Abstract
Purpose
Cuffless blood pressure (CL-BP) measurements are believed to be a potentially alternative to cuff-occlusion-based (C-BP) measurement. A new cuffless device was developed for ambulatory BP monitoring. We assessed the accuracy of a new CL-BP device compared to a standard oscillatory C-BP device over the 24 h.
Materials and methods
Eighty-four consecutive patients were included in the study. BP was measured simultaneously by the CL-BP device and by a C-BP device over the 24 h. Calculations included 24 h mean systolic (S) BP, the mean diastolic (D) BP and the heart rate (HR). Correlations between the CL-BP and C-BP measurements were sought using Pearson’s correlation coefficients and Bland-Altman plots.
Results
Using the C-BP device, the 24 h SBP value for the cohort was 125.4 ± 10.9 mmHg (mean ± SD); the corresponding DBP value being 75 ± 8.3 mmHg. Mean SBP/DBP were higher with the CL-BP device, i.e. 131.1 ± 15.9/80.2 ± 9.7 mmHg . The correlation coefficients between the two sets of values were significant (SBP: r = 0.58, DBP: r = 0.65). Better correlations for SBP and DBP were found 1) in patients with BMI > 25 (SBP: r = 0.65, DBP: r = 0.70) compared to those with BMI <25 and 2) in males compared to females (SBP: r = 0.71, DBP: r = 0.77).
Conclusions
In our patients a CL-BP device estimated 24 h mean SBP and DBP differently from the classical oscillometric device, with a moderate correlation. CL-BP measurements were most accurate on male and overweight subjects.
Introduction
Standard devices for office, ambulatory and home blood pressure (BP) measurements make use of oscillometric or, less frequently, auscultatory methods to identify systolic and diastolic values when the pressure in a cuff applied around an arm is gradually reduced from supra-systolic levels.
However, methods based on an inflatable cuff share several limitations. For example, it is necessary to select a cuff of an appropriate size for each patient because small cuffs in overweight patients and large cuffs in underweight ones (as well as in children and adolescents) may seriously overestimate and underestimate BP, respectively [Citation1]. This may not be easy to comply with in clinical practice, for which reason cuffs of inadequate size are frequently used. Furthermore, a number of patients do not tolerate the high pressure developed within the cuff, particularly when values have to exceed a patient’s very high systolic BP. The resulting discomfort or pain (and rarely capillary ruptures) may alter patients’ customary BP values [Citation2].
Finally, cuff inflations may interfere with patients’ behaviour during the day and affect the quality of sleep during the night, thereby altering the circadian pattern. Failure to properly measure nocturnal BP is an especially serious limitation because nocturnal BP has an important prognostic value [Citation2] which makes its correct measurement important for the quantification of total cardiovascular risk [Citation3–6]
In the last few years interest has grown on the development of non-invasive cuffless BP (CL-BP) measurement devices. Based on the biological and mechanical properties of the cardiovascular system, (large artery elasticity, dimension, stiffness, etc) the developers suggest that BP can be estimated indirectly from pulse transition time or other parameters such as pulse arrival time, pulse wave velocity, pre-ejection period or their combinations. It has also been proposed that CL-BP methods that utilise electrocardiographic, photopletismometric and/or phonocardiographic sensors can be suitable for BP measurements over the 24 h with no use of the arms [Citation7–11]. This might make 24 h BP monitoring more clearly representative of patients’ behaviour over both the day and the night now limited by potential sleep disturbances and the fact that patients have to stop any activity and remain immobile when cuff inflations start.
A novel portable cuffless device has been recently developed and presented as capable to avoid the inconveniences of standard devices for ambulatory BP monitoring. In this study we evaluate its accuracy and validity.
Materials and methods
Study population
The present study conforms to the principles outlined in the Declaration of Helsinki, and was approved by the Ethical Committee of the Policlinico di Monza. Between March and September 2018, 100 consecutive outpatients were visited for hypertension at the European Society of Hypertension (ESH) Excellence Centre of Verano Brianza, Monza (Italy). For inclusion in the study, patients had to be on sinus rhythm, exibit no supraventricular or ventricular arrythmias at an EKG and sign a written informed consent. Pregnant women and patients on a pacemaker were excluded from the study
Blood pressure measurements
BP was measured simultaneously by the CL-BP Rooti RX (Rooti Labs™, Taipei City, Taiwan) and a standard cuff-occlusion based BP (C-BP) device (Spacelabs™ 90207, Verona, Italy) over the 24 h.
The CL-BP device extrapolates the pressure values from the EKG signal: first the EKG-BP pair database was built by maturing EKG and BP simultaneously. To derive the EKG to BP transfer function, features were extracted from EKG waveform both in time and frequency domain. Based on statistical learning algorithm, a quality metric was designed to iterate and optimise the model. An optional calibration mechanism provides personalised offset for each individual.
The two devices were synchronised before their application to the patient: we checked the clock time of the computer where the C-BP software was installed and we synchronised it with the one of the CL-BP device.
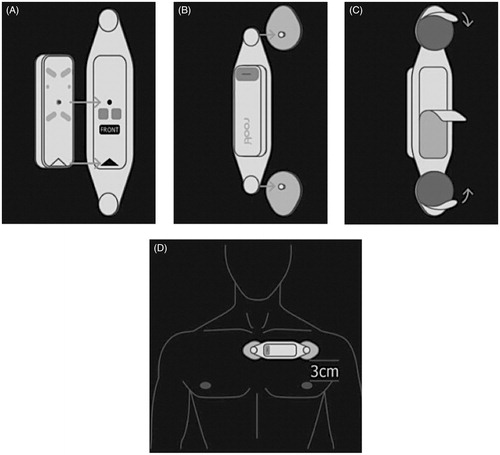
The Rooti Rx cuffless system was applied on the patient as shown in . The recording system was fixed on a disposable self-adhesive patch then connected to the skin with two electrodes. The patch/recorder system was placed on the medio-sternal area and then it was ready to be configured with the dedicated software in a few minutes. The cuffless recording system device is equipped with a software that allows calibration against three consecutive BP measurements performed with the standard device as applied to the patient’s arm. The CL-BP vs C-BP calibration procedure was performed in a quiet room with the patient seated for 5 min before beginning BP measurements. The interval between measurements was three minutes. After the calibration procedure was completed the patient was dismissed with the instruction to engage into his/her normal daily activities and to return for removal of the two the devices the next day. The CL-BP system can record BP beat by beat but to perform a correct comparison with the standard device, the CL-BP measurements data were extracted at 20 min intervals which was the same time interval programmed for measurements with the standard device.
Data analysis
For each device calculations included 24 h mean SBP, mean DBP and mean HR. From which mean absolute and percentage mean differences between the CL-BP and C-BP measuring devices were computed. Calculations were carried out for the entire cohort, and, separately, for males and females, different body mass indices and normal or elevated office BP values (< or >130/80 mmHg). Separate calculations were also made for the night (10 pm to 7am) and the day (7am to 10 pm) time. Between-device differences were graded according to the Institute of Electrical and Electronics Engineers (IEEE) and Association for the Advancement of Medical Instrumentation (AAMI) standards [Citation12,Citation13] where grade A corresponds to a BP difference of <4mmHg, grade B to a BP difference of 5–6 mmHg, grade C to a BP difference of 6–7 mmHg and grade D to a BP difference of >7mmHg.
Statistical analysis
Results are expressed as mean ± standard deviation for continuous variables and as percentage for categorical variables. The accuracy of the CL-BP device compared to the reference C-BP device was also assessed both by the correlation coefficient and by building a Bland-Altman plot. Correlation coefficient values were classified as follows: >0.75= excellent, 0.40–0.75 = fair to good, and <0.40 = poor. A p value <0.05 was considered statistically significant. Database management and statistical analysis were performed using a SPSS software (SPSS Inc., Chicago, IL, USA).
Results
Considered the study population of 100 patients 84 patients were included in the study and 16 patients were excluded for the following reasons: 10 patients stopped the BP recording too early due to cuff-related arm discomfort, 3 patients had long period of atrial fibrillation during the monitoring time and 3 patients had the BP cuff displacement with more than 50% loss of BP measurements.
Mean age was 62 years, 46.4% of the patients were women and 27.3% were diabetic. 21.4% of the patients had a high-normal BP, 39.2% patients were affected by grade 1 hypertension, 9.4% by grade 2 or 3 hypertension according to the European guidelines [Citation14], 77.3% of the patients were under hypertensive drug treatment and 25% had a history of cardiovascular events. The patients’ demographics and main clinical characteristics are reported in .
Table 1. Baseline characteristics (mean values ± standard deviation or percentages) of the study population.
Using the C-BP device, the 24 h mean SBP and DBP values of the entire cohort were 125.4 ± 10.9 mmHg and 75 ± 8.3 mmHg, respectively. The corresponding values with the CL-BP device were 131.1 ± 15.9 mmHg and 80.2 ± 9.7 mmHg), the differences being thus of a limited size and not statistically significant. Similar results were obtained in males and females as well as in patients with a lower and greater body mass index.
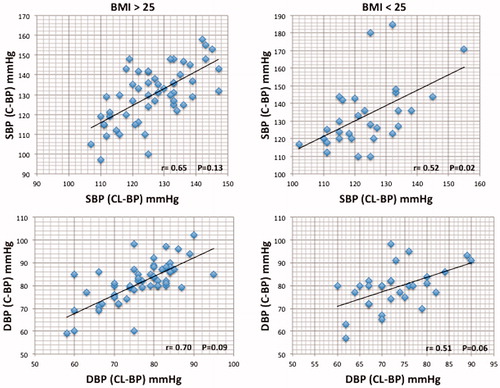
In the entire cohort the 24 h mean BP values provided by the two devices showed a significant correlation. The correlation coefficient being r = 0.58 p = 0.006 for SBP and r = 0.65, p = 0.0002 for DBP. Patients with a body mass index >25 exibited a better correlation (SBP: r = 0.65, p = 0.13; DBP: r = 0.70, p = 0.009) than those with a body mass index <25 (SBP: r = 0.52, p = 0.02 – DBP: r = 0.51, p = 0.06; ). This was also found in males (SBP: r = 0.71, p = 0.10; DBP: r = 0.77, p = 0.004) compared to female patients (SBP: r = 0.41, p = 0.03 – DBP: r = 0.45, p = 0.008).
Figure 2. Correlation between C-BP and CL-BP devices in patients with BMI > 25 and BMI < 25. C-BP: cuff based blood pressure; CL-BP: cuffless blood pressure; BMI: body mass index.
The 24 h mean absolute SBP and DBP differences between CL-BP and C-BP were 5.7 ± 13.1 mmHg and 5.3 ± 7.7 mm Hg, which correspond to IEEE and AAMI Grade B validation criteria [Citation12]. The corresponding percent differences were 3.6 ± 8.3% and 5.9 ± 9.6%. Both absolute and percent differences were lower in patients with an office BP ≥ 130/80 mmHg than in those with an office BP < 130/80 mmHg, the absolute and percent discrepancies between the two groups reaching statistical significance for DBP only (p = 0.004 and p = 0.003). SBP and DBP differences between the two devices were lower during the day than during the night, the level of significance being again achieved only for DBP (p = 0.002) ().
Table 2. Twenty-four hours mean absolute and percent differences (delta) between the blood pressure (BP) measuring devices in patients with a 24 h ambulatory SBP and DBP normal or elevated (upper panel).
The Bland-Altman analysis shows that the BP values measured with CL-BP device were on average respectively 5.7 (SBP) and 5.2 (DBP) mmHg higher than that measured with the C-BP device. When only patients with an elevated BP were considered (office BP ≥ 130/80 mmHg) the differences were less, i.e. SBP and DBP values measured with the CL-BP device were on average respectively 3.6 and 1.9 mmHg higher than those measured with the reference device (Online Supplemental File A and B).
Discussion
The present study shows that BP measurements by the cuffless device that was tested provides over the 24 h SBP and DBP average values that were higher than those simultaneously observed by a validated device of large current use. It further shows, however, that the differences were not large, and indeed that their magnitude was within the limits indicated by expert documents issued in US and Europe to represent validation [Citation12,Citation13].
The device tested seems thus to represent a suitable means to measure BP over the 24 h without the need of periodical cuff inflations. Based on our data this is likely to be the case in both genders, young and old ages, and different body mass indices. It should be emphasised that measuring 24 h BP without cuff inflations can have important advantages. First, although in a study performed years ago semiautomatic or automatic cuff inflations were found not to affect the BP values simultaneously recorded intra-arterially from the contralateral arm [Citation15] there is no question that in a number of patients these inflations may be associated with anxiety, discomfort or even pain and that this may alter BP [Citation16]. Furthermore, although in a previous study on selected patients measuring 24 h BP by a cuff-inflation-based device did not modify the nocturnal BP fall quantified intra-arterially from the contralateral arm or by tonometry [Citation17,Citation18] it is common experience that in some individuals periodical nocturnal cuff inflations can alter the quality of sleep, with a resulting alteration of night-time BP fall. It may also determine an increase of nocturnal BP variability due to the alternation between sleep-induced BP reductions and arousal-induced BP increases. Both phenomena may have adverse consequences because 1) both the night BP reduction and the absolute night-time BP value have been repeatedly reported to have a prognostic importance greater than the day-time ones [Citation3–6] and 2) an independent adverse prognostic value has been documented for BP variability as well [Citation19,Citation20]
In addition, by avoiding day-time cuff inflations, cuffless devices may also determine the day-time BP pattern in conditions closer to patients’ real life. This may occur because with cuff-based devices patients have to stop any activity and remain immobile when cuff inflations start. Activity is thus restricted and recordings not truly ambulatory. This will not happen with cuffless devices.
Several other findings of the present study need mention.
One, the differences between the tested cuffless and the standard devices were not greater in patients with higher (high normal BP and grade 2–3 hypertension) than in those with lower BP values, which suggests that our data are relevant to normotensive and hypertensive individuals.
Two, the discrepancies were not greater in patients with greater body mass indices, which is relevant to a large number of patients in whom hypertension is accompanied by an increased body mass index. A possible explanation of these differences could be the better quality of the EKG signal linked, in women, to the anatomical characteristics of the chest and in hypertensive and obese patients to the presence of a greater left ventricular mass with consequent greater amplitude of the surface EKG signal.
Three, between-device differences were about half smaller for the night than for the day-time BP values, a finding that the prognostic importance of night time BP makes once more.
Four, the reliability of the tested cuffless devices is further documented by the relatively high between-device correlation coefficients (up to 0.77) which shows that correspondence involved the majority of individual patients.
We firmly believe in the potential widespread use of CL-BP devices, particularly concerning the benefits obtained from both patient’s comfort and reduce technical limitations of standard BP evaluations. A next step for the validation of this device would be to demonstrate it to be technically non-inferior to the gold standard yet more cost-effective or efficient, and to produce consistent results in different contexts of BP measurements and in a larger cohort of patients than the one here presented; needless to say that randomisation and blinding could be very hard to obtain in this conditions.
Our study has limitations. First, we did not extend comparison to conditions in which BP may undergo marked sudden increase such as during isometric or dynamic exercise, cold pressor test, etc. although this is recommended by validation guidelines to examine the appropriateness of the measurements in conditions of sudden BP alterations. Second, some small temporal discrepancies between the two sets of BP measurements cannot be excluded because the difference between the two devices regarding their hardware clocks. However, this does not detract from the conclusion that the estimate of 24 h BP was not majorly different between the two devices.
Conclusions
In our patients a CL-BP device estimated 24 h mean SBP and DBP differently from the classical oscillometric device, with a moderate correlation. CL-BP estimates were most accurate on male and overweight subjects and the CL-BP accuracy was better in hypertensive patients and in the recording diurnal phase.
Supplemental Material
Download Zip (268 KB)Disclosure statement
The authors certify that they have no financial interest in the subject matter or materials discussed in this manuscript.
References
- Stergiou GS, Palatini P, Asmar R, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–1366.
- van der Steen MS, Lenders JW, Thien T. Side effects of ambulatory blood pressure monitoring. Blood Press Monit. 2005;10:151–155.
- Mancia G, Verdecchia P. Clinical value of ambulatory blood pressure: evidence and limits. Circ Res. 2015;116:1034–1045.
- Salles GF, Reboldi G, Fagard RH, et al.; ABC-H Investigators. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: the ambulatory blood pressure collaboration in patients with hypertension (ABC-H) meta-analysis. Hypertension. 2016;67:693–700.
- Minutolo R, Agarwal R, Borrelli S, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171:1090–1098.
- Cuspidi C, Sala C, Tadic M, et al. Nocturnal hypertension and subclinical cardiac and carotid damage: an updated review and meta-analysis of echocardiographic studies. J Clin Hypertens. 2016;18:913–920.
- McCombie DB, Shaltis PA, Reisner A, et al. Adaptive hydrostatic blood pressure calibration: development of a wearable, autonomous pulse wave velocity blood pressure monitor. Proceedings of the 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2007 Aug 22–26; Lyon, France. p. 370–373.
- Gribbin B, Steptoe A, Sleight P. Pulse wave velocity as a measure of blood pressure change. Psychophysiology. 1976;13:86–90.
- Poon C, Zhang YT. Cuffless and noninvasive measurements of arterial blood pressure by pulse transit time. Proceedings of the 27th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2005; Shanghai, China. p. 5877–5880.
- Poon C, Zhang YT, Liu YB. A study of the effects of hydrostatic pressure on pulse transit time for developing wearable cuffless blood pressure measurement devices. Proceedings of the 3rd IEEE-EMBS International Summer School and Symposium on Medical Devices and Biosensors; 2006.
- Muehlsteff J, Aubert XA, Morren G. Continuous cuffless blood pressure monitoring based on the pulse arrival time approach: the impact of posture. Proceedings 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2008 Aug 20–25; Vancouver, BC. p. 1691–1694.
- Zhongguo YL, Qi XZ, Zhi . IEEE standard for wearable cuffless blood pressure measuring devices. IEEE Standards Documents. 2015;39:285–287.
- Stergiou GS, Palatini P, Asmar R, et al. Recommendations and practical guidance for performing and reporting validation studies according to the universal standard for the validation of blood pressure measuring devices by the Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO); European Society of Hypertension Working Group on Blood Pressure Monitoring. J Hypertens. 2019;37:459–466.
- Williams B, Mancia G, Spiering W, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Press. 2018;27:314–340. Erratum in: Blood Press. 2019;28(1):74.
- Sheshadri V, Tiwari AK, Nagappa M, et al. Accuracy in blood pressure monitoring: the effect of noninvasive blood pressure cuff inflation on intra-arterial blood pressure values. Anesth Essays Res. 2017;11:169–173.
- Parati G, Pomidossi G, Casadei R, et al. Lack of alerting reactions to intermittent cuff inflations during noninvasive blood pressure monitoring. Hypertension. 1985;7:597–601.
- Villani A, Parati G, Groppelli A, et al. Noninvasive automatic blood pressure monitoring does not attenuate nighttime hypotension. Evidence from 24 h intraarterial blood pressure monitoring. Am J Hypertens. 1992;5:744–747.
- Petersen EH, Theilade S, Hansen TW, et al. Cuff inflations do not affect night-time blood pressure: comparison of 24 h ambulatory blood pressure measured by a cuff and a tonometric device in type 2 diabetes. Blood Press Monit. 2015;20:369–372.
- Mancia G, Bombelli M, Facchetti R, et al. Long-term prognostic value of blood pressure variability in the general population: results of the Pressioni Arteriose Monitorate e Loro Associazioni Study. Hypertension. 2007;49:1265–1270.
- Bilo G, Dolan E, O'Brien E, et al. The impact of systolic and diastolic blood pressure variability on mortality is age dependent: data from the Dublin Outcome Study. Eur J Prev Cardiolog. 2020; 27:355–364.