Abstract
Purpose
The current study examined the effects of chronic stress and a genetic risk score on the presence of hypertension and elevated systolic blood pressure and diastolic blood pressure among Hispanics/Latinos in the target population of Hispanic Community Health Study/Study of Latinos.
Materials and Methods
Of the participants (N = 11,623) assessed during two clinic visits (Visit 1 2008–2013 & Visit 2 2014–2018), we analysed data from 7,429 adults (50.4% female), aged 18–74, who were genotyped and responded to chronic stress questionnaires. We calculated an unweighted genetic risk score using blood pressure increasing single nucleotide polymorphisms (SNPs) found to be generalisable to Hispanics/Latinos (10 SNPs). Linear and logistic regression models were used to estimate associations between chronic stress and genetic risk score and their interaction, with prevalent Visit 2 SBP or DBP, and hypertension, respectively. Models accounted for sampling weights, stratification, and cluster design.
Results
Chronic stress (adjusted OR = 1.18, 95%CI:1.15,1.22) and hypertension genetic risk score (adjusted OR = 1.04, 95%CI:1.01,1.07) were significantly associated with prevalent hypertension, but there was no significant interaction between the chronic stress and genetic risk score on hypertension (p = .49). genetic risk score (b = .32, 95%CI:.08, .55, R2 = .02) and chronic stress (b = .45, 95%CI:.19, .72, R2 = .11) were related to DBP, with no significant interaction (p = .62). Genetic risk score (b = .42, 95%CI:.08, .76, R2 = .01) and chronic stress (b = .80, 95%CI:.34,1.26, R2 = .11) were also related to SBP, with no significant interaction (p = .51).
Conclusion
Results demonstrate the utility of a genetic risk score for blood pressure and are consistent with literature suggesting chronic stress has a strong, direct association with elevated blood pressure among U.S. Hispanics/Latinos.
Main text introduction
Hypertension, or high blood pressure, is one of the strongest risk factors associated with CVD in the United States (U.S.); however, the disease is poorly treated and controlled among U.S. Hispanics/Latinos [Citation1]. There has been recent interest in the contribution of genetic variants to hypertension. Genome-wide association studies (GWAS) of hypertension have identified several genetic risk variants; however, few variants have been replicated among Hispanic/Latino populations. In terms of both non-modifiable risk factors, hypertension risk is associated with age, gender, race, sedentary lifestyle, poor diet, obesity, diet, diabetes, smoking, and chronic stress [Citation2]. Further, although there are many different conceptualizations of stress, chronic stress, specifically, has been found to be associated with increased hypertension among U.S. Hispanics/Latinos [Citation1]. However, the existing literature lacks investigation into whether chronic stress interacts with genetic risk to impact hypertension development [Citation3].
Gene-environment studies and studies comparing whether distinct risk factors differentially operate among minority populations are useful in helping to identify those with elevated risk from those with lower risk. Thus, providing the opportunity to identify better strategies to improve fidelity for treatment and control of hypertension, impacting disparities observed in hypertension for Hispanics/Latinos and other minority groups [Citation4]. The International Consortium for Blood Pressure Genome-Wide Association of systolic and diastolic blood pressure has investigated single nucleotide polymorphisms, single base-pair variations in a DNA sequence, associated with systolic, diastolic, mean arterial, and pulse blood pressure [Citation4]. Sixteen novel loci involved with blood pressure regulation in persons of European descent were identified [Citation4]. Few loci have been replicated among Hispanics/Latinos; however, recent GWAS have identified several single nucleotide polymorphisms associated with differences in systolic and diastolic blood pressure and are generalisable to Hispanics/Latinos [Citation5,Citation6]. Although there is minimal genetic variability between populations, the expression of genes is highly dependent on the environment [Citation7]. For example, an explanation for the observed is the distinct socio-cultural environments and intergenerational health effects of societal issues that work to affect gene expression and health differences rather than the small genetic variation that is observed between groups at the genetic level [Citation7–9].
By understanding how genes and lifestyle factors differentially impact and may interact to affect hypertension development, we can better characterise those who are at increased risk. Therefore, the objective of the current study was to assess the extent to which genetic risk score for blood pressure predicts the prevalence of hypertension, to evaluate any observed differences in genetic risk scores between Latin American and Caribbean ethnic groupings, and to assess the extent to which chronic stress is associated with the prevalence of hypertension in U.S. Hispanics/Latinos in the target population of HCHS/SOL [Citation10,Citation11]. Further, additional aims were to investigate whether chronic stress and genetic risk score interact in the association with hypertension and SBP and DBP among U.S Hispanics/Latinos.
Materials and methods
Participants and procedures
The HSHC/SOL is a population-based study of 16,415 Hispanic/Latino adults, aged 18–74 (M = 53.32, SD= 13.16), recruited at four field centres (Bronx, NY, Chicago, IL, San Diego, CA, and Miami, FL). Data for HCHS/SOL were collected during a baseline examination cycle (2008 to 2011) and a follow-up examination cycle (October 2014 to December 2017) (Visit 2). On average, the second examination for participants was conducted 6–7 years after the baseline examination. The main study variables included in the present study were from the follow-up examination (Visit 2) due to the availability of specific questionnaires of interest collected during that examination cycle, specifically the chronic stress questionnaire. A total of 7,429 Hispanic/Latino participants (5676 women), aged 18–74 (M = 53.32, SD = 13.16) who responded to the Visit 2 chronic stress questionnaires and were genotyped contributed to analyses in the present study.
HCHS/SOL participants self-identified as one of seven Hispanic/Latino background groups (Central American, South American, Mexican, Cuban, Dominican, Cuban, Puerto Rican, or Other/Multiple backgrounds). Institutional Review Board approval was obtained and written informed consent was obtained from all selected participants. The selection of study participants included a multi-stage probability sampling. Methods have been described by prior studies in greater detail [Citation12,Citation13]. Visit 2 sampling weights were generated to address disproportionate sampling at each stage and to partially adjust for bias resulting from differential nonresponse in the sample at the person and household levels, which result in a final sample with age, sex, and Hispanic/Latino background characteristics that reflect the communities [Citation12]. Participants completed a baseline clinical examination during which information on birthdate, Hispanic/Latino background, diet quality, and sedentary behaviour was collected. During Visit 2, questionnaires were, again, administered by interviewers and collected the following information: demographic information, education, and occupational history. Interviews for self-report information were conducted by certified assessors who were bilingual, allowing interviews to be conducted in either English or Spanish (language groups), depending on participant preference.
Blood pressure measurement
Systolic and diastolic blood pressures are averages of three consecutive readings taken during Visit 2 with participants in a seated position using the Omron HEM 907XL sphygmomanometer. The pulse and blood pressure were measured in the right arm of all participants [Citation11,Citation12]. Hypertension was defined according to recommendations by the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) at the time the study was conducted and those used in the GWAS papers (a systolic blood pressure [SBP] greater than or equal to 140 mmHg or diastolic blood pressure [DBP] greater than or equal to 90 mmHg) [Citation14].
Chronic stress
Chronic stress burden was assessed during Visit 2 using an 8-item scale that addresses the number of ongoing health problems occurring for at least six months in major life domains. These domains include financial, work, relationship, health issues in oneself or close other, drug or alcohol issues in a close other, caregiving, or another chronic stressor (i.e. Many people experience ongoing problems with their everyday lives. Please tell us whether any of the following has been a problem for you. 1. Have you had a serious ongoing health problem?, 2. Has someone close to you had a serious ongoing health problem?). From this, a summary score was calculated, which indicated the total number of stressors with a minimum six-month duration (range 0–8) and was used in analyses. Higher scores represented a higher number of chronic stressors present for participants during a six-month period. This measure of chronic stress has been used in other cohorts besides HCHS/SOL and is meant to be generally applicable across varied sociodemographic groups [Citation15,Citation16].
DNA extraction and genotyping
DNA of HCHS/SOL participants was extracted from blood collected during Visit 1 and genotyped on an Illumina custom array, HCHS/SOL Custom 15041502 B3, consisting of the Illumina Omni 2.5 M array and 150,000 custom SNPs [Citation10].
Construction of genetic risk score and SNP selection
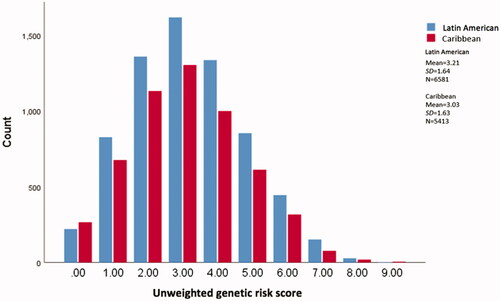
The present study utilised 10 blood pressure increasing-associated SNPs that reached significance levels within or were generalisable to Hispanic/Latino samples in Franceschini and colleagues’ 2016 study and Sofer and colleagues’ 2017 study [Citation5,Citation6]. An unweighted genetic risk score was calculated using a summed approach such that a 10 mmHg change in blood pressure per each increasing blood pressure risk allele was estimated by the sum of the risk alleles across SNPs (range 0 to 20 alleles). In this approach, each SNP takes on a value from 0 to 2 depending on the number of risk alleles known to increase blood pressure, and the total sum represents the unweighted genetic risk score [Citation17]. In our study, an unweighted risk score was used, such that each SNP allele counts equally in the genetic risk score. Higher genetic risk scores indicate an increased genetic predisposition for high blood pressure. Additionally, based on the results of the findings from the Conomos et al. [Citation10] study we broadly defined two ethnic groupings based on self-reported Hispanic/Latino background (Central American, Cuban, Dominican, Mexican, Puerto Rican, and South American. The Latin American group (Mexicans, Central Americans, and South Americans) consisted of persons with a larger relative proportion of Amerindian ancestry than those in the Caribbean group (Cuban, Dominican, and Puerto Rican) [Citation5,Citation6,Citation10].
Covariates and baseline auxiliary variables
Visit 2 sociodemographic covariates included age, sex(male/female), Latin American/Caribbean analysis grouping, study site, education (<high school, > high school), income (less than $20000, $20,000–50000, >$50000), health insurance status (yes/no). Visit 1 auxiliary variable included demographics (income, education), behavioural risk factors (sedentary behaviour, dietary sodium intake, and biologic risk factors (BMI, age, and Visit 1 blood pressure) (reason for inclusion specified in statistical analyses section below). BMI was computed as weight (kg)/height (m2). Sedentary behaviour was based on self-reported time spent sedentary (defined as either sitting or reclining in min/day). Dietary sodium intake (mg/day) was calculated based on available 24-hour dietary recalls obtained from participants. In total, two 24-hour dietary recalls were collected during HCHS/SOL baseline period. The first recall was collected in person at the clinic, and the second recall was collected by telephone within three months of the first recall. Calculations were conducted based on items in the Alternative Healthy Eating Index a questionnaire that measures diet quality based on components predictive of chronic disease risk [Citation18]. The full score is derived from eleven components (vegetables, whole fruit, whole grains, sugar-sweetened beverages, nuts, red meat, trans fat, long-chain fats, polyunsaturated fatty acids, sodium, and alcohol); however, we used a single component of dietary salt intake (mg/day) in analyses, which was calculated based on information obtained through the 24-hour dietary recalls.
Statistical analyses
Before testing associations between genetic risk score, chronic stress, and blood pressure, we first assessed the data for missingness and obtained descriptive statistics for all study variables using SPSS V24. All analyses accounted for complex survey design and weighting accounted for the sampling design of HCHS/SOL. Preliminary analyses were additionally conducted to test whether the first five principal components of ancestry based on genotyped data should be included as covariates in regression analyses. The inclusion of principal components did not alter results in the models tested. This result is similar to findings from other genetic risk score analyses [Citation19]. However, the first five principal components were controlled for in the present analyses as this is the standard across genetic risk score investigations [Citation20]. Genetic risk score, chronic stress, systolic blood pressure, and diastolic blood pressure were measured continuously and the presence of hypertension was measured categorically (yes/no). The genetic risk score and chronic stress variables were centred and multiplied to test the effect of interaction between the two variables on the presence of hypertension. Statistical adjustments were made in all models for relevant covariates: sex (male/female), age, recruitment site (Brooklyn, NY, San Diego, CA, Chicago, IL, and Miami, FL), Visit 2 SES (income and education), Visit 2 health insurance status (yes/no), broad ethnic background group (Latin American and Caribbean) in all models. To account for the HCHS/SOL sampling design, which included genetically related individuals and individuals living in the same household and community block unit, linear or logistic mixed models with correlations modelled via kinship, household sharing and community block unit sharing matrices were used.
Logistic regression analyses were performed using SPSS version 24 using complex survey procedures to estimate associations between genetic risk score and chronic stress with hypertension. Linear regression analyses were performed in Mplus version 8 to estimate associations between genetic risk score and chronic stress with systolic blood pressure and diastolic blood pressure. To improve Visit 2 blood pressure prediction in linear models, specifically for participants on antihypertensive medication, their blood pressure readings were treated as missing data, and full information maximum likelihood estimation was used with a Visit 1 auxiliary variable model. The practice of adding a constant to systolic blood pressure, and diastolic blood pressure, 15 mmHg and 10 mmHg, respectively, for participants taking antihypertensive medication, does not adequately control for the dampening effect on blood pressure observed for participants on oral antihypertensive medications [Citation21]. Visit 1 auxiliary variable related to blood pressure (defined above) was also included in linear models to improve the prediction of blood pressure at Visit 2.
Results
Mean scores and standard deviations for each primary study variable are included in and . Both the unstandardised and standardised regression coefficients for hypertension, systolic blood pressure, and diastolic blood pressure across genetic risk score and chronic stress are presented in and ; however, only unstandardised coefficients are commented on in the present section. After adjusting for potential confounders, we found that genetic risk score independently was associated with hypertension, systolic blood pressure, and diastolic blood pressure in this population (OR = 1.04, 95%CI:1.01,1.07 [See ]; b = .42, 95%CI:.08, .76; b = .32, 95%CI:.08, .55, respectively [See ]). Additionally, after adjustment for potential confounders, we found that chronic stress also independently relates to hypertension, systolic blood pressure, and diastolic blood pressure in this population (OR = 1.18, 95%CI:1.14,1.22 (See ]; b = .80, 95%CI:.34,1.26; b = .45, 95%CI:.19, .72; respectively [See ]). However, we found no significant interaction between genetic risk score and chronic stress, as evidenced by statistically non-significant interaction terms, in relation to prevalent hypertension (p = .49), or high SBP (p = .51) or DBP (p = .62).
Table 1. Characteristics of the target population of HCHS/SOL.
Table 2. Means and standard deviations of main study variables.
Table 3. Adjusted logistic regression model results for chronic stress and GRS on prevalent hypertension at HCHS/SOL visit 2.
Table 4. Adjusted linear regression model results for chronic stress and genetic risk score on systolic blood pressure (SBP) and diastolic blood pressure (DBP).
Further, genetic risk score frequency and range across Hispanic/Latino ethnic groups (Latin American and Caribbean) are depicted in , with higher genetic risk scores indicating greater genetic susceptibility. The mean genetic risk score (M = 3.21, SD = 1.64) found for Latin American Hispanics/Latinos was slightly higher than the mean genetic risk score (M = 3.03, SD = 1.63) found for Caribbean Hispanics/Latinos (). However, both groups followed similar distribution trends and ranges related to genetic risk scores (). Finally, across models, genetic risk score accounted for less than 2% of the variability in systolic blood pressure and diastolic blood pressure, whereas chronic stress accounted for 11% of the variability in systolic blood pressure and diastolic blood pressure.
Discussion
To our knowledge, the current study is among the first to investigate the application of a genetic risk score for hypertension and blood pressure based on a population-based Hispanic/Latino cohort and the possible interaction between genetic risk score and chronic psychosocial stress. We found an association between the genetic risk score, which was derived from ten validated Hispanics/Latinos blood pressure increasing SNPs, and prevalent hypertension and blood pressure (systolic blood pressure and diastolic blood pressure) among a diverse sample of U.S. Hispanics/Latinos. We also found that the mean and distribution of genetic risk scores differed slightly between Latin American and Caribbean background groups (). Additionally, our findings replicated the longstanding literature concerning the proposed positive association between chronic stress with hypertension and blood pressure, specifically among U.S. Hispanics/Latinos [Citation3,Citation22]. Our results also indicated that chronic stress explained a larger proportion of variance than genetic risk score in systolic blood pressure and diastolic blood pressure. However, we found no significant interactions between chronic psychosocial stress and genetic risk score on prevalent hypertension and elevated blood pressure based on the data included in the current study.
Main effect of genetic risk score on the presence of hypertension and elevated blood pressure
Results from the current study demonstrated a significant positive association between the combination of recently identified genetic risk variants generalisable to U.S. Hispanics/Latinos and hypertension and systolic blood pressure and diastolic blood pressure across models tested [Citation5,Citation6]. This finding is important as a significant main effect was detected from the limited number of SNPs included in the study based on their validation in Hispanics/Latinos, despite the limitations of genetic risk score predictability discussed in the prior section. Findings from this study further support the literature that genetic risk scores are useful predictors of diseases, as significant associations were found using an unweighted genetic risk score constructed from a relatively small number of SNPs [Citation23]. However, the mechanisms through which these genetic loci are related to blood pressure are still being understood [Citation3]. Further, genetic risk scores have potential clinical utility as part of a precision medicine approach as they improve predictability in disease risk [Citation24]. This study further contributes to the potential uses for genetic risk scores as predictors of disease among non-European samples.
We found a difference in mean genetic risk scores between Latin American and Caribbean Hispanic/Latino groups. Caribbean Hispanics/Latinos have a higher proportion of African ancestry and face unique environments compared to Latin American [Citation5–7]. This finding supports the use of groupings based on ancestral population differences within the admixed Hispanic/Latino population determined by prior studies [Citation25]. We found that the Latin American group had a higher average genetic risk score when compared to the Caribbean group (See ). The genetic risk score used in the present study was calculated using GWAS single nucleotide polymorphisms from a large meta-analysis of individuals of European descent and may perform better among populations with higher European ancestry admixture, such as the Latin American group. The unweighted genetic risk score in the present study may have masked the effect of individual single nucleotide polymorphisms such that the single nucleotide polymorphisms found at a higher frequency among Caribbean Hispanics/Latinos have larger associated effects weights. Notably, we did not investigate differences in environment between the two groups that also may have affected gene expression. Future studies should work to incorporate better sociocultural and intergenerational factors that may be associated with observed disparities into analyses [Citation7].
Main effects of chronic stress on hypertension and elevated blood pressure
Our findings support the current literature suggesting that chronic stress is significantly positively associated with hypertension and systolic blood pressure and diastolic blood pressure, specifically among a diverse sample of U.S. Hispanics/Latinos. While chronic stress has long had a hypothesised positive association with hypertension and high blood pressure, there remain a limited number of cohort and case-control studies investigating this association [Citation3]. Further, there are even fewer studies investigating the role of chronic stress among U.S. Hispanics/Latinos [Citation22]. Our findings are consistent with a previous study that reported a cross-sectional association between chronic stress and hypertension prevalence in a subset of participants from the HCHS/SOL baseline cohort; however, we are unaware of any other studies that have explored this association in a diverse U.S. Hispanic/Latino sample using blood pressure and hypertension [Citation22].
While the associations found in this study between chronic stress and hypertension and blood pressure were small in magnitude, it should be noted that standardised associations were larger in magnitude than a genetic risk score. Further, in the linear regression models testing the main effects of genetic risk score and chronic stress on systolic blood pressure and diastolic blood pressure, genetic risk score accounted for 1.0% and 1.5% of the variance in systolic blood pressure and diastolic blood pressure, respectively, while chronic stress, based on 8 domains (financial, work, relationship, health issues in oneself or close other, drug or alcohol issues in a close other, caregiving, or another chronic stressor), accounted for 11% of the variance in both systolic blood pressure and diastolic blood pressure, which is somewhat higher than effects reported by other studies [Citation3,Citation26]. These findings are significant as they suggest that among U.S. Hispanics/Latinos, stress is more strongly associated with hypertension and high- blood pressure than genetic risk. Practically, our findings suggest that for U.S. Hispanics/Latinos with four chronic stressors, we would expect to see a 4 mmHg increase in systolic blood pressure and 2.25 mmHg in diastolic blood pressure. While this is comparatively less than the 10 mmHg difference in systolic blood pressure and 5 mmHg in diastolic blood pressure observed based on medication therapies, this finding highlights the utility of a combination approach focussed on both medication and stress interventions to more greatly lower blood pressure among hypertensive U.S. Hispanics/Latinos [Citation27].
Interaction effects between genetic risk score and chronic psychosocial stress
Our study found no interaction between blood pressure increasing SNPs and chronic stress based on 8 domains (financial, work, relationship, health issues in oneself or close other, drug or alcohol issues in a close other, caregiving, or another chronic stressor) for U.S. Hispanics/Latinos. The pathophysiology of hypertension is complex, with several established environmental and psychosocial risk factors, and recently identified genetic risk factors [Citation5,Citation6]. Other studies have failed to detect interactions between genetic risk scores and environmental factors. For example, Krogarger and colleagues (2018) found no significant interaction effect between genetic risk scores, constructed from 300 blood pressure increasing SNPs, and age on hypertension in a population-based cohort of 4,809 individuals. Possible explanations for a lack of interaction cited by other studies include the need to use variants with higher p-values, the need for a larger number of single nucleotide polymorphisms, small sample sizes, and differences between individual stress profiles [Citation27]. However, our results, and other studies’ results, failing to detect interactions between genetic risk and psychosocial stress, may also suggest that while gene-environment interactions are a growing area of research interest, genes may not interact with lifestyle factors across all disease outcomes to impact disease progression.
This study had several notable strengths and limitations. A major strength of the current study is the use of a genetic risk score for blood pressure variants among Hispanic/Latinos in the United States. Further, the present study’s use of a genetic risk score that combined information from ten SNPs related to elevated blood pressure can aid future approaches in identifying U.S. Hispanics/Latinos at higher risk for developing hypertension. The use of blood pressure increasing SNPs for Hispanics/Latinos is a novel and important strength of this study, as there has been a bias towards individuals of European descent in genome-wide association studies [Citation24].
There are also several points to consider when interpreting the findings from the present study. An unweighted genetic risk score was calculated from a limited number of single nucleotide polymorphisms and used in the current analyses. The relative effect size (beta coefficient), used to calculate a weighted genetic risk score, was unavailable because the present study drew from two separate GWAS [Citation5,Citation6]. Additionally, only single nucleotide polymorphisms generalisable to Hispanics/Latinos were used, and the relatively small number of single nucleotide polymorphisms (10 single nucleotide polymorphisms) may not have the predictive power to detect a gene × environment interaction. It remains possible that there are other major population-variants that were excluded from the current analyses based on our definition of single nucleotide polymorphisms.
Additionally, hypertension risk is associated with age, gender, race, sedentary lifestyle, poor diet, obesity, diet, diabetes, smoking, and chronic stress [Citation2]. Although the present analyses controlled for age and sex, it remains possible that these other risk factors impacted the results of the present study. It would be prudent for future studies to take a more intersectional approach when investigating risk factors across outcomes.
Conclusions
In summary, results from this study provide clear evidence that genetic risk score is associated with hypertension and high blood pressure among a diverse population of U.S. Hispanics/Latinos. Further, the findings support the literature by confirming genetic differences between Latin American and Caribbean Hispanics/Latinos. A genetic predisposition for the increased blood pressure may interact with other lifestyle factors, such as age, gender, race, sedentary lifestyle, poor diet, obesity, diet, diabetes, smoking, and chronic stress, yet not interact with chronic stress for U.S. Hispanics/Latinos [Citation2]. Additionally, the findings from this study support the continued need for GWASs to include diverse populations to obtain a more precise use of genetic risk scores among non-European populations. Increased standardisation in the construction and use of genetic risk scores may become an essential feature in the clinical effort to provide more targeted, population-specific hypertension prevention and intervention strategies. Further, an increased understanding of the mechanism through which risk factors, like chronic stress and genetic risk score, are differentially associated with hypertension among U.S. Hispanics/Latinos could help create culturally-informed management strategies for hypertension, which could work to improve controlled hypertension among this population.
Supplemental Material
Download MS Word (13.7 KB)Acknowledgements and funding
The Hispanic Community Health Study/Study of Latinos is a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (HHSN268201300001I/N01-HC-65233), University of Miami (HHSN268201300004I/N01-HC-65234), Albert Einstein College of Medicine (HHSN268201300002I/N01-HC-65235), University of Illinois at Chicago – HHSN268201300003I/N01-HC-65236 Northwestern Univ), San Diego State University (HHSN268201300005I/N01-HC-65237).
The authors thank the participants for their contribution to the current study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Sorlie PD, Allison MA, Avilés-Santa ML, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic community health study/study of Latinos. Am J Hypertens. 2014;27(6):793–800.
- Center for Disease Control (CDC). 2017. Hypertension: data & statistics. Available from: https://www.cdc.gov/nchs/fastats/hypertension.htm.
- Liu M, Li N, Li WA, et al. Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurol Res. 2017;39(6):573–580.
- Ehret GB, Munroe PB, Rice KM, et al. Genetic variants in novel pathways influence BP and cardiovascular disease risk. Nature. 2011;478(7367):103–109.
- Franceschini N, Carty CL, Lu Y, et al. Variant discovery and fine mapping of genetic loci associated with BP traits in Hispanics and African Americans. PLOS One. 2016;11(10):e0164132.
- Sofer T, Wong Q, Hartwig FP, et al. Genome-wide association study of BP traits in the Hispanic community health study/study of Latinos (HCHS/SOL). Sci Rep. 2017;7(1):10348.
- Bliss C. Conceptualizing race in the genomic age. Special Report: For “All of Us”? on the Weight of Genomic Knowledge, Hastings Center Report. 2020;50(3):S15–S22.
- Braun L, Fausto-Sterling A, Fullwiley D, et al. Racial categories in medicine: How useful are they? PLOS Med. 2007;4(9):e271.
- Cuevas AG, Dawson BA, Williams DR. Race and skin color in latino health: an analytic review. Am J Public Health. 2016;106(12):2131–2136.
- Conomos MP, Laurie CA, Stilp AM, et al. Genetic diversity and association studies in US Hispanic/Latino populations: Applications in the Hispanic community health study/study of Latinos. Am J Hum Genet. 2016;98(1):165–184.
- CDC. 2015. Community health assessments & health improvement plans. November 2015. Available from: https://www.cdc.gov/stltpublichealth/.
- Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection for the Hispanic community health study/study of Latinos. Ann Epidemiol. 2010;20(8):642–649.
- Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic community health study/study of Latinos. Ann Epidemiol. 2010;20(8):629–641.
- Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high BP in adults: executive summary. J Am Coll Cardiol. 2017;71(19):e127–e248.
- Bromberge JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychol Aging. 1996;11(2):207–213.
- McCurley JL, Mills PJ, Roesch SC, et al. Chronic stress, inflammation, and glucose regulation in U.S. Hispanics from the HCHS/SOL sociocultural ancillary study. Psychophysiology. 2015;52(8):1071–1079.
- Lim NK, Lee JY, Lee JY, et al. The role of genetic risk score in predicting the risk of hypertension in the Korean population: Korean genome and epidemiology study. PLOS ONE. 2015;10(6):e0131603.
- Chiuve S, Fung T, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009–10018.
- Belsky DW, Moffit TE, Sugden K, et al. Development and evaluation of a GRS for obesity. Biodemography Soc Biol. 2014;59(1):85–100.
- Choi SW, Mak TS-H, O'Reilly PF. Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc. 2020;15(9):2759–2772.
- Tobin MD, Sheehan NA, Scurrah KJ, et al. Adjusting for treatment effects in studies of quantitative traits: antihypertensive therapy and systolic BP. Stat Med. 2005;24(19):2911–2935.
- Gallo LC, Roesch SC, Fortmann AL, et al. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the Hispanic community health study/study of Latinos sociocultural ancillary study. Psychosom Med. 2014;76(6):468–475.
- Elfassy T, Zeki Al Hazzouri A, Cai J, et al. Indcidence of hypertension among U.S. Hispanics/Latinos: the Hispanic community health study/study of Latinos, 2008-2017. J Am Heart Assoc. 2020;9:e015031.
- Martin AR, Kanai M, Kamatani Y, et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nature. 2019;51:584–591.
- Nelson SC, Stilp AM, Papanicolaou GJ, et al. Improved imputation accuracy in Hispanic/Latino populations with larger and more diverse reference panels: applications in the Hispanic community health study/study of Latinos (HCHS/SOL). Hum Mol Genet. 2016;25(15):3245–3254.
- Sparrenberger F, Cichelero FT, Ascoli AM, et al. Does psychosocial stress cause hypertension? A systematic review of observational studies. J Hum Hypertens. 2009;23(1):12–19.
- Svensson T, Kitlinski M, Engstrom G, et al. A genetic risk score for CAD, psychological stress, and their interaction as predictors of CAD, fatal MI, non-fatal MI and cardiovascular death. PLOS ONE. 2017;12(4):e0176029.
- Krogager ML, Kuhr Skals R, Appe EV, et al. Hypertension GRS is associated with burden of coronary heart disease among patients referred for coronary angiography. PLOS One. 2018;3:e0208645.