Abstract
Purpose
The aim of this study was to examine myocardial performance using pressure-strain loops in hypertensive patients with different level of blood pressure control.
Material and methods
This cross-sectional study included 204 subjects (45 controls, 70 patients with well-controlled hypertension, 58 patients with uncontrolled hypertension and 31 patients with resistant hypertension) who underwent complete two-dimensional echocardiographic examination including two-dimensional speckle-tracking echocardiography. Pressure-strain curve was used to determine global myocardial work, constructive work, wasted work and work efficiency in all study participants.
Results
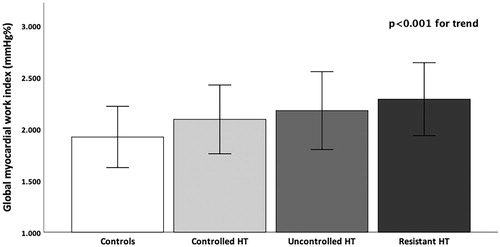
Left ventricular (LV) longitudinal strain gradually reduced from controls throughout well-controlled hypertensive patients, to patients with uncontrolled and resistant hypertension. Global myocardial work was higher in patients with uncontrolled and resistant hypertension than in controls and well-controlled hypertension. Constructive work was also higher in all hypertensive patients than in controls. Global wasted work and work efficiency were similar between different groups. Global myocardial work index was associated with peak oxygen consumption independently of sex, age, body mass index (BMI), LV structural and functional parameters in all hypertensive participants.
Conclusions
Myocardial work was significantly deteriorated in patients with uncontrolled and resistant arterial hypertension compared to controls and well-controlled hypertensive patients. Global myocardial work was associated with functional capacity independent of clinical and echocardiographic parameters.
Introduction
Left ventricular (LV) mechanics is impaired in patients with arterial hypertension [Citation1,Citation2]. This particularly refers to LV longitudinal strain. The predictive importance of LV longitudinal strain in hypertensive patients has been confirmed in several studies [Citation3,Citation4]. The effect of hypertension on layer-specific strain has also been investigated and investigations revealed its impact on all myocardial layers [Citation5,Citation6]. The influence of increased afterload on longitudinal strain reduction was previously established, which might lead to misinterpretation of the true contractile function of the myocardium, and can lead to misleading conclusions regarding decreased myocardial function [Citation3–6]. The load-dependent limitation of strain might be improved by measuring myocardial work, which considers both longitudinal strain and afterload.
Parameters of echocardiography-derived myocardial work were established recently [Citation7]. These indexes were previously determined during cardiac catheterization [Citation8]. However, this is invasive and impractical method for everyday clinical assessment. Global constructive work represents myocardial work performed during LV shortening in systole and LV lengthening during the isovolumic relaxation phase, whereas global wasted work represents myocardial work performed during LV lengthening in systole and LV shortening in isovolumic relaxation phase [Citation9].
Our recent study showed that hypertension had significant impact on myocardial work in terms of increased global myocardial work index and global constructive work [Citation10]. This was also reported from some other authors [Citation11,Citation12]. This can be explained by the fact that myocardial work takes into account not only LV longitudinal mechanics, but also arterial blood pressure and timing of valvular events, which altogether provide pressure–strain loops that can estimate LV performance in a non-invasive manner [Citation10].
Functional capacity is reduced in hypertensive patients, and previous studies showed correlation between LV longitudinal strain and functional capacity in hypertensive patients [Citation13,Citation14]. Data about the influence of different types of blood pressure control on echocardiography-derived myocardial work, and particularly relationship between myocardial work and functional capacity are unknown.
The aim of this investigation was to evaluate echocardiography-derived myocardial work in patients with well-controlled, uncontrolled and resistant arterial hypertension, as well as the association between myocardial work and functional capacity in hypertensive patients.
Methodology
This was a retrospective cross-sectional study that involved 45 control subjects, 70 controlled hypertension, 58 patients with uncontrolled hypertension and 31 patients with resistant hypertension. The patients were referred to the echocardiographic examination between March 2015 and June 2017 as the part of the screening hypertension program conducted at the University Hospital ‘Dr. Dragisa Misovic – Dedinje’, Belgrade, Serbia. Screening program included 285 patients, but 81 patients were excluded due to exclusion criteria. Inclusion criteria were arterial hypertension confirmed by 24-h ambulatory blood pressure monitoring and age ≥18 years. Exclusion criteria were: coronary artery disease, diabetes, more than mild valve disease, heart failure, atrial fibrillation, neoplastic disease, liver cirrhosis or kidney failure.
Anthropometric measures (height and weight), and laboratory analyses (fasting glucose level, total cholesterol, triglycerides and creatinine) were taken from all study participants. Body mass index (BMI) and body surface area (BSA) were calculated for each patient. Arterial hypertension was defined as clinic systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mm Hg on two separate occasions or regular taking antihypertensive treatment [Citation15]. Uncontrolled hypertension was defined as ≥140/90 mmHg in patients treated with antihypertensive therapy and resistant hypertension was defined as ≥140/90 mmHg in patients taking at least three antihypertensive drugs at optimal or best tolerated doses including a diuretic.
All patients underwent 24-h ambulatory blood pressure monitoring in order to exclude white coat hypertension and masked hypertension. Anamnestic data were used for determination of medication use and adherence to antihypertensive treatment. The study was approved by the local Ethics Committee in Belgrade (ID DM-48/2012), and written informed consent was obtained from all the participants.
Cardiopulmonary exercise testing
A maximum symptom-limited treadmill exercise test according to a modified Bruce ramp protocol (adding to the standard Bruce protocol stage 3 min; 1.7 km/h, at 5% grading) was performed in all study participants. The patients were encouraged to reach respiratory exchange ratio >1. The peak oxygen uptake (peak VO2) was evaluated by a breath-by-breath gas analysis. The ventilation/carbon dioxide slope was computed automatically. Blood pressure and heart rate were measured before and during the exercise test.
Echocardiography
Echocardiographic examination was performed using Vivid ultrasound machine (GE Healthcare, Horten, Norway). Two experienced echocardiographers performed all studies and measurements, including strain and myocardial work assessment. All parameters were averaged over three consecutive cardiac cycles. LV diameters, interventricular septum and posterior wall thickness were measured in 2D [Citation16]. The biplane method was used for evaluation of LV ejection fraction (EF). The formula of the American Society of Echocardiography was used for calculation of LV mass [Citation16], which was indexed for BSA. Left atrial (LA) volume was measured by biplane method and indexed for BSA. Transmitral Doppler inflow and tissue Doppler velocities were obtained according to the guidelines [Citation17].
LV Strain analysis and myocardial work analysis
2D strain imaging was performed by using three consecutive cardiac cycles [Citation18]. Q-analysis (EchoPAC Version 202, GE-Healthcare, Horten, Norway) was used for 2D strain evaluation. Speckle tracking analysis of the LV was performed in three apical (4- and 2-chamber and long-axis) views and parasternal short-axis view at the papillary muscle level. Longitudinal strain was assessed in apical views. The automatic tracking of the endocardial contour provided by software was manually verified and the region of interest was revised to confirm the inclusion of the whole LV thickness in all echocardiographic views. The software divided the LV into six segments in each of 4-chamber, 2-chamber, apical long-axis views and calculated longitudinal strain [Citation18].
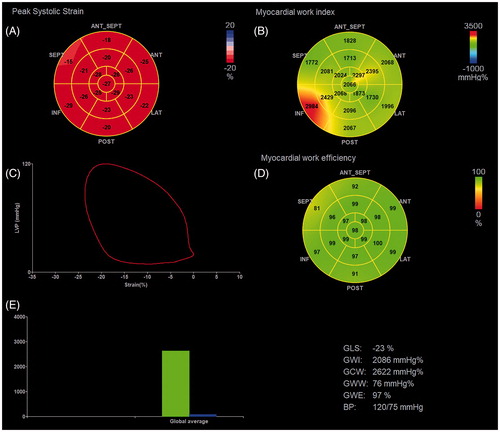
The same software was used for evaluation of myocardial work. After calculation of LV global longitudinal strain, values of brachial blood pressure were inserted and the time of valvular events was determined by echocardiography [Citation9]. Pulse-wave Doppler signal at mitral valve and aortic valve level of the apical long-axis view was used for determination of the time of valvular events. The software provided non-invasive pressure-strain loops by synchronizing longitudinal strain, blood pressure and data about the time of valvular events (). Blood pressure used for calculation of myocardial work was measured before echocardiographic examination and cardiopulmonary exercise testing was performed afterwards. Arterial pressure values were obtained by measuring the average value of two consecutive measurements (at least 5 min apart) obtained by a conventional sphygmomanometer in the sitting position. The area of the loop served as global myocardial work index, which corresponds with total work within the area of LV pressure-strain loop, from mitral valve closure to mitral valve opening (). Other parameters of myocardial work were also determined: global constructive work (myocardial work performed during LV shortening in systole and LV lengthening during the isovolumic relaxation phase); global wasted work (myocardial work performed during LV lengthening in systole and LV shortening in isovolumic relaxation phase); and global work efficiency (constructive work divided by the sum of constructive and wasted work) [Citation9]. The validation of this echocardiographic software for calculation of pressure-strain loops analysis and their correlation with invasive measurements has been previously performed [Citation19].
Figure 1. Measurement of myocardial work indices derived from left ventricular pressure and strain by echocardiography (A. Bull’s eye of left ventricular global longitudinal strain; B. Bull’s eye of myocardial work index at a blood pressure of 120/75 mmHg; C. LV pressure-strain loop; D. Bull’s eye of myocardial work efficiency; and E. Bar graph showing global constructive work and global wasted work and measured myocardial work values). BP: blood pressure; GCW: global constructive work; GLS: global longitudinal strain; GWE: global work efficiency; GWI: global work index; GWW: global wasted work.
Statistical analysis
Continuous variables were presented as mean ± standard deviation and were compared by the analysis of equal variance (ANOVA), as majority of variables showed normal distribution. Tukey HSD post-hoc analysis was used for the comparison between different groups. The Mann–Whitney U test for non-normally distributed continuous variables was used for variables that did not show normal distribution. Differences in proportions were compared by the χ2 test. The univariable and multivariable regression analyses were used to evaluate the relationship between demographic, laboratory and echocardiographic parameters and global myocardial work and constructive work. The inter- and intra-observer agreements were determined by evaluation of the intra-class correlation coefficients (ICCs) in 15 randomly chosen subjects. ICCs were used for assessment of LV strain reproducibility. The p value < .05 was considered statistically significant.
Results
Age, sex distribution and BMI were not statistically different between hypertensive groups (). ACE/ARB, beta-blockers and channel blockers were used more in patients with resistant hypertension than in other study participants. There was no difference in laboratory parameters (glucose, creatinine, total cholesterol and triglycerides levels) between different study groups ().
Table 1. Demographic characteristics and clinical parameters of study population.
Cardiopulmonary exercise test
Forced expiratory volume and forced vital capacity were similar between observed groups (). BP and heart rate at rest and during exercise were significantly higher in patients with uncontrolled and resistant hypertension than in controls and patients with well-controlled hypertension. Peak oxygen uptake was significantly lower and ventilation/carbon dioxide slope was significantly higher in patients with uncontrolled and resistant hypertension than in other two groups ().
Table 2. Cardiopulmonary exercise testing results in study population.
Echocardiographic measurements
LV diameters and EF were similar between different groups (). Interventricular septum, LV posterior wall thickness, LV mass index and LA volume index gradually increased from controls to resistant hypertensive patients (). E/A and E/é ratio gradually deteriorated from controls to resistant hypertensive patients ().
Table 3. Echocardiographic parameters of left ventricular structure and function in the study population.
2D longitudinal was significantly lower in uncontrolled and resistant hypertensive patients than in controls and patients with controlled hypertension (). Global myocardial work index gradually increased from controls, throughout controlled and uncontrolled patients, to patients with resistant hypertension (, ). The same was found for global constructive work. However, statistical significance was revealed only when different hypertensive patients were compared with controls. Global wasted work and global work efficiency were similar between observed groups ().
Regression analyses
Univariable regression analysis showed significant association between sex, SBP, E/é, LV mass index, LVEF and global myocardial work index (). SBP, E/é and global myocardial work index were independently associated with peak oxygen capacity in hypertensive patients ().
Table 4. Univariable and multivariable regression analysis of different demographic and echocardiographic parameters and parameters of peak oxygen uptake in hypertensive patients.
Reproducibility
Intra-observer variability
The intra-observer variability was high for LV longitudinal strain: ICC (95% CI) = 0.93 (0.92–0.94), p < .001; global myocardial work index 0.94 (0.92–0.96); global constructive work 0.95 (0.93–0.97); global wasted work 0.92 (0.90–0.94) and global work efficiency 0.96 (0.95–0.97).
Inter-observer variability
Interclass correlations coefficients were also high for LV longitudinal strain: ICC (95% CI) = 0.91 (0.88–0.95), p < .001; global myocardial work index 0.92 (0.89–0.93); global constructive work 0.93 (0.91–0.95); global wasted work 0.91 (0.88–0.97) and global work efficiency 0.95 (0.94–0.96).
Discussion
This study revealed several important findings that deserve further discussion. First, global myocardial work index was higher in resistant hypertension than in controls and controlled-hypertension. Second, all hypertensive patients had higher global constructive work than controls. Third, functional capacity was significantly decreased in uncontrolled and resistant hypertension compared to controls and well-controlled hypertension. Fourth, global myocardial work index was associated with peak oxygen uptake in hypertensive patients independently of clinical and echocardiographic parameters.
Myocardial work includes blood pressure into equation and provides incremental information to LVEF and LV longitudinal strain that are sensitive to LV afterload. Russell et al. reported that increased afterload induce reduction of longitudinal strain, which is not associated with decreased contractility as one might think, but with change in afterload [Citation7]. Furthermore, the pressure–strain loop area reflects myocardial metabolic demand (myocardial glucose metabolism measured by positron emission tomography – PET) and oxygen consumption [Citation7], which showed that the myocardial work method provided insight into myocardial energetics. Our study showed reduced longitudinal strain and increased global myocardial work index and constructive work in patients with hypertension and particularly in those with uncontrolled and resistant hypertension in comparison to normotensive controls. This could be explained by lower longitudinal strain and higher blood pressure in these patients. Interestingly, longitudinal strain decreased gradually from controls to resistant hypertension, whereas myocardial work did not significantly differ between various groups of hypertensive patients (controlled, uncontrolled and resistant). The reason for this finding could be higher blood pressure in patients with uncontrolled and resistant hypertension. Additionally, increased myocardial work index and constructive work in these patients might represent initial compensatory changes in development of hypertensive heart disease. Our findings revealed no difference in global wasted work and work efficiency. Considering that wasted work reflects myocardial work that does not contribute to LVEF and lengthening of myocytes during systole, it seems that LV stretching is not impaired in hypertensive patients, which would be expected due to increased myocardial interstitial fibrosis and stiffness that are well-known features for hypertensive heart disease [Citation2].
Functional capacity was significantly lower in uncontrolled and resistant hypertension than in controls and well-controlled hypertension and there was a significant association between longitudinal strain and peak oxygen consumption. Similar findings were previously reported from our group [Citation20]. The novelty of this study is the relationship between functional capacity and global myocardial work index in hypertensive patients. Previous study showed correlation between myocardial work and myocardial glucose metabolism assessed by PET [Citation7]. Study that investigated patients with heart failure with preserved ejection fraction (HFpEF) showed that global constructive work, but not global myocardial work index, was independently of global lo with peak oxygen consumption [Citation21]. Approximately, 90% of study population had arterial hypertension, but prevalence of other risk factors, such as obesity and diabetes was also significant. Nevertheless, our patients do not have HFpEF, but they are under large risk of HFpEF development and therefore results are similar. Future studies will show if myocardial work parameters might be used for prediction of HFpEF development in hypertensive patients and particularly in those with resistant hypertension.
Echocardiographic evaluation of myocardial work has several important advantages over invasive measurements obtained during heart catheterization. This is non-invasive, potentially widely available and rapid method that is not associated with any complication for patient. Myocardial work seems to be more sensitive marker of myocardial impairment than longitudinal strain and therefore could be used in evaluation of myocardial involvement in hypertensive and diabetic patients, as well as in those with heart failure and cardiomyopathies, which represents the most important clinical implication of myocardial work variables [Citation22].
Limitations
This study has some limitations that should be discussed. The patients with other comorbidities were excluded from this study, which limits the generalization of our results. The adherence to antihypertensive treatment was not evaluated by drug concentration in serum, but from anamnestic data, which represents an important limitation of our study. Echocardiographic evaluation of LV mechanics and myocardial work might be influenced by the inadequate quality of ultrasound images. However, this kind of limitation cannot be overcome in clinical investigations and do not induce any relevant bias. Subclinical coronary artery disease was not excluded. However, echocardiographic examination and cardiopulmonary exercise test accompanied with ECG monitoring excluded relevant coronary artery disease. In this study, systolic BP measured at a clinical visit rather than supine BP measured at the time of the echocardiography was used for calculation of myocardial work. The cross-sectional nature of this investigation does not allow estimation of causal relationship between hypertension and LV myocardial work.
Conclusion
This study revealed that LV myocardial work and mechanics were significantly worse in uncontrolled and resistant hypertensive patients than in controls and well-controlled hypertensive patients. Study revealed that myocardial work was independently of age, sex, BMI and LV function and hypertrophy associated with peak oxygen consumption in patients with hypertension. Further follow-up investigations with large population of hypertensive patients are necessary to assess prognostic impact of myocardial work on cardiovascular outcome in hypertensive patients.
Author contributions
MT and VC contributed to the study design, collecting data, analysis and writing the article, CC contributed to study design, interpretation of data and writing the article, BP and VV contributed to the data collection and methodology, ST and GG contributed to the interpretation of data and revised it with important intellectual contribution.
Disclosure statement
The authors declare no conflict of interest related to this study.
References
- Lembo M, Santoro C, Sorrentino R, et al. Prominent basal and middle strain longitudinal involvement in newly-diagnosed and never treated hypertensive patients without clear-cut hypertrophy. Int J Cardiol. 2020;304:179–184.
- Tadic M, Cuspidi C, Bombelli M, et al. Hypertensive heart disease beyond left ventricular hypertrophy: are we ready for echocardiographic strain evaluation in everyday clinical practice? J Hypertens. 2018;36(4):744–753.
- Al Saikhan L, Park C, Hardy R, et al. Prognostic implications of left ventricular strain by speckle-tracking echocardiography in the general population: a meta-analysis. Vasc Health Risk Manag. 2019;15:229–251.
- Saito M, Khan F, Stoklosa T, et al. Prognostic implications of LV strain risk score in asymptomatic patients with hypertensive heart disease. JACC Cardiovasc Imaging. 2016;9(8):911–921.
- Tadic M, Cuspidi C, Vukomanovic V, et al. Layer-specific deformation of the left ventricle in uncomplicated patients with type 2 diabetes and arterial hypertension. Arch Cardiovasc Dis. 2018;111(1):17–24.
- Kim SA, Park SM, Kim MN, et al. Assessment of left ventricular function by layer-specific strain and its relationship to structural remodelling in patients with hypertension. Can J Cardiol. 2016;32(2):211–216.
- Russell K, Eriksen M, Aaberge L, et al. A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J. 2012;33(6):724–733.
- Hulshof HG, van Dijk AP, Hopman MTE, et al. Acute impact of changes to hemodynamic load on the left ventricular strain-volume relationship in young and older men. Am J Physiol Regul Integr Comp Physiol. 2020;318(4):R743–R750.
- Manganaro R, Marchetta S, Dulgheru R, et al. Echocardiographic reference ranges for normal non-invasive myocardial work indices: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2019;20(5):582–590.
- Tadic M, Cuspidi C, Pencic B, et al. Myocardial work in hypertensive patients with and without diabetes: An echocardiographic study. J Clin Hypertens (Greenwich). 2020;22:2121–2127.
- Chan J, Edwards NFA, Khandheria BK, et al. A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2019;20(1):31–39.
- Mansour MJ, AlJaroudi W, Mansour L, et al. Value of myocardial work for assessment of myocardial adaptation to increased afterload in patients with high blood pressure at peak exercise. Int J Cardiovasc Imaging. 2020;36(9):1647–1656. 10.1007/s10554-020-01867-9.
- Tadic M, Cuspidi C, Suzic-Lazic J, et al. Influence of circadian blood pressure patterns and cardiopulmonary functional capacity in hypertensive patients. J Clin Hypertens (Greenwich)). 2019;21(10):1551–1557.
- Tadic M, Ivanovic B. Why is functional capacity decreased in hypertensive patients? From mechanisms to clinical studies. J Cardiovasc Med (Hagerstown). 2014;15(6):447–455.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041.
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2015;28(1):1–39.
- Quinones MA, Otto CM, Stoddard M, et al. Recommendations for quantification of Doppler echocardiography: a report from the Doppler quantification task force of the nomenclature and standards committee of the American Society of Echocardiography. J Am Soc Echocardiogr. 2002;15(2):167–184.
- Mor-Avi V, Lang RM, Badano LP, et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. Eur J Echocardiogr. 2011;12(3):167–205.
- Hubert A, Le Rolle V, Leclercq C, et al. Estimation of myocardial work from pressure-strain loops analysis: an experimental evaluation. Eur Heart J Cardiovasc Imaging. 2018;19(12):1372–1379.
- Celic V, Tadic M, Suzic-Lazic J, et al. Two- and three-dimensional speckle tracking analysis of the relation between myocardial deformation and functional capacity in patients with systemic hypertension. Am J Cardiol. 2014;113(5):832–839.
- Przewlocka-Kosmala M, Marwick TH, Mysiak A, et al. Usefulness of myocardial work measurement in the assessment of left ventricular systolic reserve response to spironolactone in heart failure with preserved ejection fraction. Eur Heart J Cardiovasc Imaging. 2019;20(10):1138–1146.
- Chan J, Edwards NFA, Scalia GM, et al. Myocardial work: a new type of strain imaging? J Am Soc Echocardiogr. 2020;33(10):1209–1211.