Abstract
In this report we present a case of missed hypertension due to subclavian artery stenosis. A 77 year-old female patient, initially thought as being normotensive, was referred to us due to newly discovered systolic heart murmur suspicious for aortic stenosis. We noted inter-arm blood pressure difference of 30 mmHg, with higher, hypertensive values on right arm. Further workup and medical imaging excluded aortic stenosis and revealed an asymptomatic, hemodynamically significant, stenosis of left subclavian artery. Due to absence of symptoms, the patient has been managed with conservative therapy for subclavian stenosis and hypertension, and she is currently in good conditions and followed up for any signs of disease progression. This case clearly shows importance of measuring blood pressure on both arms when initially diagnosing hypertension as this is often overlooked and is key to properly diagnose hypertension and possible subclavian stenosis.
Introduction
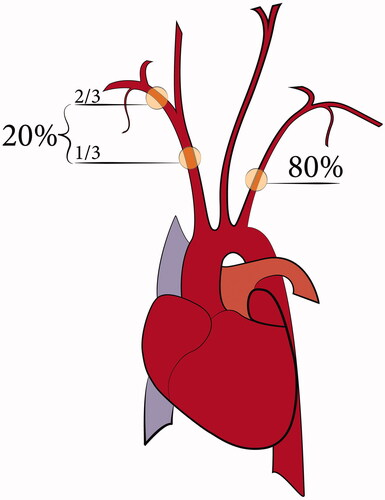
Subclavian artery stenosis is typically asymptomatic, due to its slow progression and development of collateral circulation. On the other hand, hemodynamically significant stenosis associated with more than 70% obstruction can be presented with ischaemic claudication of ipsilateral arm, distal embolisation and vertebro-basilar insufficiency due to subclavian steal syndrome [Citation1,Citation2]. It is usually caused caused by atherosclerotic plaques.Other possible causes include gigantocellular arteritis, Takayasu arteritis, post-radiation injury, trauma, thoracic outlet syndrome, fibromuscular dysplasia, neurofibromatosis, and congenital malformations [Citation1–3]. Left subclavian artery stenosis is four times more common than that the right artery (). Incidence of subclavian artery stenosis is around 2% in the general population, but it may be substantially greater in patients with usual atherosclerosis risk factors [Citation2]. In this report, we present a case of asymptomatic, hemodynamically significant, subclavian stenosis where diagnose of hypertension was missed because of described stenosis.
Case description
A 77 year-old, asymptomatic female patient, was referred to our Hypertension clinic for further work up of newly discovered systolic crescendo/decrescendo heart murmur suspicious for aortic stenosis. Until then patient had been healthy, with no regular medications. Medical history was otherwise unremarkable.
On examination, her BMI was 24 kg/m2, with excess abdominal fat and abdominal circumference of 100 cm. On auscultation, there was a noticeable systolic bruit with maximal intensity in the left supraclavicular fossa, propagating to the left side of the neck. Significant inter-arm blood pressure difference of 30 mmHg was recorded, with higher systolic pressure (163 mmHg) on her right arm and normal diastolic pressure on both arms. Electrocardiogram (ECG) showed sinus rhythm with normal heart rate and left anterior fascicular block. Laboratory results were within the reference ranges. Echocardiography revealed hypertensive heart disease, with 66% ejection fraction, without signs of aortic stenosis.
Due to significant inter-arm blood pressure difference clinical suspicion of subclavian artery stenosis was thus advanced. CTA examination () of aortocervical vasculature confirmed hemodynamically significant stenotic lesion (70 to 80%) and minimal post-stenotic dilatation of left subclavian artery after branching off aortic arch. There was also hemodynamically insignificant stenosis at the beginning of left internal carotid artery. Based on lack of symptoms we decided that there was no need for further invasive therapy. Due to apparently normal pressure on her affected arm, she had not been treated for hypertension previously. The patient was prescribed antihypertensive therapy, antilipemic therapy with statins, and antiplatelet agents. She will have regular follow-ups to evaluate efficacy of the therapy, possible other manifestations of atherosclerosis, and to early recognise possible indications for further invasive therapy. We instructed her, that blood pressure measurement should be done on her right arm.
Discussion
Identifying patients with subclavian stenosis
When collecting medical history, physicians should be attentive to certain symptoms, which include ischaemic claudication in upper extremities, or emboli to hands [Citation1]. In particularly severe cases, it can be presented as subclavian steal syndrome with syncope, vertigo, light-headedness, diplopia, dysarthria, dysphagia, ataxia, numbness, nystagmus, blurred vision, transient ischaemic attacks [Citation4]. It can even cause myocardial ischaemia in patients that had undergone coronary artery bypass graft surgery with left internal mammary arteryorintermittent ischaemic claudications in patients that underwent axillo-femoral bypass graft surgery [Citation2].
Physical examination might reveal ischaemic findings and significantly diminished or absent pulses on affected upper extremity. Care should be taken when assessing carotid pulses and radial pulses, and accurate auscultation expecting supraclavicular, cervical, vertebral and carotid bruits should be performed [Citation2].
However, all things considered the most useful and easiest means to detect sign of subclavian stenosis is inter-arm blood pressure difference of 10 mmHg or moremeasured on both arms on different occasions [Citation5].
Imaging
Further non-invasive diagnostic tools consist of colour flow Doppler ultrasound imaging. Biphasic, or dampened and monophasic waveforms, turbulent flow, and increased blood velocities, indicate a possible stenosis [Citation2].
Computed tomography angiography may provide excellent information regarding anatomical position, length and morphology of the plaque, with additional information on calcification; contrast imaging will further quantify degree of stenosis. which could be precisely identifiable also with invasive angiography [Citation2].
Management of comorbidities and hypertension
Patients with subclavian stenosis of atherosclerotic aetiology are at high risk for other cardiovascular diseases and poor long-term survival [Citation3] In this respect, Saha et al. [Citation2, p.409] pointed out that when a diagnosis of SS is made half of the patients already have coronary artery disease, and in one third of the cases stenotic lesions in carotid and vertebral vessels can also be found.
When using ambulatory blood pressure monitoring to exclude masked or white coat hypertension, measurement should be done on the arm with higher blood pressure to avoid missdiagnosing and adjust medical antihypertensive treatment [Citation6]. Importantly, in case of bilateral stenosis, pressures on both arms can be decreased and therefore misleading [Citation4].
Treatment options
Key initial decision in subclavian stenosis management is to distinguish between symptomatic and asymptomatic stenosis. In case of symptomatic stenosis, revascularization should be considered (Class IIa, level C) [Citation7]. In contrast, in asymptomatic stenosis, revascularization is advisable only in rare cases of bilateral stenosis (Class IIb, level C), in patients undergoing coronary artery bypass grafting (CABG) with ipsilateral internal mammary artery, in patients after CABG with signs of myocardial ischaemia, and in patients with ipsilateral arteriovenous fistula for dialysis (Class IIa, level C) [Citation7].
In most cases of asymptomatic stenosis medical therapy with high-dose statins, and antihypertensive medications is sufficient. Current European Society of Cardiology Guidelines recommends antiplatelet therapy only in patients with symptomatic peripheral artery disease. However, recommendations are based on The Aspirin for Asymptomatic Atherosclerosis trial [Citation8], where peripheral artery disease was suspected based on ankle-brachial index. No such trial was done for subclavian stenosis. Therefore in case of significant, asymptomatic, subclavian stenosis diagnosed with imaging and with suspected vulnerable plaque the prescription of antiplatelet drug is in our opinion at discretion of treating physician. Target LDL values are below 1.4 mmol/L, target blood pressure is less than 140/80 mmHg according to comorbidities and age group, with angiotensin converting enzyme inhibitors or angiotensin-II receptor blockers as first-line therapy. Diabetic patients need tight glycaemic control (HbA1c <7%), and smoking cessation is advised to all. Patients are encouraged to follow healthy diet and regular physical activity [Citation6,Citation7,Citation9].
Conclusion
The presented patient has asymptomatic subclavian stenosis and hypertension that should be addressed properly and was not recognised earlier because blood pressure was never measured on both arms. Our patient was managed conservatively. Statin, angiotensin converting enzyme inhibitor with blood pressure treatment target of 130/80 mmHg, and 100 mg acetylsalicylic acid as antiplatelet therapy at our discretion were prescribed. The patient has remained asymptomatic until now.
We wanted to stress the importance of inter-arm blood pressure difference measurement in patient initial visit diagnosing hypertension, as it is a simple, affordable, and useful tool and missed case of hypertension can be avoided. It can also be used as a prognostic marker of higher mortality and increased atherosclerotic burden.
Disclosure statement
No potential conflicts of interest were reported by the author(s).
References
- Salman R, Hornsby J, Wright LJ, et al. Treatment of subclavian artery stenosis: a case series. Int J Surg Case Rep. 2016;19:69–74.
- Saha T, Naqvi SY, Ayah OA, et al. Subclavian artery disease: diagnosis and therapy. Am J Med. 2017;130(4):409–416.
- Aboyans V, Criqui MH, McDermott MM, et al. The vital prognosis of subclavian stenosis. J Am Coll Cardiol. 2007;49(14):1540–1545.
- Stone PA, Srivastiva M, Campbell JE, et al. Diagnosis and treatment of subclavian artery occlusive disease. Expert Rev Cardiovasc Ther. 2010;8(9):1275–1282.
- Clark CE, Taylor RS, Shore AC, et al. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379(9819):905–914.
- Williams B, Mancia G, Spiering W, et al. Practice guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Pressure. 2018;27(6):314–340.
- Aboyans V, Ricco J-B, Bartelink M-L, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS)Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2017;39(9):763–816.
- Fowkes FG, Price JF, Stewart MC, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303(9):841–848.
- Mach F, Baigent C, Catapano AL, ESC Scientific Document Group, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2020;41(1):111–188.