Abstract
Purpose
Primary aldosteronism is one of the most frequent causes of secondary arterial hypertension, and whether primary aldosteronism is associated with masked hypertension is unknown.
Materials and methods
We describe a 64-year-old man with a history of hypothyroidism, recurring hypokalaemia, and normal home and office blood pressure values. Ambulatory blood pressure monitoring revealed masked hypertension with strikingly high systolic blood pressure variability and typical hypertension-mediated organ damage.
Results
The patient required gradual escalation of antihypertensive medication to four drugs. During the diagnostic process we identified primary aldosteronism, cobalamin deficiency, severe obstructive sleep apnoea, and low baroreflex sensitivity (1.63 ms/mmHg). Following unilateral adrenalectomy, cobalamin supplementation and continuous positive airway pressure, we observed a spectacular improvement in the patient’s blood pressure control, baroreflex sensitivity (4.82 ms/mmHg) and quality of life.
Conclusions
We report an unusual case of both masked arterial hypertension and primary aldosteronism. Elevated blood pressure values were masked in home and office measurements by coexisting hypotension which resulted most probably from deteriorated baroreflex sensitivity. Baroreflex sensitivity increased following treatment, including unilateral adrenalectomy. Hypertension can be masked by coexisting baroreceptor dysfunction which may derive from structural but also functional reversible changes.
Introduction
Arterial hypertension is a major presenting feature in primary aldosteronism. Comparisons of primary aldosteronism with arterial hypertension to essential hypertension alone, have shown an acceleration of cardiovascular complications in those with co-morbid primary aldosteronism. Considering the negative effects of aldosterone excess on the cardiovascular system and because primary aldosteronism appears to be under detected [Citation1], detailed clinical assessment is needed to ensure appropriate treatment is implemented.
Case report
A 64-year-old man with a history of hypothyroidism was referred to the Department of Hypertension and Diabetology at the Medical University of Gdańsk because of recurring hypokalaemia which required oral supplementation. On admission, the only symptoms reported by the patient were occasional headaches and dizziness. When questioned about a history of hypertension, he said that his blood pressure (BP) had been elevated several years ago and that he used to take three antihypertensive drugs. However, during the following years, his BP had been better controlled and he had even experienced episodes of hypotension. Consequently, his antihypertensive medication had been slowly reduced to one drug. However, this single agent was poorly tolerated and he stopped taking it. When he presented to us, his only medication was thyroxine 50 μg and potassium 20mEq. Drug-induced hypokalaemia and improper nutrition were excluded in the medical interview. His BP was 96/67 mmHg and the rest of the physical examination was unremarkable. Initial laboratory results are presented in .
Table 1. Patient’s test results.
Twenty-four-hour ambulatory blood pressure monitoring performed with SpaceLabs 90207 (Spacelabs Healthcare, Snoqualmie, United States) equipment revealed masked arterial hypertension with an elevated mean BP of 157/93 mmHg. The results also showed a strikingly high systolic BP standard deviation of 43.8 mmHg (). We also identified arterial hypertension complications, including left ventricular hypertrophy and white matter lesions, found on transthoracic echocardiography and central nervous system magnetic resonance imaging, respectively. As a result of the patient’s reverse-dipper BP profile, polysomnography was arranged. This revealed severe obstructive sleep apnoea with an apnoea-hypopnea index of 48. Given the patient’s body mass index of 25 kg/m2 and his excessive amount of upper airway soft tissue, we initiated continuous positive airway pressure therapy and made a referral to laryngology.
Table 2. Ambulatory blood pressure monitoring results.
Because of the patient’s unusually high BP variability, we decided to assess baroreceptor function. Baroreflex sensitivity was assessed from the extracted time series with custom software via the transfer function method in a low-frequency band, (0.04-0.15 Hz) using the technique which expresses baroreflex sensitivity as the average of the transfer function in the low-frequency band. The obtained baroreflex sensitivity was 1.63 ms/mmHg.
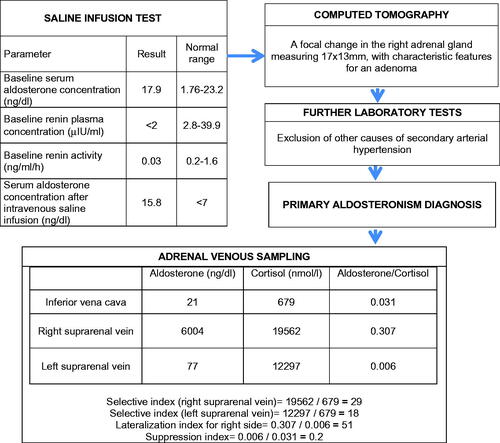
Taking into account the patient’s recurring hypokalaemia and newly detected masked hypertension, further investigation to look for primary aldosteronism was performed (). We confirmed unilateral primary aldosteronism and surgical treatment was planned.
Given the patient’s elevated BP, arterial hypertension complications and tendency for hypotension secondary to baroreflex dysfunction, we initiated hypertension treatment with valsartan 160 mg in the evening and spironolactone 25 mg in the morning; a strategy to escalate treatment slowly was chosen (). Concomitant medication with thyroxine, cobalamin, iron and potassium was continued alongside regular monitoring of blood potassium, haemoglobin and thyroid stimulating hormone levels. During the following weeks, antihypertensive medication was escalated, however, BP control remained inadequate despite the use of four antihypertensive drugs ().
Laparoscopic adrenalectomy of the right adrenal gland was performed and histopathological examination confirmed an adenoma. Following surgery, antihypertensive therapy was significantly reduced due to a marked reduction in the patient’s BP. Home BP values varied greatly, between 60/40 mmHg to 126/90 mmHg. The patient complained of occasional dizziness and reduced tolerance of physical activity, and following further assessment, he was found to have orthostatic hypotension. Accordingly, his antihypertensive medication was again reduced.
During the following weeks, the patient reported better tolerance of physical activity and three months following surgery, ambulatory blood pressure monitoring showed good BP control (). Repeat supine aldosterone and renin plasma levels were 5.1 ng/dl and 12.8μIU/ml, respectively. Repeat assessment of baroreceptor function was performed and baroreflex sensitivity increased to 4.82 ms/mmHg.
Discussion
We described a patient suffering from primary aldosteronism and arterial hypertension masked by baroreceptor dysfunction. Although the patient presented with typical features of primary aldosteronism such as persistent hypokalaemia, pronounced hypertension and target organ damage, some unusual findings were identified. Occasional BP measurements were within normal range and the patient reported previous intolerance to some antihypertensive drugs. Additionally, he was found to have severe obstructive sleep apnoea, despite not being obese. Detailed observation with ambulatory blood pressure monitoring and baroreflex sensitivity assessment allowed us to diagnose primary aldosteronism, and arterial hypertension masked by baroreceptor dysfunction. The patient’s initial estimated baroreflex sensitivity was 1.63 ms/mmHg; baroreflex sensitivity values lower than 3 ms/mmHg have been associated with increased cardiovascular risk [Citation2].
In the presented case, there was no history of mechanical or physical baroreceptor injury and the aetiology of baroreflex dysfunction might be multifactorial including hypertension per se, the effects of aldosterone overproduction, obstructive sleep apnoea, hypothyroidism and cobalamin deficiency.
Firstly, elevated BP leads to increased baroreceptor activity, however, sustained hypertension over time causes baroreceptor activity to decline and baroreceptor adaptation occurs [Citation3]. One of the suggested mechanisms involved in the development of low baroreflex sensitivity in hypertension is activation of 4-aminopyridine sensitive K + channels [Citation3].
Secondly, it is known that baroreceptors are not directly sensitive to BP but to blood vessel distension. Aldosterone per se induces several changes such as vascular remodelling, impaired endothelial-dependent relaxation and enhanced fibrosis, leading to decreased arterial compliance [Citation4]. Another possible mechanism is the direct effect of aldosterone on baroreceptors (as presented in a dog model). In that study, baroreceptor sensitivity was blunted in a dose-dependent manner by carotid sinus perfusion with aldosterone, regardless of arterial compliance [Citation5]. Additionally, a central effect of aldosterone on baroreflex structures such as the nucleus tractus solitarius or peripherally, on efferent sympathetic endings has been postulated [Citation5].
Thirdly, deterioration of baroreceptor function has been linked to obstructive sleep apnoea [Citation6]. However, it has been shown that appropriate management of obstructive sleep apnoea with long-term continuous positive airway pressure therapy (as was administrated in our patient) can reverse obstructive sleep apnoea-related baroreflex dysfunction [Citation6].
Fourthly, thyroid function status influences cardiovascular regulation. Foley et al. described a blunted arterial baroreflex in rats with hypothyroidism in which baroreflex dysfunction was mainly characterised by an impaired response to hypotension [Citation7]. Our patient had a diagnosis of hypothyroidism but was euthyroid as a result of appropriate thyroxine supplementation. Although hypothyroidism can lead to many cardiovascular complications, treatment with L-thyroxine dose tailoring reverses or blunts cardiovascular abnormalities. Restoration of euthyroidism possibly leads to improved baroreflex sensitivity but no data are available to confirm this hypothesis.
Finally, in cobalamin deficiency, orthostatic hypotension may be due to autonomic dysfunction, and this has been attributed to changes in both postganglionic fibres and sympathetic neurons in the brainstem and spinal cord [Citation8]. There is data suggesting that vitamin B12 supplementation can reverse autonomic dysfunction in cobalamin deficiency [Citation8].
Following unilateral adrenalectomy our patient noticed amelioration of his main symptoms (dizziness, tolerance of physical activity) and his BP normalised allowing us to reduce his antihypertensive medication, eventually to a low dose of only one drug. At repeat assessment of his baroreceptor function, baroreflex sensitivity increased to 4.82 ms/mmHg which is above the threshold attributed to increased cardiovascular risk.
Conclusion
We described an unusual case with both masked arterial hypertension and primary aldosteronism. Elevated BP values were masked in both home and office measurements by coexisting hypotension resulting most probably from multifactorial baroreflex dysfunction. We consider the performed unilateral adrenalectomy to be the main factor responsible for improvement in baroreflex sensitivity. Detailed observations with insightful analysis of additional tests allowed us to diagnose primary aldosteronism, and as a result treatments were implemented which produced remarkable improvement in the patient’s BP, baroreflex sensitivity and quality of life.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- Rossi GP. Primary aldosteronism: JACC state-of-the-Art review. J Am Coll Cardiol. 2019;74(22):2799–2811.
- Gouveia S, Scotto MG, Pinna GD, et al. Spontaneous baroreceptor reflex sensitivity for risk stratification of heart failure patients: optimal cut-off and age effects. Clin Sci (Lond). 2015;129(12):1163–1172.
- Chapleau MW, Lu J, Hajduczok G, et al. Mechanism of baroreceptor adaptation in dogs: attenuation of adaptation by the K + channel blocker 4-aminopyridine. J Physiol. 1993;462(1):291–306.
- Briet M, Barhoumi T, Mian MOR, et al. Aldosterone-Induced vascular remodeling and endothelial dysfunction require functional angiotensin type 1a receptors. Hypertension. 2016;67(5):897–905.
- Wang W, McClain JM, Zucker IH. Aldosterone reduces baroreceptor discharge in the dog. Hypertension. 1992;19(3):270–277.
- Bonsignore MR, Parati G, Insalaco G, et al. Continuous positive airway pressure treatment improves baroreflex control of heart rate during sleep in severe obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2002;166(3):279–286.
- Foley CM, McAllister RM, Hasser EM. Thyroid status influences baroreflex function and autonomic contributions to arterial pressure and heart rate. Am J Physiol Heart Circ Physiol. 2001;280(5):H2061–2068.
- Toru S, Yokota T, Inaba A, et al. Autonomic dysfunction and orthostatic hypotention caused by vitamin B12 deficiency. J Neurol Neurosurg Psychiatry. 1999;66(6):804–805.