Abstract
Purpose: Credible data is scarce in representative population aged ≥18 years, though hypertension is highly prevalent and poorly controlled in population aged ≥30 years in Xinjiang Northwest China. Therefore, we tried to provide data on hypertension status for reference.
Materials and methods: We conducted a population-based cross-sectional survey between 2014 and 2015 using stratified multi-stage random sampling as part of a national survey. Hypertension is defined as systolic blood pressure (BP) ≥140 mmHg, and/or diastolic BP ≥90 mmHg and/or taking anti-hypertensive agents. We assessed prevalence, awareness, treatment and control rates of hypertension by rural and urban regions, by gender and by ethnicity, and related factors including agent prescription pattern.
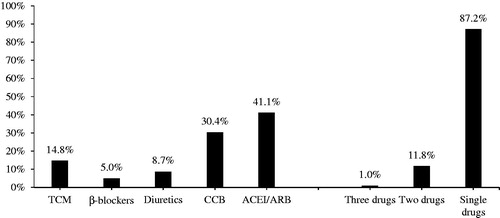
Results: Data for 6807 subjects ≥18 years with 79.2% rural and 52.0% women subjects are analyzed. Overall age-adjusted prevalence of hypertension in population aged ≥18 years is 22.2%, and shows no disparity between genders and regions. By ethnicity, the prevalence of hypertension was the highest in Tajik subjects (25.4%), followed by Mongolian (25.3%) and Kazakh (24.8%) subjects and the lowest in Kyrgyz (20.2%) subjects. Of the hypertensives, 55.5% have awareness, 43.9% receive anti-hypertensive treatment, whereas only 14.5% have their BP controlled. In different ethnic groups, the awareness, control and control in treatment rates showed no significant disparities, except for the treatment rate. It was the highest in Kazakh subjects (50.0%) and the lowest in Hui subjects (36.7%). The most common prescribed agent encompassed ACEI/ARBs (41.1%) and calcium channel blockers (30.4%). Over 87.2% of hypertensives were prescribed for single drug regimen.
Conclusions: Hypertension is moderately prevalent in Xinjiang, whereas poorly controlled. Standardization of its treatment such as introducing treatment algorithm might be the priorities for future improvement, with healthy life promotion.
Introduction
Globally 80% of cardiovascular disease (CVD) mortality occurs in low-, middle-income countries [Citation1], driven by both an increased prevalence of risk factors, such as hypertension and a relative lack of access to medical care in under-resourced health systems [Citation2]. Hypertension, 75% occurring in developing world and a major risk factor and key driver of CVD, remains widely undetected, under-treated and poorly controlled, especially in underdeveloped areas [Citation3,Citation4].
In China, prevalence of hypertension is about 27.3% in population aged ≥18 years [Citation3], up to 41.9% in population aged ≥35 years [Citation5], whereas the control rate is only 15.3%, which is even unacceptably low (8.2%) in underdeveloped areas, compared with urban population [Citation6]. Indeed, previous studies also reported patterns of hypertension may vary in remote less developed areas of China such as Xinjiang [Citation7].
Xinjiang, a less developed province, is located in Northwestern China, where historically hypertension is affecting about 35% of population aged ≥35 years [Citation8]. Also, the prevalence is as high as >50% in some population ≥30 years [Citation8,Citation9]. In addition, mortality from ischemic cerebrovascular disease, ischemic heart disease and hypertensive heart disease is higher in Xinjiang than in national average of China [Citation10]. Over 70% of stroke in China can be explained by hypertension [Citation11] and over 80% of stroke survivors in Xinjiang are reported to have hypertension [Citation12]. This evidence highlights the huge burden of the diseases attributable to hypertension in this region. However, credible data are scarce on prevalence, awareness, treatment and control rates of hypertension and on their associated factors including medication prescription pattern, specially in population aged ≥18 years. Accurate estimates of the prevalence and related factors of this condition are essential as a source of primary information and for rational planning of health services and would allow public-health policy-makers to assign sufficient priority and resources to its management and prevention [Citation13].
Between 2012 and 2015, Wang et al. conducted a nationwide survey on hypertension using a four-stage, stratified sampling method to acquire representative population aged ≥15 years and included over 7000 subjects from Xinjiang [Citation3]. In this report, we performed an analysis to this data in order to provide overall prevalence, awareness, treatment and control rates of hypertension and their associated factors in the population aged ≥18 years.
Methods
Study population
This cross-sectional study was conducted between 2014 and 2015 as a part of national study [Citation3]. A four-stage, stratified sampling method was used to select participants aged ≥15 years from general population of Xinjiang as detailed in our previous article [Citation14]. In brief, first, two cities as the urban areas and five counties as rural areas were selected using a probability proportional to size in sites selected as in . Then, two districts or two townships were selected in each city or county using simple random sampling (SRS). Next, in each district and township, three communities or villages were chosen respectively using SRS. Finally, participants stratified by sex and age were chosen using SRS according to the population composition. Finally, 7276 participants aged ≥15 years (with response rate: >95%) participated in the survey. In this analysis, prevalence, awareness, treatment and control rates were assessed in population aged ≥18 years (N = 6807).
Training and data collection
A standardized questionnaire developed by the coordinating center was administered by trained staff to obtain information on demographic characteristics and social-economic factors [Citation3]. Body mass index (BMI) was calculated as weight divided by the square of height (kg/m2). Height was measured without shoes using a standard right-angle device and a fixed measurement tape (to the nearest 0.5 cm). Bodyweight without heavy clothing was measured using an OMRON body fat and weight measurement device (V-body HBF-371, OMRON, Kyoto, Japan). BP was measured with the OMRON HBP-1300 Professional Portable Blood Pressure (BP) Monitor (OMRON, Kyoto, Japan) three times on the right arm positioned at heart level after the participant was sitting at rest for five minutes, with 30 s between each measurement with an observer present. The average of the three readings was used for analysis. For BP measurement, cuffs in various size were applied according to the circumference of the arm.
Definitions
In order to keep the data comparable to the nationwide one, we kept the definitions similar. Hypertension was defined as systolic BP (SBP) ≥140 mmHg, and/or diastolic BP (DBP) ≥90 mmHg, and/or use of antihypertensive medicine within 2 weeks, based on 2018 ESC/ESH Guideline [Citation15]. Awareness was defined as self-report of any previous diagnosis of hypertension by a doctor, treatment as self-reported use of a prescription medication for hypertension within past two weeks at the time of the interview, and control as SBP <140 mmHg and DBP <90 mmHg. In addition, the prevalence (SBP ≥130 or DBP ≥80 mmHg) of hypertension was also estimated according to 2017 ACC/AHA High Blood Pressure Guideline [Citation16].
Overweight and obesity were defined as a BMI between 24.0–27.9 and ≥28.0 kg/m2. Abdominal obesity was defined as waist circumference ≥90 cm for men and ≥85 cm for women. Current smokers were defined as participants who have smoked at least 20 packets of cigarettes in their lifetime and currently smoke cigarettes; former smokers as participants who have smoked at least 20 packets of cigarettes in their lifetime, and quit smoking for at least 1 month; never smokers as participants who never smoked or smoked <20 packets of cigarettes in their entire lifetime. Drinker was defined as consuming at least once alcoholic beverage per week in the past month.
Statistical analysis
Continuous variables were presented as means ± standard deviations (m ± SD) and were analyzed using ANOVA. Categorical variables were expressed as frequency (n) and proportion (%) and were analyzed using the Chi-square test. As for hypertension, multiple logistic analysis was used to analyze the associated factors for prevalence, awareness, treatment and control of hypertension, adjusted odds ratio (OR) with associated 95% confidence interval (95% CI) were calculated. All statistical tests were two-tailed and differences were considered statistically significant when the p value was <.05. All statistical analyses were performed using SPSS version 19.0 for Windows (SPSS Inc., Chicago, IL).
Results
Population characteristics
In total, data for 6807 subjects ≥18 years were analyzed with 79.2% rural subjects, 52.0% women subjects and 43.8% Han ethnic subjects (Supplementary Table 1). Subjects from urban area are younger than those from rural area (44.35 ± 18.54 vs. 45.70 ± 16.30, p = .007). Proportion of those who acquired senior and higher education was higher in urban area than rural area (60.5 vs. 17.3%, p < .001). Women subjects showed higher prevalence of abdominal obesity than did men subjects (46.1 vs. 33.7%, p < .001), whereas men subjects were more cigarette consumers (44.0 vs. 3.2%, p < .001) and alcohol intakers (37.1 vs. 7.2%, p < .001).
There were seven ethnic groups included in this data, whereas the number of Uygur subjects was 211, and thus we excluded them from further subgroup analysis.
Prevalence of hypertension
By 140/90 mmHg, in population aged ≥18 years in Xinjiang, age-adjusted prevalence of hypertension was 22.2% and similar for both genders (22.2 vs. 22.1%, p = .912) and for rural and urban regions (22.3 vs. 21.0%, p = .109). The prevalence of hypertension significantly decreased with increasing education attainment status from 24.0% in those with primary and lower education to 22.2% in those with junior high school education attainment and to 21.3% in those who acquired senior higher and higher education.
By modifiable factors, the prevalence of hypertension increased by obesity status. That is, it increased from 11.1% in normal subjects to 25.6% in overweight and to 40.9% in obese population by BMI. When obesity was assessed using waist circumference, the same trend was observed (). Crude prevalence of hypertension by two criteria was also assessed in subjects stratified by age, gender and region as in Supplementary Table 2. In addition, distribution of BP by characteristics is given in Supplementary Table 3.
Table 1. Prevalence of hypertension and proportions who were aware, treated and controlled by unmodifiable factors in population ≥18 years (%, 95% CI).
Prevalence of hypertension by 2017 ACC/AHA guideline
Using the 2017 American new guideline, aged-adjusted overall prevalence of hypertension was 37.6%, also similar in men (37.4%) and women (37.8%) and in rural (37.5%) and urban region (37.3%). The prevalence was the highest in obese subjects as 63% by BMI and 56.5% by waist circumference. In addition, the prevalence was the highest in current cigarette consumers (39.2%), compared past and never consumers ( and ).
Table 2. Prevalence of hypertension and proportions who were aware, treated and controlled by modifiable factors in population ≥18 years (%, 95% CI).
Prevalence of hypertension by ethnicity
By 140/90 mmHg, in different ethnic groups, the prevalence of hypertension was the highest in Tajik subjects (25.4%, 95% CI: 23.9–26.7), followed by Mongolian (25.3%, 95% CI: 24.1–26.5) and Kazakh (24.8%, 95% CI: 23.6–25.9) subjects and the lowest in Kyrgyz (20.2%, 95% CI: 19.1–21.4) subjects.
By 130/80 mmHg, the prevalence of hypertension was the highest in Kazakh (44.1%, 95% CI, 42.9–45.2), followed by Tajik (41.6%, 95% CI, 40.4–42.7) and Mongolian (38.8%, 95% CI, 37.8–39.7) and the lowest in Hui (32.1%, 95% CI, 31.2–33.0) subjects ().
Awareness, treatment and control rates of hypertension
Of the hypertensive subjects, 55.5% (95% CI 53.8–57.2) were aware of having hypertension, 43.9% (95% CI 42.1–45.6) were under anti-hypertensive treatment, whereas only 14.5% (95% CI 13.3–15.7) had their BP controlled. In addition, in hypertensives who received anti-hypertensive treatment, the control rate was 33.0%, with the higher rates in men compared to women subjects interestingly (36 vs. 30%, p < .001). In different ethnic groups, the awareness, control and control in treatment rates showed no significant disparities, except for the treatment rate. Interestingly, it was the highest in Kazakh subjects (50.0%, 95% CI: 47.5–52.4), and the lowest in Hui subjects (36.7%, 95% CI: 34.2–39.2) ( and ).
Associated factors for prevalence, awareness, treatment and control of hypertension
In non-modifiable factors, increasing age was significantly associated with existence of hypertension (OR = 1.18, 95 CI% 1.13–1.23), higher awareness (OR = 1.45, 95% CI 1.34–1.57), treatment (OR = 1.19, 95% CI 1.10–1.28) and control rates (OR = 1.14, 95% CI 1.02–1.27). In modifiable factors, overweight and obesity were significantly associated with higher prevalence of hypertension (OR = 2.10, 95% CI 1.76–2.49 and OR = 3.48, 95% CI, 2.82–4.30), compared to normal weight subjects. Current smokers showed higher risk for existence of hypertension, whereas failed to reach statistical significance (OR = 1.04, 95% CI 0.87–1.25), compared to non-smokers ().
Table 3. Multivariable-adjusted odds ratios for hypertension prevalence, awareness, treatment and control rates (OR, 95% CI).
Pattern of anti-hypertensive agent usage
A total of 680 hypertensive patients reported taking anti-hypertensive agents at the time of the survey, whereas 60% (n = 407) of the subjects provided the detailed information on prescribed agents. The characteristic comparison of hypertensive patients with and without information on anti-hypertensive agent is given in Supplementary Table 4. As in , 41.1% of hypertensives were prescribed for ACEI + ARBs, 30.4% for CCBs, 8.7% for diuretics, 5.0% for beta blockers and 14.8% were prescribed for traditional combinations. The most common used agents in each type encompassed captopril for ACEI, nifedipine for CCB, indapamide for diuretics and metoprolol for beta blockers (data not given). While further analyzing the combination therapy, it was observed that 87.2% of hypertensive patients were prescribed for single drug regimen, 11.8% for two drugs and only 1.0% were prescribed for three or more drugs ().
Figure 2. Prescription pattern of anti-hypertensive agents and percentage of single, two and three agent prescriptions in treated hypertensive patients (n = 407). Notes: (Left) Prescription pattern of anti-hypertensive agents in treated hypertensive patients. (Right) Percentage of single, two and three agent prescriptions in treated hypertension. ACEI/ARB: angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; CCB: calcium channel blockers; β-blockers: beta receptor blockers; TCM: traditional Chinese medicine.
Discussion
This is an analysis of data from Xinjiang as part of a nationwide hypertension survey in China conducted between 2012 and 2015. The main results encompassed that, the overall age-adjusted prevalence of hypertension is 22.2% in population aged ≥18 years with the highest in obese ones (40.9%). In different ethnic groups, the prevalence of hypertension is the highest in Tajik subjects (25.4%), followed by Mongolian (25.3%) and Kazakh (24.8%) subjects, and the lowest in Kyrgyz (20.2%) subjects. The overall awareness, treatment and control rates of hypertension were 55.5, 43.9 and 14.5%, respectively. Overweight and obesity and cigarette consumption were significantly associated with higher prevalence of hypertension, and lower awareness and treatment rates, compared to normal weight subjects. ACEI + ARBs (45.28%) and CCBs (33.42%) are the most commonly used agents here, whereas 87.4% of hypertensive patients were prescribed for single drug regimen.
Hypertension is a major risk factor and key driver of CVD but remains widely undetected, undertreated and poorly controlled in developing countries and especially less developed regions [Citation4]. Mortality from ischemic cerebrovascular disease and hypertensive heart disease is higher in Xinjiang than in national average [Citation10], for which hypertension is the main determinant in China [Citation17]. Although previous studies focused on status of hypertension in Xinjiang, the sampling methods and regions, population and age criteria for inclusion limited generalization of their results, making this analysis the one to report status of hypertension in relatively representative population aged ≥18 years. Jingmei Jiang et al. reported that the overall prevalence of hypertension is 50.0% in men (47.1% in urban men and 54.2% in nomad men) and 41.1% in women (22.8% in urban women and 47.0% in nomad women) in community-based Kazakh participants aged ≥30 years using stratified random clustering sampling in Altay region in 2012–2013 [Citation18]. Zhao Lei et al. reported that the prevalence of hypertension in Mongolian and Kazakh, Uygur and Han ethnic groups aged ≥30 years from Boertala Mongolian Autonomous Region was 42.0, 40.5, 35.6 and 33.2%, respectively [Citation19]. Yaoda Hu et al. reported that age and gender-adjusted prevalence of hypertension was 45.5% in Kazakh adults aged ≥30 years in Hongdun town of Altay [Citation20]. Yong Tao Wang et al. showed that overall age-adjusted hypertension prevalence was 35.01, and 36.84% in Han, 33.32% Uygur and 52.57% in Kazak population aged ≥35 years in a four-stage stratified cluster random sampling in 2007–2010 [Citation8], whereas most participants involved in the study were enrolled from big cities of Xinjiang. Mayila et al. reported the weighted prevalence of hypertension in population aged ≥45 years enrolled using four-stage, stratified, cluster sampling is 47.1% in 2011 [Citation21]. Nonetheless, the age-adjusted prevalence in this relatively representative population aged ≥18 years is 22.2%, which is parallel to 23.1% of national average in 2012–2015 [Citation3]. The age-adjusted overall prevalence goes up to 37.6%, using 130/80 criteria of ACC/AHA 2017 guideline, which includes the population with high normal BP criteria. Health providers should keep in mind that subject with BP in this range is recommended drug treatment only if high out of office BP, suggestive of masked hypertension or hypertension mediated organ damage is present.
This analysis also provides relatively updated data on hypertension status in some ethnic groups living in Northwest China. This analysis observed that hypertension prevalence is similar in Tajik (25.4%), Mongolian (25.3%) and Kazakh ethnic groups (24.8%), and lower in Kyrgyz subjects (20.2%). A survey by Yulin Wang, conducted in the rural areas of Xinjiang during 2009–2010 in 11,340 individuals ≥18 years using a stratified cluster random sampling method, reported that the age-standardized prevalence of hypertension among Kazakhs and Uyghurs are 37.0 and 26.0%, respectively [Citation22]. Mongolian and Kazakh subjects aged ≥30 years have even higher prevalence of hypertension [Citation9], whereas data in Tajik ethnic group are scarce. The latest data reported as 7.47% in representative population in 1984 [Citation23]. Current analysis also observed that prevalence of hypertension in subjects from Kyrgyz is 20.2%, similar to 20.43% in 2012 reported in another survey [Citation24]. Disparities in hypertension prevalence among ethnic groups may be attributable to different environmental exposures, ethnic-specific genetic background and their interactions. Xinjiang is a multi-ethnic and multi-cultural region. Some populations have a mixture of Asian and European ancestry [Citation25]. Population here is also characterized by higher intake of salt and animal fat and proteins [Citation26] and stock-raising regions are featured by long and cold winter, which may contribute to the prevalence of hypertension by limiting intake of essential nutrients and daily activity [Citation27]. Some populations included live in areas above 3000 m above sea level. For instance, Most Kazakh, Mongolian and Kyrgyz population live in mountainous places and Tajik subjects reside in the Pamirs with an average altitude level of 4500 m [Citation21]. Most of them lead a nomadic life and move around with seasonal changes. The higher altitude lands are characterized by alpine region and low oxygen levels and limit access to fresh vegetables and fruits, and the penetration rate of medical resources, which also play negative roles in the epidemics of hypertension. More importantly, Kazakh, Kyrgyz, Tajik and Mongolian populations are currently residing in Asian, Central Asian and Eastern European countries like Kazakhstan, Kyrgyzstan, Tajikistan, Uzbekistan, Russia, China and Turkey, who still share lifestyle and dietary habits, where burden of CVD is huge. For instance, CVD is estimated to account for more than a half (53%) of all deaths in Kazakhstan. Age-standardized CVD mortality is 636 per 100,000 in Kazakhstan and 531 per 245 100,000 in the Russia Federation in 2010, almost 5–6 times higher than the 112 per 100,000 of 246 United Kingdom [Citation28]. Nonetheless, some countries like Tajikistan still lacks epidemiological data on hypertension. Therefore, results of this study could extend to this specific population from other regions in terms of prevention of hypertension.
The awareness and treatment rates of hypertension are 55.5 and 43.9%, slightly higher than the 46.9 and 40.7% of national average [Citation3] whereas consistent with the 56.1 and 44.7% of local population ≥35 years in CARDIAC survey [Citation8] and with the 56.8 and 43.2% of local population ≥45 years in CHARLS survey [Citation29]. However, while taking into the huge burden of hypertension-related disease [Citation10], this study may have overestimated the awareness and treatment rates due to the fact that there were local hypertension intervention or survey programs conducted in Aletai [Citation20], in Akeqi [Citation11] and in Tashkurghan [Citation21], where the current survey was conducted. On the contrary, >56% of hypertensives were untreated and >85% in total hypertensives and >60% in hypertensives under treatment had uncontrolled BP in Xinjiang at the time of survey indicating that sub-optimal management is the possible reason for huge burden of hypertension-related diseases [Citation10] and that major bottlenecks for ineffective control are diagnosis, effective screening and treatment titration. Possibly, screening and quality improvement to ensure titration of medications may be critical for better outcomes [Citation30]. However, further studies are warranted to clarify the background reasons for sub-optimal management to take effective actions.
Of all the related factors, age, obesity and cigarette consumption (marginally) are observed to be in association with the existence of hypertension. Obesity is reported to possibly responsible for about 40 − 78% of hypertension in different population [Citation31,Citation32]. In this analysis, general and abdominal obesity was associated with higher prevalence of hypertension and showed dose-dependent risk for hypertension, indicating that implementation of healthy life interventions is still the core element of prevention, because even a modest weight loss has a beneficial effect on BP levels and other obesity-related diseases [Citation31,Citation32].
One important aspect of this analysis is to provide data on drug prescription, and results showed that ACEI/ARBs were prescribed for 45.28% and CCBs for, 33.42% of hypertensive patients at the time of the survey. However, 87.4% of hypertensive patients were prescribed for single drug regimen. Furthermore, the prescription percentage of 1 and ≥2 agent is slightly higher in uncontrolled hypertensives, compared to controlled ones, possibly indicating that although prescribed, the agents are not used to the best dosage to control BP. This practice pattern may suggest that there is a wide gap between evidence-based recommendations and current practice and that health providers at survey sites might have been less knowledgeable or experienced and that lack knowledge or willingness to follow new guidelines [Citation33]. In fact, clinical trials document that achieving BP targets is usually not possible with a single agent [Citation34]. Therefore, introduction of treatment algorithms as put forward in world health organization HEARTS program [Citation35] and single pill combinations should be considered the focus of future prevention.
This analysis is strengthened by relatively representative study subjects and by their diversity in ethnicity, age, sex and region, which makes the report highly informative for public health sectors and for clinical setting. However, several points deserve consideration when interpreting the data. First of all, the number of Uyghur population, one of the main ethnic minorities in Xinjiang, was too limited in this study and, therefore, caution is needed in interpreting the data as representative of the whole area. Furthermore, this analysis failed to focus on the data of salt intake, which might have brought some bias on analysis of associated factors of hypertension. Nonetheless, previous studies provided data that daily salt intake of local population is about 12.4–16.1 g and negatively associated with awareness, treatment, control and medication control rates of hypertension [Citation20]. Therefore, salt restriction, an easy, effective and affordable public health intervention, is needed urgently here.
In conclusion, hypertension is moderately prevalent in Xinjiang, whereas treatment and control rates are sub-optimal. Considering the huge burden of CVD, introduction of treatment algorithms might be the priorities for future improvement of hypertension management, together with healthy life promotion.
Online_Supplementary_tables_with_front_page.doc
Download MS Word (155 KB)Acknowledgments
Nanfang Li was involved in the study design. Mulalibieke Heizhati, Lin Wang, Nanfang Li, Jing Hong, Xiaoguang Yao, Delian Zhang, Suofeiya Abulikemu and Guijuan Chang collected the data. Mulalibieke Heizhati and Lin Wang performed the statistical analysis. Mulalibieke Heizhati and Lin Wang wrote the article. Nanfang Li, Ling Zhou, Jing Hong, Xiaoguang Yao, Delian Zhang, Suofeiya Abulikemu and Guijuan Chang gave important suggestions and did significant changes. All authors reviewed and approved the final version of the article. We also thank all the participants of the survey including the population.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization; 2011.
- Yusuf S, Rangarajan S, Teo K, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371(9):818–827.
- Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137(22):2344–2356.
- A global brief on hypertension. Geneva, Switzerland: World Health Organization; 2013.
- Li W, Gu H, Teo KK, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J Hypertens. 2016;34(1):39–46.
- Campbell NRC, Zhang XH. Hypertension in China time to transition from knowing the problem to implementing the solution. Circulation. 2018;137(22):2357–2359.
- Hozawa A, Ueshima H. Blood pressure differences by race: the importance of assessing lifestyle. Hypertens Res. 2009;32(12):1049–1050.
- Wang YT, Adi D, Yu ZX, et al. The burden and correlates of hypertension among Chinese rural population in Han, Uygur, and Kazak: a cross-sectional study. J Am Soc Hypertens. 2017;11(11):737–745.
- Yao XG, Frommlet F, Zhou L, et al. The prevalence of hypertension, obesity and dyslipidemia in individuals of over 30 years of age belonging to minorities from the pasture area of Xinjiang. BMC Public Health. 2010;10(1):91.
- Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the global burden of disease study 2013. Lancet. 2016;387(10015):251–272.
- Liu M, Wu B, Wang WZ, et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6(5):456–464.
- Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759–771.
- Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223.
- Wang L, Heizhati M, Zhang D, et al. Excess weight loss is a vital strategy for controlling hypertension among multi ethnic population in northwest China. Medicine. 2019;98(36):e16894.
- Williams B, Mancia G, Spiering W, et al. ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Pressure. 2018;27(6):314–340.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–e248.
- Yong H, Foody J, Linong J, et al. A systematic literature review of risk factors for stroke in China. Cardiol Rev. 2013;21(2):77–93.
- Jiang J, Zhang B, Zhang M, et al. Prevalence of conventional cardiovascular disease risk factors among Chinese Kazakh individuals of diverse occupational backgrounds in Xinjiang China. Int J Cardiol. 2015;179:558–560.
- Lei Z, Kun W, Yian-Ying G, et al. Epidemiology study on hypertension in boertala Mongol autonomous prefecture of Xinjiang. Chin J Hypertension. 2006;3:14.
- Hu Y, Wang Z, Wang Y, et al. Prevalence, awareness, treatment, and control of hypertension among Kazakhs with high salt intake in Xinjiang, China: a community-based cross-sectional study. Sci Rep. 2017;30(7):45547.
- Mayila K, Delian Z, Ling Z, et al. Epidemiological survey of hypertension in the middle-age and elderly people among the Tajik nationally living in Tashkurghan. Xinjiang Med J. 2018;048(004):357–359.
- Wang Y, Zhang Y, Ding Y, et al. Prevalence of hypertension among adults in remote rural areas of Xinjiang, China. Int J Environ Res Public Health. 2016;13(6):524.
- Tianyi WU, Shizhen W. A survey of blood pressure survey in some ethnic groups and plateau areas in China. Chin J Cardiovasc Dis. 1984;12:1–4.
- Weihong Z, Weihong C, Daozhen C, et al. Sampling survey of hypertension patients in Kirgiz ethnic group Akeqi County. World Health Digest. 2012;37:9–10.
- Xu S, Huang W, Qian J, et al. Analysis of genomic admixture in Uyghur and its implication in mapping strategy. Am J Hum Genet. 2008;82(4):883–894.
- Liu L, Liu L, Ding Y, et al. Ethnic and environmental differences in various markers of dietary intake and blood pressure among Chinese Han and three other minority peoples of China: results from the WHO Cardiovascular Diseases and Alimentary Comparisons (CARDIAC) study. Hypertens Res. 2001;24(3):315–322.
- Zhou L, Zhao X, Heizhati M, et al. Trends in lipids and lipoproteins among adults in northwestern Xinjiang, China, from 1998 through 2015. J Epidemiol. 2019;29(7):257–263.
- WHO Global Health Observatory Data Repository, 2016. Available from https://apps.who.int/gho/data/node.country.
- Yin M, Augustin B, Fu Z, et al. Geographic distributions in hypertension diagnosis, measurement, prevalence, awareness, treatment and control rates among middle-aged and older adults in China. Sci Rep. 2016;14(6):37020.
- Oti SO, van de Vijver S, Gomez GB, et al. Outcomes and costs of implementing a community-based intervention for hypertension in an urban slum in Kenya. Bull World Health Organ. 2016;94(7):501–509.
- Garrison RJ, Kannel WB, Stokes J, et al. Incidence and precursors of hypertension in young adults: the Framingham offspring study. Prev Med. 1987;16(2):235–251.
- Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302(4):401–411.
- Wang Z, Wang X, Chen Z, et al. Hypertension control in community health centers across China: analysis of antihypertensive drug treatment patterns. Am J Hypertens. 2014;27(2):252–259.
- Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Clin Hypertens. 2011;13(3):146–154.
- HEARTS technical package for cardiovascular disease management in primary health care: healthy-lifestyle counselling. Geneva, Switzerland: World Health Organization; 2018. WHO/NMH/NVI/18.1

