Abstract
Purpose
May Measurement Month (MMM) is an international screening campaign for arterial hypertension (HT) organised by the International Society of Hypertension and the World Hypertension League. It aims at raising the awareness of elevated blood pressure (BP) in the population. The goal of this analysis was to assess the results obtained in Swiss pharmacies during a 3-year campaign.
Material and methods
Swiss data from the MMM17 to MMM19 campaigns were extracted from the global MMM database. The analysis was conducted specifically on measures taken in pharmacies. BP and a questionnaire including demographical and clinical information were recorded for each participant. To assess BP control, ESH 2018 thresholds of <140/90 mmHg and ESH 2021 pharmacy-thresholds of <135/85 mmHg were used.
Results
From an initial sample of 3634 Swiss participants included during this 3-year campaign, 2567 participants (73.2%women and 26.8% men, p<.001) had their BP measured in triplicates in pharmacies. The first BP measurement was associated with 2.0 ± 4.9 mmHg effect on systolic blood pressure (SBP) (p<.001) and 0.7 ± 3.7 mmHg on diastolic blood pressure (DBP) (p<.001) compared to the mean of the second and third measurements. Based on the ESH 2018 and the ESH 2021 pharmacy thresholds, prevalence of HT (mean of second and third measurements) increased from 29.5% to 38.3%, respectively. In treated participants, 58.3% (279) had an average BP < 140/90 mmHg and 40.3% (193) had an average BP < 135/85 mmHg.
Conclusions
HT screening campaigns in pharmacies recruits mainly women. It helps the detection of untreated hypertensive participants and uncontrolled treated participants. Our data suggest that the average BP should be calculated on the second and third measurements due to a significant first measure effect in pharmacies measurement.
High blood pressure (BP) is a major global public health issue as the leading risk factor of global death.
World-wide initiatives like May Measurement Month (MMM) aim to screen thousands of people each year to raise awareness of hypertension (HT).
Switzerland participated in MMM 2017–2019 and screened more than 2500 participants in pharmacies.
When adopting the recent proposed thresholds of HT diagnosis in pharmacies (ESH 2021 > 135/85 mmHg), HT prevalence in Switzerland is high (38.3%) with only 2/3 of treated hypertensive achieving the BP goals.
Women are more likely to participate in such campaigns taking place in pharmacies.
A first measurement effect (FME) was also present in pharmacies, highlighting that taking three BP measurements in pharmacies and discarding the first should be also considered in the pharmacy setting.
Involving a routine pharmacy-based health care of patients would help to identify more hypertensive patients and uncontrolled treated patients, who may not have had access to BP measurement.
Summary
Introduction
Raised blood pressure (BP) is a major global public health issue as the leading risk factor of global death [Citation1]. Hypertension (HT) prevalence is high and still increasing due to ageing and to the increasing prevalence of obesity worldwide [Citation2]. According to the World Health Organisation (WHO), high BP is responsible for nine million deaths annually worldwide, and it is estimated that nearly one quarter of the adult world population will suffer from HT in 2025 [Citation3]. However, an important proportion of hypertensive patients are unaware of their condition [Citation4–6]. Even patients with established coronary artery disease are unaware of their elevated BP, indicating the need of more efficient cardiovascular prevention programmes [Citation7].
Data from the Swiss Federal Office of Statistics showed that in 2018 ischaemic heart disease was responsible for 54.9% and 25.3% of death in men and women, respectively, and cerebrovascular diseases for 20.4% and 17.4% in men and women, respectively, per 100.000 persons, supporting that early detection and efficient treatment of arterial HT are of high importance. In unselected Swiss adult population-based studies HT ranged from 26% to 37% [Citation8–10].
Consequently, detection of high BP and diagnosis of HT are important in order to define a therapeutic strategy based on BP values and cardiovascular risk. Today, primary care is probably the most frequent place where HT is diagnosed either through systematic routine screening or through opportunistic measurements. However, a significant number of patients do not attend regular primary care consultations [Citation11,Citation12]. Pharmacies, as being the most accessible and frequently visited places compared to other health-care facilities, have been shown valuable in the improvement on BP diagnosis and monitoring of adherence strategies [Citation13–17]. In line with this, the importance of the pharmacist’s role is highlighted in recent guidelines (ACC/HTA2017, ESH 2018, WHO 2021), which support the involvement of non-physician health care professionals (as pharmacists and nurses) in team-based care interventions for the management of HT [Citation18–20].
The recently published 2021 ESH practice guidelines for office and out-of-office blood measurement proposed the adoption of a lower threshold of 135/85 mmHg, as more reasonable for diagnosing HT in the pharmacy setting, based on a meta-analysis of studies comparing BP measurements in pharmacies to other classic BP measurements (office BP, home BP and ambulatory BP monitoring) [Citation16,Citation21].
The low HT awareness was the reason of a worldwide effort to measure BP annually called May Measurement Month (MMM), which aimed at screening people around the world who have not had their BP measured for at least one year. Over 4.2 million participants have been screened worldwide during the 3-year campaign (MMM17–MMM19).
We took the opportunity to coordinate and to test a screening programme in pharmacies of the Canton de Vaud, Switzerland, during MMM 2017 and at a national level in the initiative during MMM18 and MMM19, following the standard MMM protocol. Here we present the results for the pharmacy-based prevalence and control rates of HT in Switzerland.
Materials and methods
Ethics approval for this project was obtained by the local ethics committee (https://www.cer-vd.ch/) (No 2017-00531) and the study was conducted according to the Declaration of Helsinki and International Conference on Harmonisation Guidelines for Good Practice, as revised in 2013. This primary cross-sectional study was performed following ‘The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines’ [Citation22].
Setting
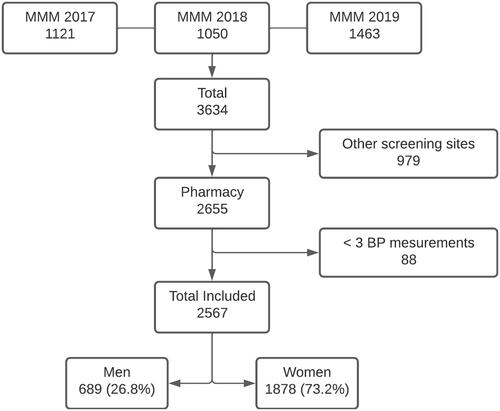
This study uses the Swiss data from the MMM 2017 to 2019 campaigns, which were carried out throughout the month of May in pharmacies of the Canton de Vaud during the MMM17 and in pharmacies in a national level during the MMM18–19. The Lausanne University Hospital (CHUV) served as the coordinating centre. All data were entered directly on the application during the subject’s visit and analysed centrally by the MMM project team in United Kingdom. Swiss data were extracted by statisticians of the MMM programme and sent to the local investigators. Only data from pharmacies (screening site) were used and participants without three consecutive BP measurements were excluded ().
Participants
Eligible patients were adults (≥18 years) willing to participate. Participants were provided with a complete information leaflet about the study and HT facts. All enrolled patients signed a written informed consent.
Variables
Health professionals of the pharmacy screening sites performed three BP measurements at 1 min interval according to international guidelines [Citation23]. BP was preferably measured with a validated automated oscillometric device on the upper arm. Arm circumference was measured and an adapted cuff was used (regular cuff if circumference <32 cm, large cuff if circumference 32–42 cm, extra-large cuff if circumference >42 cm and paediatric cuff if circumference <20 cm). The cuff was placed at the heart level. The patient’s arm being used for the measurement was resting on a table. BP was measured on one arm only, preferably left. Prior to measurement, participants were seated with their backs supported and with their legs, resting on the ground and in the uncrossed position for 5 min. Participants did not smoke immediately before or during the measurement. The BP and heart rate were directly uploaded on the server using the online app provided by the lead organisations of MMM (ISH and WHL).
HT was defined as being on at least one antihypertensive medication (based on the subject’s report) or an average systolic blood pressure (SBP) (mean of the last 2 of 3 readings) ≥140 mmHg and/ or average diastolic blood pressure (DBP) (mean of the last 2 of 3 readings) ≥90 mmHg. For pharmacy-HT (PHT) the threshold of ≥135/85 mmHg was used [Citation23,Citation24].
Among those receiving antihypertensive medication, controlled HT was defined using two thresholds. First, we used SBP of <140 mmHg and DBP of <90 mmHg for the ESH2018 thresholds and second, SBP of <135 mmHg and DBP of <85 mmHg for the pharmacy ESH2021 thresholds. A first measurement effect (FME) was defined as a difference more than +10 mmHg between the first measurement of BP and the average of the second and third measurements, i.e. delta SBP = SBP1-SBP23.
Additional study covariates were collected via sociodemographic and medical questionnaires, which were anonymously collected and uploaded on the app. These covariates included age, gender, alcohol intake and active smoking. Among the self-reported medical conditions were diabetes, stroke and heart attack. Details of all questions included in the questionnaire can be found in the global publication [Citation25]. Measurements of height and weight were taken at the clinical exam and body mass index (BMI) was calculated as kg/m2. Patients were further divided in three groups based on their BMI as: lean (<25 kg/m2), overweight (≥25–<30 kg/m2) and obese (≥30 kg/m2). Additionally, further categorisation according to their age was done as following: <30 years, 30–45 years, 45–60 years and >60 years.
Finally, participants with untreated or uncontrolled HT using the 140/90 mmHg cut-off were supplied with an evidence-based summary of diet and lifestyle modification advice to lower BP. Advice on further follow-up of their BP and its management, tailored to local conditions and the level of BP, was also provided by the local MMM investigators.
Statistical analysis
To proceed with the analysis of the data, we used Stata/IC 16.0 (Stata Corp, College Station, TX). Continuous variables were represented in the form of mean and standard deviation (SD), and categorical variables were represented in the form of percentage (%) and frequency/cases (n). Prevalence was described with proportions by categories of interest.
After validation of data normality, we used t-test and Chi-squared test to compare categorical variables where appropriated. Multivariate logistic regression analyses were used to model the predicted probability of an individual having HT. Statistical significance was defined as p<.05.
Results
Baseline characteristics
From a total sample of 3634 Swiss participants who were included during this 3-year campaign, 2567 participants were recruited only in pharmacies and had three BP measurements. Their mean age was 47.1 ± 18.5 years. Almost ¾ of the participants were women (73.2%) (). Most participants came from an European country (88.2%). Men had a higher cardiovascular risk profile with higher BMI, and an increased prevalence of diabetes, smoking and previous myocardial infarction. Mean systolic BP and diastolic BP were higher in men than in women (130.5 ± 16.4 mmHg vs. 118.6 ± 17.3 mmHg, p<.1 and 80.5 ± 10.7 mmHg vs. 75.8 ± 10.2 mmHg, p<.001).
Table 1. Demographic characteristics of the participants screened in pharmacies.
Effect of three BP consecutive measurements
When examining for the effect of consecutive measurements on BP, the systolic BP decreased from first to the second measurement (−2.0 mmHg, p<.001) and from the second to the third measurement but to a lesser extent (−0.7 mmHg, p<.001) (). The diastolic BP decreased from first to the second measurement (−0.9 mmHg, p<.001) and from the second to the third measurement (−0.4 mmHg, p<.001) (). No differences were observed between men and women in the difference between consecutive readings. Additionally, a FME of more than 10 mmHg was noticed in 8.1% (80) of hypertensives and in 3.7% (58) of normotensives when the pharmacy cut-offs were applied. Moreover, a statistically significant correlation between the baseline SBP and the delta SBP was found (r = 0.33, p value <.001) ().
Figure 2. Relationship between first systolic blood pressure (SBP) measurement and the first measurement effect defined as the change in SBP between the first (SBP1) and the average of the second and third measures (SBP23).
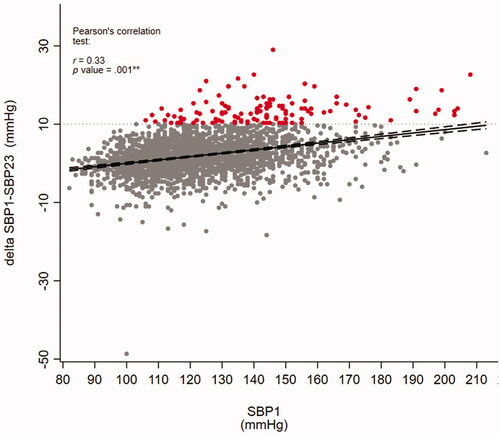
Table 2. Blood pressure values and first measurement effect.
We also assessed the relationship between FME and screening site in the initial cohort and we found no significant association, hence no higher probability of a higher FME in pharmacies compared to other screenings sites.
Prevalence of hypertension
Overall, 29.5% participants were classified as hypertensives according to 2018 ESH criteria (≥140/90 mmHg) and 38.3% participants were classified as hypertensives according to pharmacy-based thresholds (≥135/85 mmHg) ( and ). Prevalence was higher in men, reaching 58.6% using pharmacy cut offs.
Figure 3. Total prevalence of arterial hypertension using ESH 2018 and ESH2021 thresholds, and across BMI and age categories.
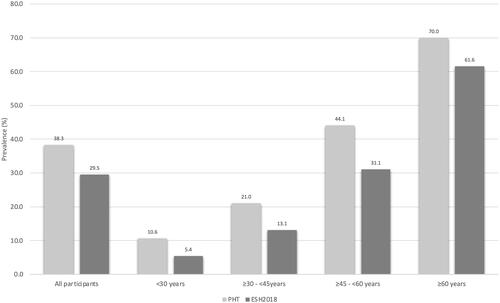
Table 3. Prevalence of arterial hypertension, proportion of treated hypertensives and proportion of treated hypertensives with controlled BP according to PHT-threshold and ESH2018-threshold and by sex.
The prevalence of HT increased across age and BMI categories when using both thresholds (p<.01) ().
Awareness and treatment
When applying the ESH 2018 and pharmacy thresholds, we found that 36.3% and 50.8% of hypertensives, respectively, were not on drug treatment, meaning that they were either unaware of their HT or were not treated for a known HT.
Hypertension control rates
Among treated hypertensive participants, uncontrolled HT was estimated at 41.8% (200) when applying the ESH 2018 and at 59.7% (286) with the pharmacy cut-off values. HT control rate was better in women only when using the ESH 2021 pharmacy’s thresholds (44.4% vs. 34.8%, p=.03) ().
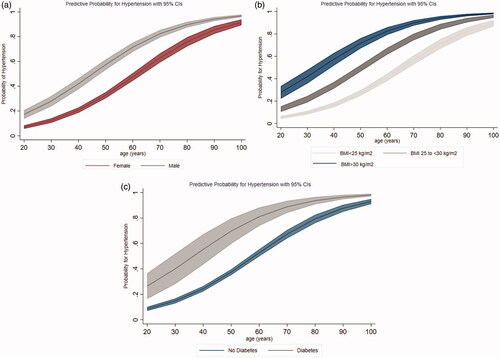
Relationship between hypertension and sociodemographic characteristics
In multivariate logistic regression analysis, the predicted probability of an individual having HT defined by using both thresholds remains significantly associated with gender (men), older age, higher BMI and presence of diabetes (). We found no association with smoking or the level of alcohol intake.
Discussion
The main finding of our study is that the prevalence of HT using the newly proposed thresholds for pharmacies is high (38.3%) and that less than half of treated hypertensives achieve a BP goal <135/85 mmHg in pharmacies, which leaves room for improvement. Women, who represented most of the participants, had higher control rates than men when applying the pharmacy thresholds. Additionally, the higher participation of women suggests that women are more likely to be screened in pharmacies than men, which is consistent with the literature [Citation26–29]. As HT is usually more prevalent in men than women, different strategies should be considered to screen men. In this respect, measuring BP in barbershops has been reported to be effective [Citation30,Citation31]. Nevertheless, men should still be offered a screening in pharmacies because of their low levels of awareness and an unfavourable CV risk profile.
Our results on the prevalence of HT in pharmacies are slightly higher than those found in the Bus Santé study of Geneva (34.4%) and other multi-cantonal cohort studies (34.9%) [Citation9,Citation32,Citation33] but much higher compared to a previously described result for the French-speaking part of Switzerland (25%) [Citation10]. The latter, might be partially explained by the fact that the data from MMM17 concerned only pharmacies from the French-speaking part of Switzerland while the data from MMM18 to MMM19 derived from a national level. Moreover, one cannot exclude some selection bias towards patients with a higher burden of chronic diseases, including HT, presenting to pharmacies.
While the adoption of the 135/85 mmHg threshold probably needs further assessments in future studies, a prevalence of HT in pharmacies of 38.3% during this three-year MMM campaign should be interpreted as a way to highlight the importance of raising awareness of elevated BP and its associated cardiovascular burden via such globally screening programmes. Indeed, these stricter cut offs might help to identify participants at risk and to give an awareness-raising message.
Moreover, despite medical advances and effective BP lowering drugs, a significant number of hypertensives do not achieve the recommended BP goals [Citation34]. In our study, we found that only 40.3% of treated patients achieved a BP <135/85 mmHg and 58.3% a BP <140/90 mmHg. These unsatisfactory results seem to be in line with those shown in a systematic analysis of population studies from 90 countries, were roughly one-half of hypertensives in high-income countries were controlled [Citation35,Citation36]. Thus, the still high rates of uncontrolled HT among patients already on antihypertensive treatment; highlight the global need for a closer follow-up of hypertensives with team-based care approaches involving also pharmacy providers [Citation37–39]. Improvement in the management of HT and other cardiovascular risk factors with pharmacists’ intervention has been supported by several meta-analysis [Citation40–42].
Among hypertensives defined by ESH 2018 and ESH 2021 pharmacy cut-offs, 36.3% and 50.8%, respectively, were not on treatment meaning that either they were unaware of their HT or refused to treat a known HT. A more active role of pharmacies, also including referral to general practitioners in a team-based management, might contribute to enhance education and understanding of the consequence of HT by identifying frequent individual barriers of adherence as the lack of knowledge concerning HT, polypharmacy and difficulties in integrating medication in daily activities [Citation20,Citation37–40,Citation43–45]. Nevertheless, even with a proper counselling on lifestyle modifications and on education of the disease and its consequences in a pharmacy setting, a number of patients are expected not to attend the advised medical appointments with their GP. Thus, ensuring that a proper follow-up in high-risk patients has taken place also seems a challenge for pharmacy providers as being a part of a team-based health approach.
Today, international guidelines suggest performing BP measurements in triplicate with 1 min intervals, in order to eliminate white coat effect. Our results show that the first and second measurements for both SBP and DBP were significantly higher than the third measurement, pointing out the importance of applying the recommendations of using the mean of the last 2 of 3 readings not only in doctors’ offices but also in the pharmacy care setting [Citation21]. Indeed, 5.3% of the participants had a first measurement that was 10 mmHg higher than the second and third measurement. However, previous studies reported contrasting effect of the pharmacy on the white coat effect [Citation28,Citation46,Citation47]. The difference in BP change between pharmacies and other screenings sites was small.
Finally, well-established associations seen between higher BP and increasing age, BMI and sex have also been confirmed in our analysis [Citation48–52]. Additionally, among the known modifiable cardiovascular risk factors, we noted a high prevalence of smoking (22.5%), which is slightly lower than the prevalence of smoking in Switzerland according to the last population-based survey released in 2017 [Citation53]. These findings support the need of a multi-level cardiovascular risk assessment in pharmacies.
Strengths and limitations
Our study presents some visible strength such as the high number of participants in pharmacies. Indeed, this is the first cross-sectional study based on data derived from MMM campaigns, which analysed the prevalence of HT by adopting the recent proposed threshold for screening HT in pharmacy settings. The latter supports the involvement and the potential of pharmacy-based BP screening in health-care programmes.
On the other hand, our study also has particular limitations. First, the BP screening took place on a single occasion, meaning that a proportion of false-positive diagnoses might have arisen, providing overestimation of the true prevalence. However, as previously reported, when adopting the ESH 2021 threshold, our results were almost identical with previous studies in Switzerland [Citation9,Citation10,Citation32,Citation33]. Despite taking the average of the second and third measurement, a possible pharmacy white coat effect with the first measurement is still possible [Citation28,Citation47]. Indeed, we found that a significant first measure effect is present in pharmacies as it occurs when BP is measured by a nurse or a physician [Citation54]. Furthermore, combining data derived from a local and from a national reference during MMM17 and MMM18–19, respectively, may have been a limitation of our study. A selection bias due to the nature of the campaign and the screening site is possible, and may lead to higher inclusion of people with pre-existing HT. Finally, as a cross-sectional study, the definite benefit for those participants being identified as having elevated BP (with or without antihypertensive treatment) and the post-survey impact on awareness was not assessed.
Conclusions
Our findings show a high prevalence of undiagnosed and uncontrolled hypertensive patients screened in Swiss pharmacies. The screening campaign in pharmacies attracts mainly women. BP measurements in pharmacies should follow the same recommended international procedure as a FME is present.
Acknowledgements
All local volunteer investigators, nurses, students and participants. The authors thank the Société Vaudoise de Pharmacies and M. Gérald Ménétré (GaleniCare Management SA) for support in Swiss pharmacies.
Disclosure statement
No conflict of interest is reported by all authors.
Data availability statement
The data that support the findings of this study are available from the corresponding author, [A.D].
References
- World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: World Health Organization; 2009.
- Collaboration NCDRF. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):129–980.
- WHO. A global brief on hypertension: Silent killer, global public health crisis. Geneva, Switzerland: World Health Organization; 2013.
- Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 2020;141(9):e139–e596.
- Neuhauser H, Adler C, Sarganas G. Selective blood pressure screening in the young: quantification of population wide underestimation of elevated blood pressure. Int J Hypertens. 2019;2019:1–8.
- Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, Middle-, and low-income countries. JAMA. 2013;310(9):959–968.
- Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European society of cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26(8):824–835.
- Danon-Hersch N, Marques-Vidal P, Bovet P, et al. Prevalence, awareness, treatment and control of high blood pressure in a Swiss city general population: the CoLaus study. Eur J Cardiovasc Prevent Rehabil. 2009;16(1):66–72.
- Guessous I, Bochud M, Theler J-M, et al. 1999–2009 Trends in prevalence, unawareness, treatment and control of hypertension in Geneva, Switzerland. PLoS One. 2012;7(6):e39877.
- Glatz N, Chappuis A, Conen D, et al. Associations of sodium, potassium and protein intake with blood pressure and hypertension in Switzerland. Swiss Med Wkly. 2017;147:w14411.
- Nwabuo CC, Dy SM, Weeks K, et al. Factors associated with appointment non-adherence among African-Americans with severe, poorly controlled hypertension. PLoS One. 2014;9(8):e103090.
- Macharia WM, Leon G, Rowe BH, et al. An overview of interventions to improve compliance with appointment keeping for medical services. JAMA. 1992;267(13):1813–1817.
- Reeves L, Robinson K, McClelland T, et al. Pharmacist interventions in the management of blood pressure control and adherence to antihypertensive medications: a systematic review of randomized controlled trials. J Pharm Pract. 2020;34:480–492.
- Frazier KR, McKeirnan KC, Kherghehpoush S, et al. Rural patient perceptions of pharmacist-provided chronic condition management in a state with provider status. J Am Pharm Assoc. 2019;59(2):210–216.
- Jokanovic N, Tan EC, Sudhakaran S, et al. Pharmacist-led medication review in community settings: an overview of systematic reviews. Res Social Adm Pharm. 2017;13(4):661–685.
- Albasri A, OʼSullivan JW, Roberts NW, et al. A comparison of blood pressure in community pharmacies with ambulatory, home and general practitioner office readings: systematic review and Meta-analysis. J Hypertens. 2017;35(10):1919–1928.
- Organization WH. Pharmacy-based hypertension management model: protocol and guidelines: a joint CINDI/EuroPharm forum project. Copenhagen: WHO Regional Office for Europe; 2005.
- Al-Makki A, DiPette D, Whelton PK, et al. Hypertension pharmacological treatment in adults: a world health organization guideline executive summary. Hypertension. 2022;79(1):293–301.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. 2018;71(6):1269–1324.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104.
- Stergiou GS, Palatini P, Parati G, et al. 2021 European society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–1302.
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of cardiology and the European society of hypertension: the task force for the management of arterial hypertension of the European society of cardiology and the european society of hypertension. J Hypertens. 2018;36(10):1953–2041.
- Stergiou GS, Palatini P, Parati G, et al. 2021 European society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–1302.
- Beaney T, Schutte AE, Tomaszewski M, et al. May measurement month 2017: an analysis of blood pressure screening results worldwide. Lancet Global Health. 2018;6(7):e736–e743. e43.
- Waszyk-Nowaczyk M, Guzenda W, Plewka B, et al. Screening services in a community pharmacy in Poznan (Poland) to increase early detection of hypertension. J Clin Med. 2020;9(8):2572.
- Schulz M, Griese-Mammen N, Schumacher PM, et al. Development and implementation of blood pressure screening and referral guidelines for german community pharmacists. J Clin Hypertens. 2020;22(10):1807–1816.
- Botomino A, Martina B, Ruf D, et al. White coat effect and white coat hypertension in community pharmacy practice. Blood Press Monit. 2005;10(1):13–18.
- Karwalajtys T, Kaczorowski J, Hutchison B, et al. Blood pressure variability and prevalence of hypertension using automated readings from multiple visits to a pharmacy-based community-wide programme. J Hum Hypertens. 2009;23(9):585–589.
- Boivin JM, Risse J, Lauriere E, et al. Screening for hypertension at the hairdresser: a feasibility study in France and Morocco. Blood Press. 2020;29(4):202–208.
- Hess PL, Reingold JS, Jones J, et al. Barbershops as hypertension detection, referral, and follow-up centers for black men. Hypertension. 2007;49(5):1040–1046.
- Walther D, Curjuric I, Dratva J, et al. High blood pressure: prevalence and adherence to guidelines in a population-based cohort. Swiss Med Wkly. 2016;146:w14323.
- Fidalgo ASQ, Vollenweider P, Marques-Vidal P. Ten-year incidence of hypertension in a Swiss population-based sample incidence of hypertension in Switzerland. J Hum Hypertens. 2019;33(2):115–122.
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.
- Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of Population-Based studies from 90 countries. Circulation. 2016;134(6):441–450.
- Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3(8):e003423.
- Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718.
- Santschi V, Wuerzner G, Pais B, et al. Team-Based care for improving hypertension management: a pragmatic randomized controlled trial. Front Cardiovasc Med. 2021;8:760662.
- Burnier M, Egan BM. Adherence in hypertension: a review of prevalence, risk factors, impact, and management. Circ Res. 2019;124(7):1124–1140.
- Santschi V, Chiolero A, Burnand B, et al. Impact of pharmacist care in the management of cardiovascular disease risk factors: a systematic review and meta-analysis of randomized trials. Arch Intern Med. 2011;171(16):1441–1453.
- Santschi V, Chiolero A, Paradis G, et al. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2012;35(12):2706–2717.
- Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a Meta-analysis. Arch Intern Med. 2009;169(19):1748–1755.
- Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296(21):2563–2571.
- Morgado M, Rolo S, Castelo-Branco M. Pharmacist intervention program to enhance hypertension control: a randomised controlled trial. Int J Clin Pharm. 2011;33(1):132–140.
- Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22(12):1533–1540.
- Sendra-Lillo J, Sabater-Hernandez D, Sendra-Ortola A, et al. Comparison of the white-coat effect in community pharmacy versus the physician’s office: the Palmera study. Blood Press Monit. 2011;16(2):62–66.
- Sabater-Hernandez D, de la Sierra A, Sanchez-Villegas P, et al. Magnitude of the white-coat effect in the community pharmacy setting: the MEPAFAR study. Am J Hypertens. 2011;24(8):887–892.
- Falaschetti E, Mindell J, Knott C, et al. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet. 2014;383(9932):1912–1919.
- Linderman GC, Lu J, Lu Y, et al. Association of body mass index with blood pressure among 1.7 million Chinese adults. JAMA Netw Open. 2018;1(4):e181271.
- Rockwood MR, Howlett SE. Blood pressure in relation to age and frailty. Can Geriatr J. 2011;14(1):2–7.
- Sandberg K, Ji H. Sex differences in primary hypertension. Biol Sex Differ. 2012;3(1):7.
- Cutler JA, Sorlie PD, Wolz M, et al. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52(5):818–827.
- Gmel GK, Notari L, Gmel C. Monitorage suisse des addictions: consommation d’alcool, tabac et drogues illégales en Suisse en 2016–2017. Addiction Suisse, Lausanne, Suisse. https://www.suchtmonitoring.ch/docs/library/gmel_2tl0igxj1e6t.pdf
- Gerc V, Favrat B, Brunner HR, et al. Is nurse-measured blood pressure a valid substitute for ambulatory blood pressure monitoring? Blood Press Monit. 2000;5(4):203–209.