Abstract
Purpose
Home blood pressure monitoring (HBPM) might be considered a valid alternative to ambulatory blood pressure monitoring (ABPM) for both the diagnosis and management of hypertension. Correct information on how to perform HBPM are crucial for its reliability. The aim of the present survey was to assess if hypertensive patients followed current recommendation on how to correctly perform HBPM measurements.
Materials and methods
The survey included 30 different items on how to perform the HBPM. It was developed by the ‘Young Investigators’ group of the Italian Society of Arterial Hypertension (SIIA) and it was administered during the office visit between May 2019 and December 2021.
Results
A total of 643 hypertensive patients participated in the study. Main results show that, despite the rate of informed patients was relatively high (71% of the whole population), unacceptable number of patients did not follow indications on how to perform a correct HBPM. Patients who were informed on how to measure home BP had a significantly higher rate of correct position during measurement (78 vs. 22%, p < 0.01), avoidance of talking and moving during measurement (68 vs. 32%, p < 0.0001), and correct number and time interval between two measurements (85 vs. 15%, p < 0.001). More accurate measurements of home BP were associated with less prevalence of carotid plaque.
Conclusions
Correct performance for HBPM is low among patients treated in Italian hypertension centers. These findings shed light on the importance of correct HBPM measurements for the detection of accurate BP values for the proper management of hypertensive patients.
Introduction
Methods for measuring blood pressure (BP) to detect a diagnosis of systemic arterial hypertension (HT) have undergone considerable change in the past decades. The bulk of knowledge about the risks of HT and the benefits of treating it is based on the traditional method of taking a small number of readings using the auscultatory or automated oscillometric technique in a medical setting (i.e. ‘in-office’ BP measurement). However, there is increasing evidence that such measures may have some limitations, such as the poor observer technique, the white-coat effect and BP variability, that reduce their diagnostic and predictive power in terms of cardiovascular (CV) risk [Citation1]. Therefore, the most recent European [Citation2] and American guidelines [Citation3] for the management of HT strongly recommend the use of ‘out-of-office’ BP monitoring for confirming new diagnoses of HT, detecting white-coat and masked HT, and managing BP control during the follow-up. Twenty-four hours ambulatory BP monitoring (ABPM) and home BP monitoring (HBPM) are the two main approaches to out-of-office BP evaluation [Citation4]. Twenty-four-hour ABPM is usually regarded as the gold standard, especially for the diagnosis of HT, for personalizing treatment according to BP profile, and for the prediction of clinical outcomes [Citation2–4]. However, it has some issues, such as the high cost of devices and not being widely available in primary care practice. Furthermore, it may also be uncomfortable resulting in poor tolerance in several patients [Citation5]. On the other hand, HBPM, which involves the use of commercially available, validated, automated devices that patients use on their own to measure BP, is better accepted and is more accessible to physicians [Citation4]. It represents an accurate and reasonable alternative method, especially for confirming the initial diagnosis of HT [Citation4], and also for predicting hypertension-mediated organ damage (HMOD) [Citation6] and CV outcomes [Citation7,Citation8]. In several studies, HBPM has been reported superior to ‘in-office’ BP as predictor of both HMOD [Citation6,Citation9] and clinical outcomes [Citation7]. Some disadvantages of HBPM might also be reported such as the need for patient training, lack of nocturnal BP readings and possible induction of anxiety resulting in excessive monitoring [Citation4]. According to the guidelines, for the technique effectiveness and self-monitoring of BP values reproducibility, patients must follow a strict procedure (e.g. sitting position, several minutes rest, correct cuff size, etc.), using validated tools, with priority automatic brachial devices, as recommended by the guidelines [Citation2–4]. Following these indications the risk of under- or overestimation of BP values is low, and the reproducibility and the accuracy of this technique increases [Citation4]. To date, available data on patients’ adherence to HBPM recommendations are still limited to few surveys [Citation10–12] in which it has been proved that only a small proportion of hypertensive patients is informed on how to correctly measure BP at home and is able to strictly follow the correct recommendations.
The current article presents the results of a national survey conducted among Italian society Hypertension Centers, with the aim of investigating the degree of adherence to current recommendations on HBPM.
Methods
The ‘Young Investigators’ research working group of the Italian Society of Arterial Hypertension (SIIA) developed a survey on how hypertensive patients perform the BP measurement at home. This survey was administered between May 2019 and December 2021. The survey was developed according to the 2018 ESH/ESC guidelines for the management of arterial hypertension [Citation2]. It was sent to the SIIA members and was spread to Italian Hypertension Centers. Ten centers collected all data with a mean number of patients recruited at each center described in Supplemental Table 1.
Participants were invited to join the survey during the control visit for hypertension in one of the certified Italian Hypertension Center. The participation was voluntary and confidential, and each responder could withdraw at any point. All the invited patients, performing home BP measurements, agreed to respond to the survey.
The questionnaire was administered in the office, just after the routine clinical visit, using an online platform. The first section, regarding anthropometric data and CV history, was filled in by the patient with the help of the physician. The next section including nine questions was related on how to measure the BP at home and patients were asked to answer independently (). Office BP values and the type of in-office BP measurement device were added by physicians at the end of outpatient’s examination (see detailed list in the Supplementary Material). Systolic and diastolic BP were measured in the sitting position by a validated automatic sphygmomanometer after 5 min of rest. Consistent with the current guidelines, BP was measured three times at 2 min intervals and the average of the last two BP readings was taken as the BP [Citation2]. Home BP was self-reported by patients as the last measurement performed at home. The presence of carotid plaque and left ventricular hypertrophy (LVH) were defined according to the current guidelines [Citation2] and investigated during the clinical visit.
Table 1. Questions used for total score calculation.
The study was performed under Article 89 of the General Data Protection and Regulation, which allows the processing of personal data for archiving purposes in the public interest, scientific or historical research purposes or statistical purposes, provided that technical and organizational measures are in place to ensure the principle of data minimization (https://gdpr-info.eu). All patients gave their informed consent to participate in the survey. The study was conducted in accordance with the principles of the Declaration of Helsinki. The study has been approved by ethical committee of University Milano Bicocca.
Statistical analysis
Statistical analysis was performed using IBM SPSS 23 (IBM Corporation, Armonk, NY, USA). Data are presented as mean ± SD for continuous variables and as percentages for categorical variables. Analysis of variance and χ2 distribution were used for exploratory statistics. A total score of good knowledge on how to correctly measure home BP was built for the main questions on BP measurement, assigning one point for each correct answer as detailed in . Pearson’s correlations were used for assessing significant variables associated with higher score. Then a logistic regression model was used to assess whether the total score impact on the presence of carotid plaque and LVH. The model was built also including age, sex, office systolic and diastolic BP values, diabetes, obesity and dyslipidemia. The null hypothesis was rejected at a two-tailed α ≤ 0.05.
Results
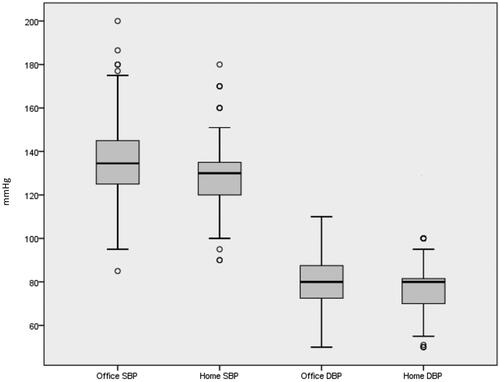
The present survey included answers from 643 patients. Main characteristics of the study population are reported in . Both systolic and diastolic BP values were significantly higher in office compared to those reported at-home BP measurements (p < 0.0001, ).
Table 2. Demographic characteristic of the study population.
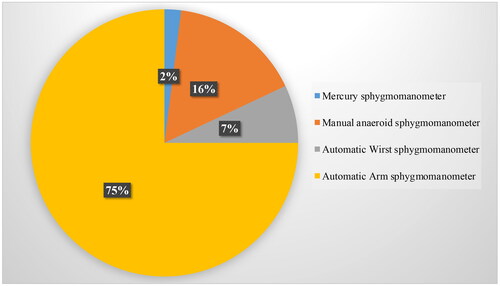
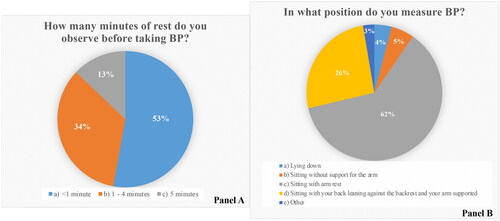
Of the total study population, 458 patients (71%) were declared to have received oral information previously from physicians on how to measure BP at home. No significant difference in age or sex was found among patients who received or not received information on home BP measurement (both p > 0.05). Most of the patients (75%) used automatic arm BP device for measuring BP at home, while other not recommended devices were quite commonly used (). Regarding resting time before home BP measurement, only 13% of the study population declared to correctly wait for 5 min, while most of the study population (53%) waited only 1 min before detecting the measurement (). Correct position during BP measurement was declared only by 26% of the study population (), while talking or movements were correctly avoided by less than 50% (Supplemental Figure 1). Only 2% of the interviewed patients declared to not have removed clothes before home BP measurements and 55% of the study population avoided tea, coffee or food immediately before home BP measurements (Supplemental Figure 2). Around 16% of the patients interviewed declared to measure BP only in the presence of symptoms and only 25% correctly measured BP two times with 1 min interval (Supplemental Figure 3). Home BP was measured one to two times per week by 41% of the patients (Supplemental Figure 4).
Figure 3. Rate of patients who affirmed to observe 5 min rest before taking blood pressure (BP) (A) and in what position they measure BP values at home (B).
Mean score obtained by patients was 4 ± 2 with normal distribution (Supplemental Figure 5). In Pearson’s correlation analysis, higher score was significantly associated with younger age, lower systolic BP in office and at home, less prevalent dyslipidemia, hypertension-mediated vascular and renal damage (all p < 0.05). Higher score was also significantly associated with higher prevalence of well-controlled values of in-office BP (p < 0.05). Higher score was not associated with lower differences between office and home BP values (p > 0.05) (Supplemental Data, ).
In a logistic regression model, the presence of carotid plaque was associated with lower total score, independent of the significant effect of male gender, office systolic BP and the presence of dyslipidemia. The presence of LVH was not influenced by the total score ().
Table 3. Logistic regression model for hypertensive mediated target organ damage, including total score of knowledge on how to correct measure home blood pressure.
Discussion
To the best of our knowledge, this is the first study assessing adherence to current recommendations during home BP measurement in a cohort of hypertensive patients referred to certified Hypertension centers of the SIIA.
Initial management of hypertension conventionally requires a diagnosis based on several clinic or office BP measurements. However, the most recent national and international guidelines [Citation2–4] suggest that, besides the ABPM, which is the more accurate estimator of ‘true’ mean BP, the HMBP could provide an appropriate alternative to ambulatory monitoring in terms of diagnosis, particularly in primary care where it might not be immediately available or deemed too costly or when patients find it inconvenient or uncomfortable [Citation13]. Although this potential role of HMBP in the management of hypertensive patients, data about how patients detect their BP values at home are missing. Moreover, it has not been clarified yet whether patients routinely received information on how to correctly measure BP at home. Interestingly, in our survey, we observed that information on how to perform a correct HBPM were not achieved by one out of three patients, and these data pointed out on how physicians should play a pivotal role in patient’s education and support the value of HBPM. Even if different studies have highlighted its crucial role for identifying white coat and masked hypertension [Citation13,Citation14], systematic mistakes in HBPM might be dangerous misleading hypertension diagnosis, treatment and control. Compared to a previous study conducted in Canada [Citation15] where the rate of patients who received information on how to perform HBPM was 30%, our study demonstrated that 70% of subjects affirmed receiving HBPM indications. A national field survey conducted in Turkey a few years ago demonstrated that among hypertensive patients the ownership of a home BP monitor was associated with lower BP values, although 50% stated that they have not had any training regarding the operation of the device and 18% used wrist device [Citation16]. The use of wrist devices in our population was not negligible (7%). As previously reported, this results in frequent detection of falsely elevated BP values likely because of poor memory and rendition of the instructions, leading to the wrong wrist position [Citation17].
In line with an Italian survey recently performed, some of the recommended procedures for HBPM were followed by most patients, but the level of adherence to other important recommendations was unacceptably low [Citation10]. Despite not being considered useful for HBPM, 18% of the study population declared to use aneroid and mercury sphygmomanometers at home. Aneroid apparatus requires frequent calibration to maintain accuracy and are not suggested for HBPM, while mercury sphygmomanometers are not allowed by the Italian law since 2009 but are still available for some of our patients. Only 13% of the study population declared to observe resting time before the measurement, in line with results from previous research [Citation10,Citation12]. Moreover, incorrect position during the BP measurement at home (reported by 38% of our interviewed) may lead to a significant difference in the reported BP values underling that this aspect is crucial for optimal HBPM [Citation18]. Prior literature suggests, in fact, that taking BP with the back unsupported may falsely elevate pressure levels by 6 mmHg to 10 mmHg [Citation19] and that crossing the legs may increase systolic BP by 2 mmHg to 8 mmHg [Citation20]. In this regard, the higher prevalence of incorrect body position reported in our survey may help to improve area of necessary training in HBPM.
We also observed that higher accuracy in HBPM measurement was significantly correlated with lower office BP values and more prevalence of controlled BP. This is in line with previous studies, demonstrating that self-monitoring of BP might be a good strategy to improve long-term BP control [Citation16,Citation21]. Nevertheless, compliance with HBPM is the main determinant of improved BP control rate [Citation22].
Finally, there are evidences that home BP is a better predictor of the development of carotid atherosclerosis than office BP, supporting the crucial role of home BP in the detection of HMOD [Citation23]. Our results highlight that more accurate measurements of home BP were associated with less prevalent of carotid plaque, strongly supporting the evidence that the accuracy of HBPM is of paramount relevance for the management of hypertensive patients. LVH was not associated with the accuracy of HBPM, and this finding is not surprising since other metabolic factors, such as obesity, strongly influence its progression and/or regression [Citation24].
Limitations
The present survey was administered during control visits of patients followed in Italian Hypertension specialist centers and thus the main results may not entirely reflect the whole community of hypertensive patients in Italy. The study was in part conducted during the COVID-19 pandemic, which might have partially influenced the selection of the patients. Also, a larger sample size would have also been desirable. Unfortunately, data on socioeconomic status, level of education and treatment adherence were not available in the present study.
Conclusions
The accuracy of home BP is low among patients treated in hypertension centers belonging to the SIIA. Higher accuracy is associated with better office BP control and less prevalent carotid plaque, which strongly encourage to plan strategies with the aim to improve the performance of home BP measurement.
Supplemental Material
Download MS Word (2.3 MB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Melville S, Byrd JB. Out-of-office blood pressure monitoring in 2018. J Am Med Assoc. 2018;320(17):1805–1806.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104.
- Whelton PK, Carey RM, Aronow WS, et al. PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–248.
- Parati G, Stergiou GS, Bilo G, et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the Working Group on Blood Pressure Monitoring and Cardiovascular Variability of the European Society of Hypertension. J Hypertens. 2021;39(9):1742–1767.
- Baguet JP. Out-of-office blood pressure: from measurement to control. Integr Blood Press Control. 2012;5:27–34.
- Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30(7):1289–1299.
- Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: Follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111(14):1777–1783.
- Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. J Am Med Assoc. 2004;291(11):1342–1349.
- Mulè G, Caimi G, Cottone S, et al. Value of home blood pressures as predictor of target organ damage in mild arterial hypertension. J Cardiovasc Risk. 2002;9(2):123–129.
- Flacco ME, Manzoli L, Bucci M, et al. Uneven accuracy of home blood pressure measurement: a multicentric survey. J Clin Hypertens. 2015;17(8):638–643.
- Wagner S, Toftegaard TS, Bertelsen OW. Challenges in blood pressure self-measurement. Int J Telemed Appl. 2012;2012:437350.
- Wagner S, Buus NH, Jespersen B, et al. Measurement adherence in the blood pressure self-measurement room. Telemed J E Health. 2013;19(11):826–833.
- Hodgkinson J, Mant J, Martin U, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: Systematic review. BMJ. 2011;342:d3621–d3621.
- Kario K. State-of-the-art review: home blood pressure monitoring: current status and new developments. Am J Hypertens. [2021 cited Feb 9]; hpab017.
- Bancej CM, Campbell N, McKay DW, et al. J. Home blood pressure monitoring among Canadian adults with hypertension: results from the 2009 survey on living with chronic diseases in Canada. Can J Cardiol. 2010;26:152–157.
- Akpolat T, Arici M, Sengul S, et al. Home sphygmomanometers can help in the control of blood pressure: a nationwide field survey article. Hypertens Res. 2018;41(6):460–468.
- Casiglia E, Tikhonoff V, Albertini F, et al. Poor reliability of wrist blood pressure self-measurement at home: a population-based study. Hypertension. 2016;68(4):896–903.
- Kallioinen N, Hill A, Horswill MS, et al. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. J Hypertens. 2017;35(3):421–441.
- Cushman WC, Cooper KM, Horne RA, et al. Effect of back support and stethoscope head on seated blood pressure determinations. Am J Hypertens. 1990;3(3):240–241.
- Pinar R, Ataalkin S, Watson R. The effect of crossing legs on blood pressure in hypertensive patients. J Clin Nurs. 2010;19(9–10):1284–1288.
- Tzourio C, Hanon O, Godin O, et al. Impact of home blood pressure monitoring on blood pressure control in older individuals: a French randomized study. J Hypertens. 2017;35(3):612–620.
- Choi J-Y, Kim K, Kim C-H. Effect of home blood pressure monitoring for blood pressure control in hypertensive patients taking multiple antihypertensive medications including fimasartan (the FORTE study). Clin Hypertens. 2020;26(1):1–9.
- Tachibana R, Tabara Y, Kondo I, et al. Home blood pressure is a better predictor of carotid atherosclerosis than office blood pressure in community-dwelling subjects. Hypertens Res. 2004;27(9):633–639.
- Lønnebakken MT, Izzo R, Mancusi C, et al. Left ventricular hypertrophy regression during antihypertensive treatment in an outpatient clinic (the Campania salute network). J Am Heart Assoc. 2017;6:e004152.