Abstract
Purpose
Little is known on the beliefs, perceptions and practices of hypertension specialists in addressing non-adherence to therapy. Therefore, a survey was undertaken amongst healthcare professionals (HCPs) managing hypertension in the European Society of Hypertension (ESH) Centres of Excellence.
Materials and methods
Cross-sectional data were obtained between December 2020 and April 2021 using an online anonymous structured questionnaire including 26 questions/136 items, that was sent to all ESH Excellence centres.
Results
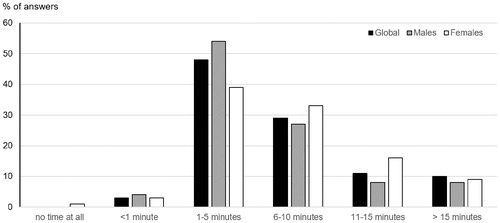
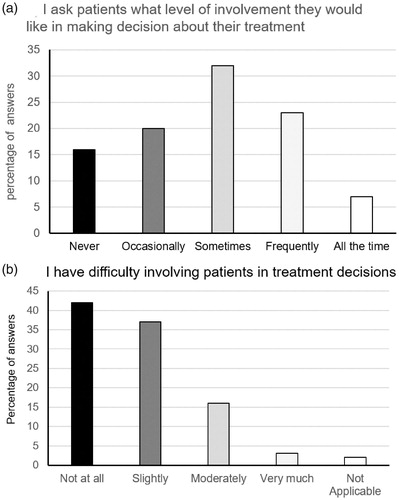
Overall 67 from 187 centres (37.3%) responded and 200 HCPs from 30 countries answered the questionnaire. Participants (60% men) were mainly physicians (91%) and nurses (8%) from University hospitals (77%). Among physicians, 83% had >10 years professional experience. Average time dedicated to discuss medications was 1-5 min in 48% and 6-10 min in 29% of cases. Interviews with patients about adherence were the most frequently used assessment method. Chemical detection of medications in urine was available in 36% of centres. One third of physicians involved their patients regularly in treatment decisions. The most frequent methods to improve adherence included simplification of medication therapy, more frequent visits, and home blood pressure monitoring.
Conclusions
The level of implementation of tools to detect and improve adherence in hypertension management by HCPs in ESH excellence centres is low. Structured educational activities focussing on adherence management and access to the newest objective measures to detect non-adherence might improve these deficits.
Introduction
The European Society of Cardiology and the European Society of Hypertension 2018 recommendations on the management of hypertension in adults state that three important factors contribute to the poor control of blood pressure (BP) in hypertension [Citation1]. These factors are low patients’ adherence to non-pharmacological as well as to pharmacological treatments, therapeutic/physician inertia and deficiencies of healthcare systems in their approach to chronic diseases [Citation1]. A partial or complete non-adherence to prescribed medications is very common in chronic ‘silent’ diseases, such as hypertension and dyslipidemia or diabetes [Citation2]. In chronic diseases such as hypertension, the causes and implications of non-adherence are multidimensional and complex [Citation3]. Thus, poor adherence not only limits a physician’s ability to achieve optimal BP control but also significantly impairs the capacity to reduce the patients’ cardiovascular risk [Citation4] and the occurrence of severe clinical outcomes such as stroke, heart failure, coronary artery disease or chronic kidney diseases [Citation3,Citation5–7].
Since the last few decades, great efforts have been dedicated to the detection of patients who are poorly adherent to their antihypertensive medications [Citation3,Citation8,Citation9]. This was important because recognition of partial or complete non-adherence is very difficult [Citation10] and represents the crucial first step of any intervention on medication adherence [Citation8]. Several qualitative studies have examined patients’ perspectives regarding their beliefs and attitudes towards the need of taking medications to treat their hypertension [Citation11]. One large European survey investigated how healthcare professionals (HCPs) such as physicians, nurses and pharmacists supported patients with taking medicines and evaluated their perceptions about the effectiveness of those actions [Citation12]. However, little is known about the beliefs, perceptions and practices of hypertension specialists in addressing non-adherence to therapy. Therefore, this study aimed to understand, through a survey, the beliefs and behaviour of healthcare professionals in managing non-adherence in hypertension amongst European Centres of Excellence of the European Society of Hypertension (ESH).
Methods
This survey focussed on the perception of initiation, adherence and persistence to antihypertensive medications of HCPs. In addition, the survey evaluated HCPs’ beliefs and behaviours regarding adherence including the choice of approaches to assess medication adherence and interventions to improve adherence to medication therapy. A previously published questionnaire was slightly adapted (Supplementary Appendix 1) and used with the permission of the authors [Citation13]. This questionnaire has been developed and previously used in the European Ascertaining Barriers for Compliance (ABC) project (http://www.ABCproject.eu) and is based on a combination of published but unvalidated scales measuring aspects of HCPs behaviours and recommendations for clinical practice from published adherence guidelines [Citation14]. The questionnaire was modified for the present study to include questions on new techniques such as the chemical detection of antihypertensive medications. It contains 26 questions and 136 items. The first seven questions on the characteristics of the participants were mandatory in order for the questionnaire to be validated.
This cross-sectional multinational online observational survey was addressed to all the designated leads or contact persons of the Centres of Excellence of the European Society of Hypertension (n = 187) using the SoGo Survey platform. (www.sogosurvey.com). Thereafter, all the leads were requested to distribute the survey internally to the members of their Excellence Centre, for example, to other HCPs involved in hypertension management in their centre. All participants could complete the survey only once. In case of non-response, one reminder e-mail was sent. The study was conducted between 1 December 2020 and 1 April 2021. Approval was waived by the ethics committee considering the fact that answering the questionnaire was free and represented implicit consent.
Statistics
Descriptive analyses of the data were undertaken to show the distribution of the percentage of answers in each answer category for every item. Missing data were excluded from the analysis. Data were analysed according to sex and years of professional experience.
Results
Overall 67 of the 187 centres responded resulting in a response rate of 37.3%. A total of 205 HCPs participated in the survey from the 67 centres. From these, 5 responses had to be excluded because mandatory questions were not completed, thus providing an average of 3.1 responses per centre. Results from 200 questionnaires from 30 countries were available for further analyses. As shown in , the majority of participants were males (60%). The respondents were mainly physicians (91%) and from University hospitals (77%), while 8% were nurses, only a few were biologists working in laboratories and no pharmacist participated. Participating HPCs were largely treating adult (99%) patients with hypertension. The large majority of participants (83%) had a professional experience of more than 10 years.
Table 1. Demographic characteristics of the participants.
shows the participants’ perception on initiation of therapy, adherence and persistence of patients treated for hypertension in their countries and their centres. When evaluating the entire population of their country, 42% of participants estimated that 0–15% of patients did not initiate their antihypertensive therapy and 44% of participants suggested that this number ranges between 16 and 35%. Regarding their perception of adherence and persistence, half of the participants believed that 36–65% of patients were adherent to therapy and persistent on therapy at 1 year. One-quarter of the answers suggested that adherence and persistence range between 66 and 85%. Interestingly, when assessing their own patients, participants were more positive with 66% of participants considering that less than 15% of their patients do not initiate therapy and 59% of participants estimating that adherence and one-year persistence ranges between 65 and 100%.
Table 2. Healthcare professionals’ perception on initiation of therapy, adherence and persistence of patients treated for hypertension in their country and in their own centre.
shows the time spent talking with patients about their use of medications according to sex. The majority of participants indicate that they spent between 1 and 5 min and about one-third of them spent 6–10 min discussing medication therapy with their patients. Females tend to spend a bit more time talking with patients but one must take into account that 20% of participating females were nurses, who dedicated more time with patients in their interviews. Indeed 6.5% of physicians answered that they spend more than 15 min discussing the use of medication whereas this percentage was 31.5% for nurses. When considering physicians only, we found no difference between men and women.
shows that more than 90% of participants agreed or strongly agreed that patients’ beliefs and concerns about antihypertensive medications have an impact on adherence and persistence. More than 95% of HCPs also agree/strongly agree that adherence can be improved, but the majority (82.8%) agreed that one single intervention cannot resolve all adherence issues. The participants’ opinion on whether non-adherence is intentional or not appears to be more divided. Further, 80.1% of HCPs agreed with the fact that patients have the right to refuse or to stop their medications provided they are correctly informed on the risks. Interestingly, more than 60% of participants consider that non-adherence is difficult to recognise (answers to the question: moderately and very much).
Table 3. Participants’ beliefs on adherence to medications in hypertension.
The survey included several questions on the methods used to assess adherence in patients with hypertension. It is evident from , that asking patients specific questions on the way they handle their medications is the most common approach. Also, interactions with the family, friends or other HCPs to assess non-adherence are common. Interestingly, most objective approaches such as using questionnaires, electronic monitors, dedicated Apps, pill count tools, and chemical detection of medications in urine or blood and directly observed therapy are either not used or used only occasionally. Pharmacy data appear to be used frequently by about 20% of participants and from time to time by 35% of them.
Table 4. Methods used to assess adherence in patients with hypertension.
Methods and approaches used by participants to improve medication adherence are shown in . HCPs appear to work essentially on simplifying treatment schemes, associating medication intake with routine activities, using medication dispensers, providing written information, recommending home BP monitoring and increasing the frequency of medical consultations. The involvement of family members and nurses is common but collaboration with pharmacists is limited.
Table 5. Methods and interventions used to improve medication adherence in hypertensive patients.
Among the barriers encountered by the participants to address adherence issues correctly and to implement adherence enhancing interventions, the most frequently mentioned are: the identification of non-adherent patients, the short duration of consultations, the high workload, the lack of continuity of antihypertensive care to support adherence, inadequate resources available in the healthcare system (Supplemental Table 1). The lack of financial incentives appears to be only a moderate barrier.
shows the participants’ behaviour in terms of sharing treatment decisions with patients. Data show that a substantial percentage of HCPs do not ask their patients if they want to be involved in therapeutic decisions and admit having some difficulties involving their patients in treatment decisions. In accordance with these difficulties, 56% of participants had never had any training on the management of adherence during their medical or nursing education and an adherence management program was lacking in close to 60% of centres.
Analyses of the survey according to the number of years of professional experience (> or <10 years of clinical experience) demonstrated that healthcare providers with shorter experience are less confident in their abilities to obtain a long-term adherence and persistence and to involve patients in treatment decisions. They tend to be more prone to using modern approaches to support adherence such as phone applications or videos but the number of participants with <10 years of experience is small; hence results are non-conclusive. For all other aspects, there was no difference between clinicians with short or long clinical experience.
Discussion
Taken together, the main observations of this survey are the following: firstly, HCPs estimated that the initiation, adherence and persistence to antihypertensive medications are far from being ideal even among their own patients. Secondly, HCPs from ESH Centres of Excellence devote little time to discuss antihypertensive medication therapies and patients are infrequently involved in therapeutic decisions. Thirdly, physicians/nurses admit that patients’ beliefs have a great impact on adherence to medications and that a ‘one size fits all’ approach to support adherence does not exist. Fourthly, talking with patients about their medicine use remains the most frequent method to assess medication adherence and the use of other techniques including chemical detection of medications or electronic monitoring to detect non-adherent patients is still infrequent (<30%). Fifthly, simplifying treatment schemes using single-pill combinations, stopping unnecessary medications, combining medication intake with regular daily activities, more frequent consultations, use of reminders, and home blood pressure monitoring are the most commonly used approaches to support long-term adherence. Lastly, the majority of Centres of Excellence have no adherence program and no specific training tools for improving adherence. Yet, they recognise that non-adherent patients are difficult to identify. In few centres, physicians collaborate with nurses but the collaboration with pharmacists is almost inexistent. Over 50% believed that most non-adherence is intentional, which also may influence other answers and interventions considered most effective.
To our knowledge, this is the first survey investigating the beliefs and behaviours of treating patients with hypertension in reference centres. The questionnaire that was used in this survey had been developed by Clyne et al. [Citation13] to examine the perceptions, beliefs and behaviours of primary HCPs, for example, doctors, pharmacists and nurses, about patient medication adherence in 10 European countries. Their first publication reported the answers of 3196 healthcare professionals comprising doctors (855), nurses (1047) and pharmacists (1294) practicing in primary care and community settings [Citation12]. Our survey differs from this initial report as it included almost exclusively physicians (few nurses and no pharmacist) working in secondary and tertiary care centres, mainly universities, and predominantly included those with a long experience in the management of hypertension.
When asked about their perception of the extent of patients’ non-adherence in terms of initiation of therapy, adherence and persistence, participants indicate that a substantial percentage of patients do not initiate the prescribed therapy. The percentage of patients with adherence and persistence >86% is low, for example, <5% for hypertensive patients treated in the community and ∼14% for their own patients. Whether the differences reported between the community and reference centres are true or reflects a healthcare professionals’ optimistic bias cannot be ascertained. Indeed, primary care physicians treating patients with chronic diseases have given similar answers, with their own patients having a higher likelihood to be adherent and persistent [Citation15,Citation16]. Regarding the percentage of patients who do not initiate their medications, the physicians’ perception is in line with data indicating that primary non-adherence, that is, not initiating a prescription, affects 24–28% of patients with hypertension in the United States and is frequent and of the same magnitude in almost all patients with chronic diseases [Citation17,Citation18].
Hypertension is a silent disease needing life-long therapy. Adaptations of prescriptions are frequent due to either insufficient efficacy or to the development of early or late side effects. In addition, barriers to medication adherence are multiple during the follow-up of patients with hypertension [Citation3]. Therefore, the likelihood that patients become non-adherent to medications at one time or another is very high. The time spent during consultations talking about antihypertensive medications is an important component of the long-term success of antihypertensive therapy. Indeed, older studies have shown that consultations of longer duration are associated with greater patient satisfaction, increased health education/prevention measures including more blood pressure measurements, and no increase in prescriptions [Citation19,Citation20]. In our survey, the self-reported time spent discussing medication therapy ranged between 1 and 5 min for ∼50% of participants and between 6 and 10 min for nearly one-third of participants (physicians + nurses). Only about one-third of all (n = 6) participating nurses spent more than 15 min discussing medication treatments with their patients. One might think that these durations are short considering the importance of the issue. However, one should be cautious when concluding because one cannot estimate what these durations represented in terms of proportion of the length of the entire consultation, as we did not find any data on the length of hypertension consultations in reference centres. Moreover, one could not make any distinction between the initial and the follow-up consultations, the former being usually of much longer duration than the latter. Nonetheless, it is interesting to mention that the same distribution of time spent discussing medication therapy was obtained in the primary care survey including more than 3000 doctors, nurses, and pharmacists, respectively 54% for 1–5 min and 25% for 6–10 min [Citation12]. In Europe, the mean duration of primary care consultations is highly variable ranging between 7.6 and 15 min in 2002 with large differences between countries [Citation21] and a trend to increase in recent years in some countries [Citation22]. Hence, these figures would suggest that primary care physicians dedicate little time in discussing medication therapies in patients with chronic diseases. Whether this is also true in secondary care centres would be important to confirm, as it might be a relevant topic of action to improve medication adherence in hypertension.
Recognition of non-adherent patients is a crucial step in the long-term management of hypertension. As expected, most participants perceived that identification of non-adherent patients is not an easy task and that they have only limited practical tools available to perform an effective and reliable detection of non-adherent patients. Our assessment of the methods used to detect non-adherence in hypertensive patients would support this observation. Indeed, asking patients about their medications duration the interview and talking with family members or friends remain the main approaches to get information on how patients manage their antihypertensive medications on a day-to-day basis. Of course, discussing with patients is essential in the doctor-patient relationship, but studies have demonstrated that interviewing patients with uncontrolled blood pressure on adherence has low reliability [Citation23]. Thus, among the various methods available to identify non-adherent patients, HCPs of ESH Centres of Excellence continue to rely mainly on easily available, cheap but poorly reliable methods. To our surprise, more reliable, but also more costly, methods such as chemical detection of medication in blood or urine, electronic monitoring or directly observed treatments are used occasionally by less than 20% of participants. In this respect, reference centres do not differ substantially from general practitioners despite the fact that the availability of reliable methods is usually greater in reference centres. This might change in the future as guidelines are being developed on the set up of some methods such as chemical detection of medications in urine or blood [Citation24]. Thus, many reference centres are now implementing this method of detection with full knowledge of its advantages and limitations (punctual estimation, limited information on duration of effect, white coat adherence).
The interventions used by participants to improve medication adherence in patients with hypertension were very much in line with the latest 2018 ESC/ESH recommendations [Citation1]. Simplification of treatment schemes using single-pill combinations, coupling medication intake with routine activities, recommendations to use home blood pressure monitoring or pill organisers, proposing more frequent consultations in case of apparent resistance to therapy are the most frequently used interventions cited by participants. Interestingly, answers regarding the involvement of family members and nurses are heterogeneous whereas collaborations with pharmacists are scarce. This is rather surprising as more than 80% of participants answered that they had the possibility to collaborate with nurses and pharmacists in their institutions. Several large studies have demonstrated the clinical interest of a team-based collaboration with nurses and pharmacists to improve blood pressure control in hypertension [Citation25–28]. In general, they have shown that the likelihood of controlling blood pressure was higher when a nurse/pharmacist was involved in the management. The development of team-based care programs in Centres of Excellence might be another effective approach to improve and support long-term medication adherence in patients with hypertension, with a possible extension to other chronic diseases [Citation29].
Sharing decisions regarding their antihypertensive treatments and empowering patients are now two strategies strongly recommended by European guidelines [Citation1]. These approaches could facilitate long-term adherence and lead to improved outcomes for patients with hypertension and other chronic cardiovascular diseases [Citation30]. Answers provided by doctors participating in our survey suggest that a large percentage of them are still not using this approach although the large majority of our participants had more than ten years of clinical practice. In accordance with these observations, more than 50% of participants have never had any training on how to conduct an interview on adherence and do not have any adherence program in their centre. This suggests that there is a lot of room for improvement. ESH-based educational programs dedicated to healthcare professionals could be developed in order to promote an effective doctor-patient relation when addressing medication adherence issues.
As with most surveys, our study has several limitations. The first is the rather small sample size and, despite the fact that 30 countries contributed to the survey, analyses according to countries or regions could not be performed. Secondly, the involvement of nurses and pharmacists was small. Thirdly, the survey concerns self-reports by HCPs of the interventions they undertake towards managing and supporting patients with medication adherence. However, we do not have any objective data to confirm their perceptions. It would be of interest to complement this study by a survey involving patients followed in the same centres and to compare, for example, the time dedicated to discussing medications as reported by HCPs and patients. Such an approach was recently used to analyse the quality of BP measurements in dialysis centers [Citation31]. Lastly, participants completing our survey were free to participate. Thus, one cannot exclude that this self-selected sample is affected by a selection bias with participants who are more interested in medication adherence than the HCPs working in all reference centres and other workplaces approaching hypertensive patients.
In conclusion, the present survey indicates that HCPs (largely physicians and nurses) working in ESH Centres of Excellence are well aware of the problems associated with medication adherence in the therapeutic management of hypertension. However, their answers demonstrate that there are major barriers to the ability to detect non-adherence in clinical practice and to implement effective methods to support patients’ adherence. This survey also identifies several aspects of the management of hypertension that could potentially be improved using dedicated educational programs, the involvement of psychologists/sociologists, and/or the implementation of new detection tools.
Supplemental Material
Download Zip (32.2 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041.
- Parthan A, Vincze G, Morisky DE, et al. Strategies to improve adherence with medications in chronic, ‘silent’ diseases representing high cardiovascular risk. Expert Rev Pharmacoecon Outcomes Res. 2006;6(3):325–336.
- Burnier M, Egan BM. Adherence in hypertension. Circ Res. 2019;124(7):1124–1140.
- Corrao G, Parodi A, Nicotra F, et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. 2011;29(3):610–618.
- Perreault S, Dragomir A, Roy L, et al. Adherence level of antihypertensive agents in coronary artery disease. Br J Clin Pharmacol. 2010;69(1):74–84.
- Perreault S, Dragomir A, White M, et al. Better adherence to antihypertensive agents and risk reduction of chronic heart failure. J Intern Med. 2009;266(2):207–218.
- Leslie KH, McCowan C, Pell JP. Adherence to cardiovascular medication: a review of systematic reviews. J Public Health. 2019;41(1):e84–e94.
- Berra E, Azizi M, Capron A, et al. Evaluation of adherence should become an integral part of assessment of patients with apparently treatment-resistant hypertension. Hypertension. 2016;68(2):297–306.
- Tomaszewski M, White C, Patel P, et al. High rates of non-adherence to antihypertensive treatment revealed by high-performance liquid chromatography-tandem mass spectrometry (HP LC-MS/MS) urine analysis. Heart. 2014;100(11):855–861.
- Zeller A, Taegtmeyer A, Martina B, et al. Physicians’ ability to predict patients’ adherence to antihypertensive medication in primary care. Hypertens Res. 2008;31(9):1765–1771.
- Marshall IJ, Wolfe CD, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ. 2012;345:e3953.
- Clyne W, Mshelia C, McLachlan S, et al. A multinational cross-sectional survey of the management of patient medication adherence by European healthcare professionals. BMJ Open. 2016;6(2):e009610.
- Clyne W, Mshelia C, Hall S, et al. Management of patient adherence to medications: protocol for an online survey of doctors, pharmacists and nurses in Europe. BMJ Open. 2011;1(1):e000355.
- Ruppar TM, Dobbels F, Lewek P, et al. Systematic review of clinical practice guidelines for the improvement of medication adherence. Int J Behav Med. 2015;22(6):699–708.
- Clyne W, McLachlan S, Mshelia C, et al. “My patients are better than yours”: optimistic bias about patients’ medication adherence by European health care professionals. Patient Prefer Adherence. 2016;10:1937–1944.
- team Tap [Internet]. Ascertaining barriers for compliance: policies for safe, effective and cost-effective use of medicines in Europe. Final report of the ABC Project (deliverable 7.1). 2012. http://abcproject.eu/img/ABC%20Final.pdf
- Fischer MA, Choudhry NK, Brill G, et al. Trouble getting started: predictors of primary medication nonadherence. Am J Med. 2011;124(11):1081–1089.
- Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25(4):284–290.
- Wilson A. Consultation length in general practice: a review. Br J General Pract. 1991;41(344):119–122.
- Wilson AD, Childs S. Effects of interventions aimed at changing the length of primary care physicians’ consultation. Cochrane Database Syst Rev. 2006;1:CD003540.
- Deveugele M, Derese A, van den Brink-Muinen A, et al. Consultation length in general practice: cross sectional study in six European countries. BMJ. 2002;325(7362):472.
- Cohidon C, Cornuz J, Senn N. Primary care in Switzerland: evolution of physicians’ profile and activities in twenty years (1993-2012). BMC Fam Pract. 2015;16(1):107.
- Meddings J, Kerr EA, Heisler M, et al. Physician assessments of medication adherence and decisions to intensify medications for patients with uncontrolled blood pressure: still no better than a coin toss. BMC Health Serv Res. 2012;12:270.
- Lane D, Lawson A, Burns A, et al. Non-adherence in hypertension: how to develop and implement chemical adherence testing. Hypertension. 2021;
- Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718.
- Clark CE, Smith LF, Taylor RS, et al. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and Meta-analysis. BMJ. 2010;341:c3995.
- Himmelfarb CR, Commodore-Mensah Y, Hill MN. Expanding the role of nurses to improve hypertension care and control globally. Ann Glob Health. 2016;82(2):243–253.
- Ödesjö H, Adamsson Eryd S, Franzén S, et al. Visit patterns at primary care centres and individual blood pressure level - a cross-sectional study. Scand J Prim Health Care. 2019;37(1):53–59.
- Perraudin C, Locca JF, Rossier C, et al. Implementation of an interprofessional medication adherence program for chronic patients in community pharmacies: how much does it cost for the provider? BMC Health Serv Res. 2019;19(1):15.
- Harmon G, Lefante J, Krousel-Wood M. Overcoming barriers: the role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21(4):310–315.
- Pappaccogli M, Labriola L, Van der Niepen P, et al. Is blood pressure measured correctly in dialysis centres? Physicians’ and patients’ views. Nephrol Dial Transplant. 2019;34(9):1612–1615.