Abstract
Purpose
There has been limited evidence for the association between socioeconomic status (SES) and arterial stiffness. This study was performed to investigate the association between household income and brachial pulse pressure (PP) in the general Korean population.
Materials and methods
This study was based on data acquired in the 2018 Korea National Health and Nutrition Examination Survey (2018 KNHANES). A total of 13004 subjects at the age of 20 years or older analysed. The information on monthly household income was obtained through the questionnaire, and was stratified into 5 groups for each quintile. Brachial blood pressure (BP) was measured 3 times, and the average of the second and third measured BPs were used. PP was calculated as the difference between systolic and diastolic BPs.
Results
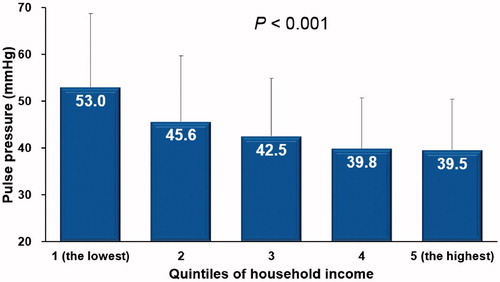
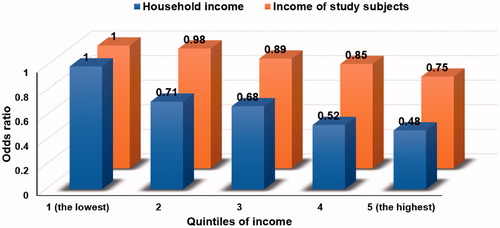
A lower household income was associated with a higher prevalence of cardiovascular risk factors. As household income increased, PP decreased proportionally (p < .001). In multiple linear regression analysis, household income (per quintile) was independently associated with PP even after controlling for potential confounders (β = −.125, p < .001). Multiple binary logistic regression analysis showed that the increased household income level was significantly associated lower probability having higher PP (≥ 43.5 mmHg) even after controlling for multiple covariates (the lowest vs. the highest household income; odds ratio, 0.48; 95% confidence interval, .41–.55; p < .001).
Conclusion
Low household income was associated with higher PP. This provides additional evidence for the association between low SES and high arterial stiffness.
Introduction
Pulse pressure (PP) is defined as the difference between systolic and diastolic blood pressures (BPs). PP is an indicator of arterial stiffness. In the healthy and complaint arteries, PP is low because systolic BP is not too high and diastolic BP is not too low by the buffering action of elastic arteries. However, as blood vessels lose their elasticity and become stiff with age, systolic BP rises, diastolic BP decreases, and PP increases [Citation1,Citation2]. Recognition of PP is clinically important, because it has been suggested that PP is an independent risk factor for the incidence and mortality of cardiovascular disease (CVD) [Citation3–8].
Many studies have reported the association between low socioeconomic status (SES) and increased risk of mortality and CVD [Citation9–12]. However, underlying pathophysiological mechanisms linking the high burden of CVD in patients with low SES has not been completely elucidated. It is fundamental and important to identify the correct mechanisms for better prevention and treatment.
Recently, our group have shown that arterial stiffness measured by brachial-ankle pulse wave velocity was significantly higher in subjects with medical aid beneficiaries than those with national health insurance beneficiaries. Additionally, medical aid beneficiaries were independently associated with higher brachial-ankle pulse wave velocity in multivariable analysis, suggesting the close interaction between low SES and arterial stiffening [Citation13]. As an extension of that study, we tried to determine whether PP, another marker of arterial stiffness, is related to SES in this study. The Korea National Health and Nutrition Examination Survey (KNHANES) data contains a variety of information about SES, such as household income, education level and occupational status [Citation14,Citation15]. We hypothesized that low SES would increase arterial stiffness, which is associated with poor cardiovascular outcome. Therefore, this study was performed to investigate the association of household income and PP using KNHANES database.
Materials and methods
Study population
This study used data acquired from the KNHANES database [Citation14,Citation15]. KNHANES has been conducted by the Ministry of Health and Welfare of Korea every year since 2007 to determine the health and nutritional status of the Korean people. KNHANES is a nationally representative, stratified, complex, and multistage sample survey. The data were obtained publicly through the proper raw data request procedure of the Korea Disease Control and Prevention Agency (KDCA) [Citation16]. The KNHANES was approved by the Institutional Review Board (IRB) of KDCA (IRB number, 2018-01-03-P-A). In this study, analysis was conducted on subjects at 20 years of age or older included in the 2018 KNHANES data. A total of 16489 subjects were identified in the 2018 KNHANES data; 1881 subjects under the age of 20, 38 subjects without household income data, and 26 subjects without PP data were sequentially excluded. Finally, 13004 subjects were analyzed in this study. The IRB of Boramae Medical Center (Seoul, Korea) approved this study protocol (IRB number, 07-2021-1) and waived written informed consent.
Household income
The information on monthly household income was obtained through the questionnaire, and stratified into 5 groups for each quintile. The specific amount of income according to sex and age is shown in .
Table 1. Clinical characteristics of study subjects according to household income.
PP
BP was measured by the 4 trained nurses in charge of BP measurement in the KDCA’s professional investigation team. In order to reinforce quality control for BP measurement, the BP measurement certification system was used, and the BP measurement method was standardized according to the current guidelines [Citation17]. BP was measured manually by the auscultatory method using a mercury sphygmomanometer of the right upper arm at the heart level. Systolic BP was taken to be the pressure at the first Korotkoff sound (when the sound is first heard) and diastolic BP was the pressure at which the fifth Korotkoff sound (the time when the sound disappears and could not be heard). BP was measured 3 times at intervals, and the average value of the second and third measured BP were used. PP was calculated as the difference between systolic and diastolic BPs.
Covariates
Body mass index was calculated as body weight in kilogram divided by height in square meter (kg/m2). Obesity was defined as body mass index ≥25 kg/m2. Information on cardiovascular risk factors, which included hypertension, diabetes, dyslipidemia and previous history of stroke as well as angina and myocardial infarction diagnosed by a physician. Information was also collected on whether or not the study subjects currently smoke or, if so, how much. We collected information on the frequency of alcohol drinking and aerobic exercise. Doing aerobic exercise was defined as performing medium-intensity physical activity for 2 h and 30 min or more, or 1 h and 15 min for high-intensity physical activity, or a mixture of medium-intensity and high-intensity physical activity (1 min for high intensity is 2 min for medium intensity) per week. Educational attainment was classified as elementary school or less, middle school, high school and college or more. Job status (with or without) and residence area (urban or rural) was also assessed. When residing in Seoul, Gyeonggi-do, and 5 metropolitan cities in Korea, it was defined as urban residence. Venous blood samples were obtained after overnight fasting more than 8 h, and the blood levels of the following laboratory parameters were measured: white blood cell count, hemoglobin, uric acid, creatinine, glucose, glycated hemoglobin, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglyceride and C-reactive protein. Information on how many subjects were taking anti-hypertensive, anti-diabetic and anti-dyslipidemic medications were reviewed.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed as percentages. In comparisons among 5 groups per quintile, analysis of variance was used for continuous variables, and chi-square test was used for categorical variables. Multiple linear correlation and multivariable logistic regression analyses were used to show independent association between household income and PP. Age, sex, body mass index, hypertension, diabetes mellitus, dyslipidemia, smoking, alcohol, aerobic exercise, creatinine, glycated hemoglobin, uric acid, total cholesterol and C-reactive protein were considered potential confounders and controlled during multivariable analyses. Receiver operating characteristic (ROC) curve analysis was used to obtain the cut-off value of PP predicting previous history of stroke, angina and myocardial infarction. The cut-off value of PP obtained from ROC curve analysis was used as a dependent variable in multiple logistic regression analysis. A p value of <.05 was considered statistically significant. All statistical analyses were performed using SPSS 22.0 (IBM Corp., Armonk, NY, USA).
Results
The clinical characteristics of the study subjects according to household income are shown in . Lower household income was associated with older age, more female dominance, greater body mass index and higher BP. Cardiovascular risk factors were more frequently observed in subjects with lower household income than with higher household income. Laboratory results also showed more unfavorable profiles for subjects with lower household income than with higher household income. Educational level was lower and less subjects had job in subjects with lower household income than those with higher household income. More subjects with lower household income took anti-hypertensive, anti-diabetic and anti-dyslipidemic medications compared to those with higher household income. As household income increased, PP decreased proportionally (p < .001) (). In multiple linear regression analysis, household income (per quintile) was independently associated with PP even after controlling for potential confounders (model 1, with adjustment for age, sex and body mass index, β = −.130, p < .001; model 2, with adjustment for cardiovascular risk factors including hypertension, diabetes mellitus, dyslipidemia, previous history of coronary artery disease, smoking, alcohol and aerobic exercise in addition to potential confounders in model 1, β = −.126, p < .001; model 3, with adjustment for laboratory findings including creatinine, glycated hemoglobin, uric acid, total cholesterol and C-reactive protein in addition to potential confounders in model 2, β = −.123, p < .001) (). The association between household income and PP was stronger in male than in female subjects (). In ROC curve analysis, the cut-off value of PP predicting previous history of stroke, angina and myocardial infarction was 43.5 mmHg (area under curve, 0.71; 95% confidence interval, 0.69–0.73; sensitivity, 63.7%; specificity, 68.8%; p < .001) (). In multiple binary logistic regression analysis using this cut-off value of PP as a dependent variable, increased household income level was significantly associated lower probability having higher PP (≥43.5 mmHg) even after controlling for multiple covariates (the lowest vs. the highest household income; odds ratio, 0.49; 95% confidence interval, 0.41 ∼ 0.58; p < .001) (). In the same multivariable analysis, there was an independent association between the subjects’ income level and PP (), but it was weaker than that between the household income level and PP (). The higher the level of education attainment, the lower the PP (), which was maintained even after controlling for various confounding variables in multivariable analysis (). Subjects with job had significantly lower PP than those without (), and the absence of job was an independent factor determining higher PP (≥43.5 mmHg) ().
Figure 2. Receiver operating characteristic curve analysis showing the cut-off value of pulse pressure predicting previous history of stroke, angina and myocardial infarction.
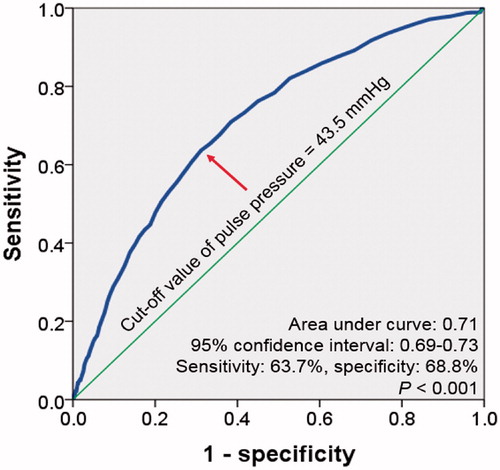
Table 2. Multiple linear regression analyses showing the independent association between household income and pulse pressure.
Table 3. Multiple binary logistic regression analyses showing the independent association between household income and high pulse pressure (≥43.5 mmHg).
Table 4. Multiple binary logistic regression analyses showing the independent association between income of study subjects and high pulse pressure (≥ 43.5 mmHg).
Discussion
Our study showed a negative correlation between the household income level and PP in the general Korean population. The association between household income and PP was significant in both multivariable linear and logistic regression analyses after adjustment for many clinical factors. Although there was also a significant association between the subjects’ income level and PP, it was weaker than that between household income and PP. Additionally, low educational level and unemployment were also independently associated with higher PP. To the best of our knowledge, this is the first report showing the associations of household income, educational level and job status with PP. This finding provides additional evidence for the association between low SES and increased arterial stiffness.
Association between SES and arterial stiffness
Only a few studies have shown the association between lower SES and increased arterial stiffness. A study of 2566 people showed that childhood family SES was independently associated with adult arterial stiffness as measured by carotid distensibility and PWV [Citation18]. Recently, our group investigated 8929 subjects and also showed that brachial-ankle PWV was significantly higher in patients with medical aid beneficiaries than with National Health Insurance beneficiaries [Citation13]. In a study of Japanese civil servants, education level was significantly associated with brachial-ankle PWV values after adjusting for existing risk factors, C-reactive protein, and occupational stress [Citation19]. In a longitudinal study, baseline aortic PWV progressed faster during the 5-year follow-up in subjects with lower employment grade, household income, and education [Citation20]. It has been reported that African Americans with lower SES adolescents had a greater PWV compared to Caucasians with higher SES adolescents [Citation21]. In consistent with these findings, the results of present study using a large number of study subjects also demonstrated that lower household income was associated with higher PP even after adjustment for potential covariates. Because PP is also an important indicator of arterial stiffness (1,2), our study, in addition to other studies mentioned above, has provided additional evidence for an association between SES and arterial stiffness.
Suggested mechanisms
Although the exact mechanism for low household income and high PP is not known, some possible hypotheses can be suggested. The first thing to consider is that low SES and high PP share risk factors such as old age, hypertension, diabetes mellitus and dyslipidemia [Citation1,Citation2,Citation13,Citation22]. In addition, antihypertensive medications were less frequently prescribed, and adherence to medications is lower in subjects with low SES, which eventually increase BP and PP [Citation23]. Also, it has been suggested that increased inflammatory response in subjects with low SES may contribute to an increase in arterial stiffness [Citation24,Citation25]. In consistent with these findings, our study showed increased white blood cell counts and higher level of C-reactive protein in subjects with lower SES than with higher SES. Increased sympathetic tone by exposure to more stress in subjects with low SES [Citation26] could be another possible underlying pathophysiology explaining the increased PP in subjects with low SES [Citation27]. Although information on birth weight was not available in our study, it could be another clue to mediate the association. Because it has been suggested that low SES is associated with low birth weight [Citation28,Citation29], which is an important risk factor for early vascular aging, arterial stiffening and increased PP [Citation30].
Household income vs subjects’ income
The association was stronger between household income and PP than between subjects’ income and PP in our study. It can be interpreted that family SES, rather than the individual subjects’ SES, has a greater influence on the arterial stiffness and further cardiovascular risk. The reason for this is unknown, but can be explained by the fact that Koreans cherishes family-oriented community.
Clinical implications
Although it is well-known that subjects with low SES have an increased cardiovascular risk, the mechanism is not clear. In order to improve the prognosis of subjects with low SES, it is necessary to first understand the underlying pathophysiological mechanism and then seek effective treatment strategies based on them. Our study suggested that increased arterial stiffness can play a role as a mediator for low SES and high cardiovascular risk. Since PP data can be obtained simply by just measuring arm BP, PP may be particularly useful for risk stratification in subjects with low SES. Further studies are needed on whether SES improvement could lead to PP decrease. In addition, the social support system should be centered on the household rather than the individual subjects in that the PP increase was more influenced by households’ income than the individual subjects’ income demonstrated in this study.
Study limitations
There are several limitations in this study. First, the cross-sectional study design was unable to determine the causal relationship between household income and PP. However, it seems more natural to think that households’ income influenced subjects’ PP when judging the background knowledge so far rather than vice versa. Second, the cut-off value of PP used as a dependent variable in logistic regression analysis may not predict the occurrence of future cardiovascular events, but it was calculated based on the cardiovascular events experienced by the subjects in the past. Third, cardiovascular drugs may affect PP value, but our study did not provide this information. Lastly, since the results of our study were obtained from the general Korean population, direct application of our results to other groups may be difficult.
Conclusions
Our study of a relatively large number of subjects showed that low household income was associated with higher PP, which provides additional evidence for the association between low SES and high arterial stiffness.
Supplementary_BP_Revised_clean_20210507.docx
Download MS Word (253.6 KB)Disclosure statement
The authors declare that there is no conflict of interest associated with this manuscript.
References
- Dart AM, Kingwell BA. Pulse pressure – a review of mechanisms and clinical relevance. J Am Coll Cardiol. 2001;37(4):975–984.
- Avolio AP, Van Bortel LM, Boutouyrie P, et al. Role of pulse pressure amplification in arterial hypertension: experts' opinion and review of the data. Hypertension. 2009;54(2):375–383.
- Benetos A, Safar M, Rudnichi A, et al. Pulse pressure: a predictor of long-term cardiovascular mortality in a French male population. Hypertension. 1997;30(6):1410–1415.
- Benetos A, Rudnichi A, Safar M, et al. Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension. 1998;32(3):560–564.
- Thomas F, Blacher J, Benetos A, et al. Cardiovascular risk as defined in the 2003 European blood pressure classification: the assessment of an additional predictive value of pulse pressure on mortality. J Hypertens. 2008;26(6):1072–1077.
- Glynn RJ, Chae CU, Guralnik JM, et al. Pulse pressure and mortality in older people. Arch Intern Med. 2000;160(18):2765–2772.
- Fang J, Madhavan S, Alderman MH. Pulse pressure: a predictor of cardiovascular mortality among young normotensive subjects. Blood Press. 2000;9(5):260–266.
- Zhao L, Song Y, Dong P, et al. Brachial pulse pressure and cardiovascular or all-cause mortality in the general population: a meta-analysis of prospective observational studies. J Clin Hypertens (Greenwich). 2014;16(9):678–685.
- Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation. 2018;137(20):2166–2178.
- Stringhini S, Carmeli C, Jokela M, LIFEPATH consortium, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet. 2017;389(10075):1229–1237.
- Clark AM, DesMeules M, Luo W, et al. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712–722.
- Kucharska-Newton AM, Harald K, Rosamond WD, et al. Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population-based data from the United States and Finland. Ann Epidemiol. 2011;21(8):572–579.
- Kim HL, Lee JY, Lim WH, et al. Relationship of socioeconomic status to arterial stiffness: comparison between medical aid beneficiaries and National Health Insurance Beneficiaries. Am J Hypertens. 2020;33(8):718–725.
- Hong KH, Lee Y. Negative correlation between vitamin A and positive correlation between vitamin E and inflammation among healthy adults in Korea: based on the Korea National Health and Nutrition Examination Survey (KNHANES) 2016-2018 7th Edition. J Inflamm Res. 2020;13:799–811.
- Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014;43(1):69–77.
- Cho MJ, Kim YS, Park EY, et al. Association between periodontal health and stroke: results from the 2013-2015 Korea National Health and Nutrition Examination Survey (KNHANES). J Dent Sci. 2021;16(1):268–274.
- Lee HY, Shin J, Kim GH, et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019;25:20.
- Puolakka E, Pahkala K, Laitinen TT, et al. Childhood socioeconomic status and arterial stiffness in adulthood: the Cardiovascular Risk in Young Finns Study. Hypertension. 2017;70(4):729–735.
- Saijo Y, Yoshioka E, Fukui T, et al. Relationship of socioeconomic status to C-reactive protein and arterial stiffness in urban Japanese civil servants. Soc Sci Med. 2008;67(6):971–981.
- Trudel X, Shipley MJ, McEniery CM, et al. Socioeconomic status, education, and aortic stiffness progression over 5 years: the Whitehall II prospective cohort study. J Hypertens. 2016;34(10):2038–2044.
- Thurston RC, Matthews KA. Racial and socioeconomic disparities in arterial stiffness and intima media thickness among adolescents. Soc Sci Med. 2009;68(5):807–813.
- Laurent S, Cockcroft J, Van Bortel L, European Network for Non-invasive Investigation of Large Arteries, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27(21):2588–2605..
- Leng B, Jin Y, Li G, et al. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33(2):221–229.
- Gruenewald TL, Cohen S, Matthews KA, et al. Association of socioeconomic status with inflammation markers in black and white men and women in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Soc Sci Med. 2009;69(3):451–459.
- Park S, Lakatta EG. Role of inflammation in the pathogenesis of arterial stiffness. Yonsei Med J. 2012;53(2):258–261.
- Algren MH, Ekholm O, Nielsen L, et al. Associations between perceived stress, socioeconomic status, and health-risk behaviour in deprived neighbourhoods in Denmark: a cross-sectional study. BMC Public Health. 2018;18(1):250.
- Świerblewska E, Hering D, Kara T, et al. An independent relationship between muscle sympathetic nerve activity and pulse wave velocity in normal humans. J Hypertens. 2010;28(5):979–984.
- Son M, An SJ, Choe SA, et al. Role of parental social class in preterm births and low birth weight in association with child mortality: a national retrospective cohort study in Korea. Yonsei Med J. 2020;61:805–815.
- Park MJ, Son M, Kim YJ, et al. Social inequality in birth outcomes in Korea, 1995-2008. J Korean Med Sci. 2013;28:25–35.
- Nilsson PM, Lurbe E, Laurent S. The early life origins of vascular ageing and cardiovascular risk: the EVA syndrome. J Hypertens. 2008;26:1049–1057.