fibrillation with and without access to primary healthcare data: experience from the Stockholm health care system. Int J Cardiol. 2013;170(2):208–214.
- Welsh TJ, Gladman JR, Gordon AL. The treatment of hypertension in people with dementia: a systematic review of observational studies. BMC Geriatr. 2014;14(1):19.
- Gardner RC, Valcour V, Yaffe K. Dementia in the oldest old: a multi-factorial and growing public health issue. Alzheimers Res Ther. 2013;5(4):27.
