Abstract
Purpose
The coronavirus disease 2019 (COVID-19) pandemic and the subsequent lockdown profoundly affected almost all aspects of daily life including health services worldwide. The established risk factors for increased blood pressure (BP) and hypertension may also demonstrate significant changes during the pandemic. This study aims to determine the impact of the COVID-19 pandemic on BP control and BP phenotypes as assessed with 24-hour ambulatory BP monitoring (ABPM).
Materials and Methods
This is a multi-centre, observational, retrospective and comparative study involving Excellence Centres of the European Society of Hypertension across Europe. Along with clinical data and office BP, ABPM recordings will be collected in adult patients with treated arterial hypertension. There will be two groups in the study: Group 1 will consist of participants who have undergone two ABPM recordings - the second one occurring during the COVID-19 pandemic, i.e. after March 2020, and the first one 9–15 months prior to the second. Participants in Group 2 will have two repeated ABPM recordings - both performed before the pandemic within a similar 9–15 month interval between the recordings. Within each group, we will analyse and compare BP variables and phenotypes (including averaged daytime and night-time BP, BP variability, dipper and non-dipper status, white-coat and masked hypertension) between the two respective ABPM recordings and compare these changes between the two groups. The target sample size will amount to least 590 participants in each of the study groups, which means a total of at least 2360 ABPM recordings overall.
Expected outcomes
As a result, we expect to identify the impact of a COVID-19 pandemic on blood pressure control and the quality of medical care in order to develop the strategy to control cardiovascular risk factors during unpredictable global events.
PLAIN LANGUAGE SUMMARY
What is the context?
A wide range of daily activities, including health care worldwide, were deeply affected by the Coronavirus disease 2019 pandemic and the subsequent lockdown.
What is new?
Our multicenter study will examine the impact of the COVID-19 pandemic on blood pressure control in hypertensive patients across Europe by analysing results of 24-hour ambulatory blood pressure monitoring.
What is the impact?
Optimising strategies for dealing with future unpredictable global situations will depend on understanding how the pandemic affected blood pressure control.
Background
The coronavirus disease 2019 (COVID-19) pandemic and associated lockdown at the beginning of the pandemic severely affected social, economic, and other aspects of daily life. Adverse consequences extended to the well-being and health of people around the world [Citation1,Citation2] as well as to control of cardiovascular risk factors which have been reported to have changed substantially during the pandemic [Citation3].
Due to COVID-19 lockdown numerous aspects of hypertension management were compromised in many countries around the world possibly because of the infection itself but also because imposed restrictions and fear of infection [Citation3].To quote few examples, treatment with angiotensin converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB) is the backbone of antihypertensive therapy according to the current Guidelines of the European Society of Cardiology (ESC) and European Society of Hypertension (ESH) for the management of arterial hypertension [Citation4]. However, shortly after the outbreak of COVID-19 concerns were raised that use of renin-angiotensin system (RAS) inhibitors might increase the risk and/or the severity of infection by SARS-CoV-2 [Citation5,Citation6]. Although unsubstantiated by subsequent dedicated studies [Citation7] this led to discontinuation of treatment with these drugs in a noticeable number of patients [Citation1]. It has been also reported that patients recovering from SARS-CoV-2 infection may show persistently elevated BP via activation of the RAS or the sympathetic nervous system, due the consequences of previous prolonged periods of mechanical ventilation or to other factors [Citation8]. Finally, it is common perception that during the COVID-19 and lockdown-related pandemic a limited access to medical consultations and pharmacies, a delayed the diagnosis of hypertension, and an increased therapeutic inertia had unfavourable consequences for the control of BP of hypertensive patients, perhaps lasting beyond the duration of the COVID-19 pandemic [Citation1,Citation9].
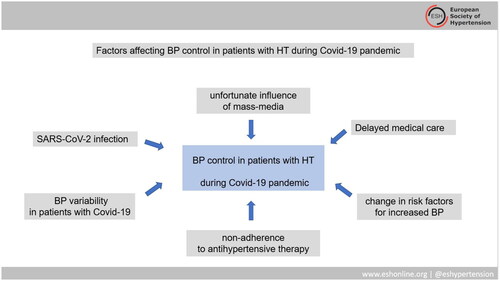
Although multiple factors could potentially affect BP control of hypertensive patients during COVID-19 pandemic () actual BP data during and at temporal distance from the COVID-19 pandemic are few and inconsistent. There are data showing that home BP was similar or lower during the lockdown and a reference period selected over the corresponding time window a year before [Citation10]. On the other hand, data from a large observational study in the United States, (more than half a million subjects) showed a rise in average BP during the early peak of the pandemic [Citation11]. Moreover, the impact of COVID-19 on office BP [Citation12,Citation13] and out-of-office BP [Citation13,Citation14] control has been recently indicated. Based on the differences between office BP and out-of-office BP, we can conclude that the pandemic had a complex effect on BP.
Aim of the present ongoing study is to assess the impact of the COVID-19 pandemic on BP values and phenotypes assessed and identified by ambulatory BP monitoring (ABPM) through the comparison of ABPM results obtained before and during the COVID-19 pandemic in hypertensive patients.
Study design
The ESH ABPM COVID-19 Study was initiated by the Scientific Council of the ESH and consists of a retrospective analysis of data made available by specialised European hypertension units including the European Society of Hypertension (ESH) Excellence Centres. The study is conducted according to the principles outlined in the Helsinki declaration for investigations in human subjects, general data protection regulations, and after approval of the study protocol by the local Ethics Committee in the countries of participating centres.
Overview
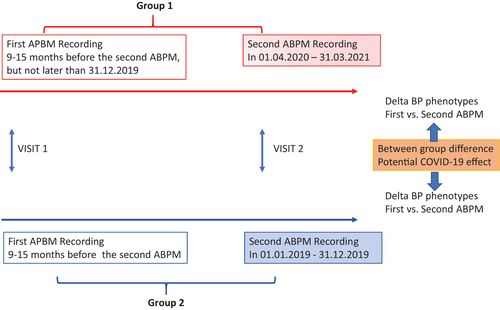
This analysis includes two different groups. The first group consists of participants with two repeated ABPM recordings, the second obtained during the COVID-19 pandemic and the first prior to the pandemic. The starting point of the pandemic is defined by the official announcement of the World Health Organisation (WHO), i.e. March 11th in 2020 (). The second group includes participants with two repeated ABPM recordings performed before the COVID-19 pandemic and the two pre-COVID-19 ABPMs have to be recorded not less than 9 and not more than 15 months apart. Besides ABPM, the study also collects clinical data, including office BP measurements, antihypertensive medication, other clinical information, and COVID-19 history.
Inclusion criteria
Data from patients with pharmacologically treated hypertension whose age is at least 18 years are collected. Office systolic and diastolic BP and heart rate have to be available. Patients will be required to have two valid ABPM recordings.
Patients with ABPM obtained during the pandemic period will be assigned to Group1 with available repeated ABPMs, where the first ABPM (visit 1) was obtained 9–15 months before the second ABPM recording, but not later than 31.12.2019; and the second ABPM (visit 2) was obtained during the pandemic period, namely between 01.04.2020 and 31.03.2021.
Group 2 will include patients who had both ABPM recordings prior to the pandemic period: first ABPM (visit 1) obtained 9–15 months before the second ABPM and second ABPM (visit 2) obtained between 01.01.2019 and 31.12.2019 ().
Exclusion criteria
Study-specific exclusion criteria include a diagnosis of secondary hypertension, pregnancy, Parkinson disease, device-based treatment of hypertension, alcohol or drug abuse, and development of any of the following condition: heart failure, myocardial infarction, cardiac surgery, or cancer between ABPM measurements.
Primary and secondary study goals
The primary goal of the study is to compare the impact of COVID-19 pandemic on the difference of averaged 24-hour systolic and diastolic BP between visits in Group 1 and Group 2.
Secondary goals
The secondary goals will be the differences between groups in:
average daytime (awake) and night-time (asleep) BP;
the prevalence of white–coat hypertension, masked hypertension, and resistant hypertension;
nocturnal blood pressure falls and prevalence of dipper/non-dipper phenotypes;
short-term BP variability;
morning surge.
Data collection
The data are collected through the analysis of patient records. After identifying repeated BP measurements taken by ABPM at predefined intervals, a review of the relevant clinical data will also be conducted. The study personnel will be responsible for pseudonymizing the personal data of the patients. A unique number that contains the centre identification will be assigned to consecutive patients. Each participating centre will use a standardised data form to enter all available data. For the analysis, an anonymized raw data file containing individual ABPM measurements should be exported from ABPM software used locally, whenever possible.
Office blood pressure (OBP)
Data on OBPs will be extracted from clinical records. It is recommended that the database contain data from at least two standard measurements. In the absence of OBP, the first BP measurements from ABPM will be recorded in the database.
Ambulatory blood pressure monitoring
Only recordings from validated oscillometric devices are accepted. Centres participating in the study provide details about the model of the device used. Recommendations are for both recordings to be performed with the same device in the same patient. Information from the logbook regarding sleep and awakening times should be provided if available.
The average of 24-hour systolic (SBP24h) and diastolic (DBP24h) BP as well as awake BP, asleep BP, and 24-hour heart rate will be analysed. Awake and asleep periods will be defined as fixed time intervals (as defined in each centre). Whenever log-book records of actual wake and sleep time will be available, awake and asleep values will also be calculated based on this information. We will only analyse ABPMs of adequate quality, i.e. with at least 20 valid awake and seven valid asleep measurements [Citation15].
To assess the night-time BP phenotype, the size of nocturnal BP fall will be calculated as % reduction from daytime average and the following categories of participants according to day-night BP profiles will be identified: (1) dippers (10–20% nocturnal fall in systolic BP); (2) non-dippers: (0–10% nocturnal fall in systolic BP) (3) risers (increase in systolic BP during the night compared to daytime values) and (4) extreme dippers (>20% nocturnal fall in systolic BP).
In subjects in whom the actual awakening time registered in the logbook will be available, morning surge will be calculated according to the method proposed by Hoshide et al. [Citation16].
The short-term BP variability will be estimated by calculation of the standard deviation (SD) of the average 24 h, awake and asleep values.
In case of raw data availability, additional indices of short-term BP variability will be calculated: (1) average real variability (ARV), computed as the average of the absolute differences between consecutive BP measurements over 24-hour [Citation17]; (2) weighted 24-hour SD, computed as the average of daytime and night-time SD weighted for the duration of these respective periods [Citation18]. To account for the dependence of the above indices on average BP levels, the corresponding coefficients of variation (CV) will be calculated. The BP variability parameters will be analysed in case of balanced availability of raw data in both studied groups.
Blood pressure measurement and definitions
Sustained hypertension will be defined as elevated BP values both in OBP (SBP ≥140 and/or DBP ≥ 90 mmHg and in ABPM phenotyping (averaged 24-h ambulatory BP ≥130 and/or 80 mm Hg) [Citation15]. True resistant hypertension will be defined as sustained hypertension in participants treated with at least 3 antihypertensive drugs including a diuretic. White-coat hypertension will be defined as an elevated OBP (SBP ≥140 and/or DBP ≥ 90 mmHg with ABPM values within normal range (averaged 24-h ABPM<130 and < 80 mmHg) [Citation15]. Masked hypertension will be defined as a normal OBP (<140 and <90 mmHg) with elevated ABPM values (averaged 24-h ambulatory BP ≥130 and/or 80 mmHg) [Citation15].
Data management and statistical analyses
The primary objective of this study is to determine the influence of COVID-19 pandemic on BP values as assessed by ABPM through the comparison of ABPM results obtained before and during pandemic period.
We will first assess whether in Group 1 significant changes in BP (averaged 24-h SBP and 24-h DBP) measured during pandemic occurred in comparison to BP obtained in the year preceding the COVID-19 pandemic. Next, we will assess whether in Group 2 significant changes in BP (averaged 24-h SBP and 24-h DBP) measured in the years before the pandemic occurred within an about one-year time interval. Then we will compare the observed changes (deltas) in average BP (24-h SBP and 24-h DBP) over 1 year between Group 1 and Group 2. We will also evaluate the predictors of BP changes in both groups. We will analyse the changes in other BP phenotypes (awake and asleep averaged SBP and DBP), BP variability, and in white-coat and masked hypertension prevalence in Group 1 and Group 2 and will compare the between groups differences.
To realise the study purpose, the sample size is estimated to obtain at least 80% power for the observed difference in averaged 24-h SBP within Group 1 of at least 3 mm Hg. The study is designed to enrol at least 590 participants with repeated ABPM in each of the study group, which means a total number of 2360 ABPMs.
Statistical analysis
Descriptive statistics will be calculated for both study groups separately. For comparison of means and proportions (clinical and BP data) within studied groups a t-test for paired observations and the Chi2 statistic, respectively, or Wilcoxon Signed Rank test, for nonparametric data will be used. Between-group comparisons will be executed with adjustment for baseline BP. Between group comparison in BP changes from first to second visit will be assessed by ANCOVA in GLM procedure. In multivariate regression model the predictors of BP changes in Group 1 and Group 2 will be identified. The prevalence of white coat and masked hypertension in each visit will be assessed for both groups and then comparison of proportions will be calculated in Chi2 statistic and logistic regression.
Exploratory subgroup analyses then will be conducted in participants with resistant hypertension, white-coat, and masked hypertension. Additionally, we will conduct exploratory subgroup analyses based on the following parameters: age, gender, country, body mass index, duration of hypertension history. These subgroup analyses will be conducted on variables of interest if the prevalence of the condition is at least 15% in the sample.
Discussion
Available studies showed the impact of COVID-19 on cardiovascular complications and major cardiovascular risk factors including hypertension [Citation1,Citation19,Citation20]. However, the impact of the COVID-19 pandemic on BP control and hypertension remains still insufficiently explored.
The control of BP is affected by lifestyle factors such as physical activity, dietary factors, smoking, and excessive alcohol use [Citation4]. Several behavioural responses may be triggered by the lockdown phenomenon [Citation21–23]. Afore mentioned factors together with sedentary lifestyles during COVID-19 pandemic lockdown are linked not only to a BP elevation but also to other adverse cardiovascular effects [Citation1]. Increased stress levels, social isolation, and home confinement may all affect sleep behaviour, and BP 24-h profiles.
The survey of the 52 Excellence Centres (ECs) of the European Society of Hypertension showed that the number of patients treated per week significantly decreased during the pandemic [Citation9]. In addition, diagnostic and therapeutic procedures related to hypertension were dramatically reduced during the first year of the COVID-19 pandemic, with the largest reduction occurring during the first lockdown [Citation24].
At the onset of the pandemic there were considerations about possible influence of ACEI or ARB use on increased risk of infection and the severity of the COVID-19, which resulted in temporal stopping of RAS-blocker therapy either by patients (27%) or physicians (36.5%) as reported by ECs [Citation9].
Data are scarce for assessing the pandemic’s effect on BP. In a study conducted in a Hypertension Unit in Milan, Italy, among 126 patients the authors showed that, despite the inability to have access to healthcare services, home BP was either the same or lower than during both pre-lockdown and a reference period selected over the same time window the year before [Citation10]. Similar results were reported from BP measurement using telemonitored home BP monitor in persons living in the Paris urban area. Among 2273 participants, a decrease in home BP monitoring during the first lockdown period was observed [Citation25].
Study on office BP and home BP monitoring in a large nationwide sample in Brazil came to similar conclusions. Slight reductions in office and home BP values were detected in the immediate months following the COVID-19 pandemic outbreak among patients treated with antihypertensive medications (n = 987) in whom BP measurements before and during the pandemic were available, but not among untreated (n = 495) participants [Citation13].
Different conclusions can be drawn from the analyses of 464 585 employees and their spouses/partners, from all 50 states of USA and the District of Columbia, who participated in an annual employer-sponsored wellness program [Citation11]. This recently published study showed that the annual BP increase was significantly higher in April to December 2020 than in 2019. Moreover, in April to December 2020, compared with the pre-pandemic period, a greater proportion of participants were up-categorized than down-categorized within the stages of hypertension definition. As a point of interest, during the pandemic period a larger systolic and diastolic BP increase was noted in women, in older participants (systolic BP only), and in younger participants (diastolic BP only) [Citation11].
It is evident that more studies on this topic are required to better characterise the effect of the COVID-19-related lockdown on BP control and the predictors of BP changes using a large cohort of patients as well as a more precise BP phenotyping approach, such as ABPM. General practitioners, hypertension specialists, and cardiologists need to be prepared for a different scenario in the future and take advantage of this challenging time by implementing the current healthcare modalities with new e-health methods [Citation26].
In February 2021, the European Society of Hypertension COVID-19 Task Force initiated a new ESH ABPM COVID-19 study with the main goal to determine the impact of COVID-19 lockdown on BP values and phenotypes as assessed by ABPM through the comparison of ABPM results obtained before and during lockdown in already treated hypertensive patients [Citation4].
ABPM has become a substantial tool in hypertension diagnosis and management and its role is now recognised by guidelines for hypertension management of major scientific societies. ABPM provides a more accurate estimate of individual’s BP status, reducing random error, inherent in office measurement and also eliminating systematic BP overestimation due to the white coat effect. In addition, it also allows to assess BP during sleep; this feature represents a key advantage over home BP monitoring. Finally, prognostically relevant estimates of BP variability can be obtained from ABPM recordings [Citation4]. Specifically, we hypothesise that ambulatory BP levels were modified in the pandemic period compared with pre-pandemic one. Mortality data suggest that effects of COVID-19 pandemic on cardiovascular disease will be delayed rather than contemporaneous. There is a substantial avoidable burden of excess mortality in people with CVD during the COVID-19 pandemic. Excess CVD deaths can be reduced in more integrated approaches, focussed on reducing COVID-19 infection rates, as well as managing CVD and comorbidities [Citation27].
Perspectives
The COVID-19 pandemic, including the lockdown period, has the potential to increase cardiovascular morbidity and mortality by influencing the course of established CVD as well as by negatively affecting the control of cardiovascular risk factors. Hypertension is one of the major risk factors for CVD. By extending our knowledge about the effects of the COVID-19 pandemic on BP control in patients with hypertension, we can propose appropriately effective strategies for providing adequate medical care in case of new pandemic waves and for long-term care, which will reduce incidence of CVD because of the current pandemic.
The ESH ABPM COVID-19 investigators
Coordinating Centre
Jagiellonian University Medical College, 1st Department of Cardiology, Interventional Electrocardiology and Arterial Hypertension, Krakow, Poland: Wiktoria Wojciechowska, Aleksandra Ostrowska; Hypertension Centre Berlin Charité, Berlin, Germany: Markus van der Giet; Hypertension Centre of Sotiria Hospital, Athens, Greece: Angeliki Ntineri; Hypertension Clinic, Department of Internal Medicine, Hospital Clinic, University of Barcelona, Spain: Miguel Camafort; National Institute of Cardiology, Warsaw, Poland: Elżbieta Szwench, Maria Gosk, Bogna Puciłowska, Katarzyna Purtak; ESH Coordinator: Mandy Elgner.
Participating centres
Hypertension Unit, Hospital Europeen Georges Pompidou, Paris, France: Michel Azizi; Istituto Auxologico Italiano, S.Luca Hospital, Cardiology Unit and Dept of Cardiovascular, Neural and Metabolic Sciences, Milano, Italy: Grzegorz Bilo; Hypertension and Cardiovascular Risk Factors Research Centre, Medical and Surgical Sciences Department, S. Orsola-Malpighi Polyclinic, Bologna, Italy: Claudio Borghi; Academic Medical Centre Amsterdam, Netherlands: Bert Jan van den Born; Dr. Peter Drzaj Hospital, Ljubljana, Slovenia: Jana Brguljan; Hadassah Hebrew University Medical Centre, Mount-Scopus (Associated Centre), Jerusalem, Israel: Michael Bursztyn; Hypertension Clinic, Internal Medicine, Hospital Clinic, University of Barcelona, Barcelona, Spain: Antonio Coca; Department of Internal Medicine, Hypertension and Clinical Oncology, Faculty of Medicine, Wroclaw Medical University, Wroclaw, Poland: Adrian Doroszko; Geneva University Hospital, Geneva, Switzerland: Georg Ehret; Hypertension Centre Berlin Charité, Berlin, Germany: Marcus van der Giet; Hypertension Clinic, Department of Cardiology, KAT General Hospital, Athens, Greece: Charalampos Grassos; Virgen de las Nieves University Hospital, Granada, Spain: Fernando Jaen Águila; National Institute of Cardiology, Warsaw, Poland: Andrzej Januszewicz; St. Imre Teaching Hospital, Budapest, Hungary: Zoltan Jarai; Unit of Hypertension and Hyperlipidaemia, Department of Cardiology, Danderyd University Hospital, Stockholm, Sweden: Thomas Kahan; Papageorgiou Hospital, Nea Efkarpia, Thessaloniki, Greece: Vasilios Kotsis; Department of Internal Medicine, Hypertension and Vascular Diseases, Medical University of Warsaw, Warsaw, Poland: Jacek Lewandowski; Department of Internal Medicine, ESH Hypertension Excellence Centre (M.L.-S.), CHU Avicenne, AP-HP, Bobigny, France: Marilucy Lopez – Sublet; Clinic for Internal Disease InterMedica, Nis, Serbia: Dragan Lovic; University Hospital Laiko, Athens, Greece: Dimitrios Papadopoulos; IRCCS Istituto Auxologico Italiano, Milano, Italy: Gianfranco Parati; Hospital Pedro Hispano, Matosinhos, Portugal: Jorge Polonia; Hypertension Unit, Department of Hypertension and Diabetology, Medical University of Gdansk, Gdansk, Poland: Krzysztof Narkiewicz; Hypertension Clinic, Internal Medicine, Hospital Clinic, University of Valencia, Valencia, Spain: Josep Redon; First Department of Cardiology, Interventional Electrocardiology and Hypertension, Jagiellonian University Medical College, Krakow, Poland: Marek Rajzer; Hospital Infanta Cristina, Badajoz, Spain: Nicolas Roberto Robles; University ‘Politecnica delle Marche’, IRCCS INRCA, Ancona, Italy: Riccardo Sarzani; Danderyd Hospital, Danderyd, Sweden: Jonas Spaak; Hypertension Centre of Sotiria Hospital, Athens, Greece: George Stergiou; Department of Internal Medicine, Institute of Medical Sciences, Medical College, University of Rzeszów, Poland: Katarzyna Styczkiewicz; University of Athens, Hippokration Hospital, Athens, Greece: Costas Tsioufis; University Hospital, Olomouc, Czech Republic: Jan Vaclavik; A.O.U. City of Health and Science of Turin, Turin, Italy: Franco Veglio; Cardiology Department Klinikum Wels-Grieskirchen, Wels, Austria: Thomas Weber; Centre for Hypertension, Charles University, Prague, Czech Republic: Jiri Widmiski; Hypertension Centre of the Lausanne University Hospital, Service of Nephrology and Hypertension, Lausanne, Switzerland: Gregoire Wuerzner; Department of Internal Medicine and Gerontology, Jagiellonian University Medical College, Krakow, Poland: Tomasz Grodzicki; Department of Nephrology and Hypertension, Universitair Ziekenhuis Brussel (VUB), Brussels, Belgium: Patricia Van der Niepen; II Clinic of Cardiology and Internal Medicine, Collegium Medicum, School of Medicine, University of Warmia and Mazury in Olsztyn, Olsztyn, Poland: Beata Moczulska; II Department of Nephrology and Hypertension with Dialysis Unit, Medical University of Białystok, Białystok, Poland: Edyta Zbroch; Department of Heart Disease, Haukeland University Hospital, Bergen, Norway: Sahrai Saeed; 3rd Department of Internal Medicine, Papageorgiou Hospital, Faculty of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece: Eugenia Gkaliagkousi.
Study registration
The study has been registered at ClinicalTrials.gov with identifier: NCT05167240
Acknowledgment
The authors are indebted to Mandy Elgner, program coordinator of the ESH, for invaluable assistance in the logistics of recruitment of centres and data collection process.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Kreutz R, Dobrowolski P, Prejbisz A, European Society of Hypertension COVID-19 Task Force Review, et al. Lifestyle, psychological, socioeconomic and environmental factors and their impact on hypertension during the coronavirus disease 2019 pandemic. J Hypertens. 2021;39(6):1077–1089.
- Pecanha T, Goessler KF, Roschel H, et al. Social isolation during the covid-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;318(6):H1441–H1446.
- Januszewicz A, Wojciechowska W, Prejbisz A, et al. Impact of the COVID-19 pandemic on blood pressure control and cardiovascular risk profile in patients with hypertension. Pol Arch Intern Med. 2021;131:16129.
- Williams B, Mancia G, Spiering W, ESC Scientific Document Group, et al. ESC scientific document group. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104.
- Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4):e21.
- Zheng YY, Ma YT, Zhang JY, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260.
- Williams B. Renin-angiotensin system inhibitors in hospitalised patients with COVID-19. Lancet Respir Med. 2021;9(3):221–222.
- Kreutz R, Algharably EAE, Azizi M, et al. Hypertension, the renin-angiotensin system, and the risk of lower respiratory tract infections and lung injury: implications for covid-19. Cardiovasc Res. 2020;116(10):1688–1699.
- The corona-virus disease 2019 pandemic compromised routine care for hypertension: a survey conducted among excellence centers of the european society of hypertension. J Hypertens. 2021;39:190–195.
- Pengo MF, Albini F, Guglielmi G, et al. Home blood pressure during covid-19-related lockdown in patients with hypertension. Eur J Prev Cardiol. 2022;29(3):e94–e96.
- Laffin LJ, Kaufman HW, Chen Z, et al. Rise in blood pressure observed Among US adults During the COVID-19 pandemic. Circulation. 2022;145(3):235–237.
- Gotanda H, Liyanage-Don N, Moran AE, et al. Changes in blood pressure outcomes Among hypertensive individuals During the COVID-19 pandemic: a time series analysis in three US healthcare organizations. Hypertension. 2022;79(12):2733–2742.
- Feitosa FGAM, Feitosa ADM, Paiva AMG, et al. Impact of the COVID-19 pandemic on blood pressure control: a nationwide home blood pressure monitoring study. Hypertens Res. 2022;45(2):364–368.
- Omboni S, Ballatore T, Rizzi F, et al. Telehealth at scale can improve chronic disease management in the community during a pandemic: an experience at the time of COVID-19. PLoS One. 2021;16(9):e0258015.
- Stergiou GS, Palatini P, Parati G, European Society of Hypertension Council and the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability, et al. 2021 European society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–1302.
- Hoshide S, Kario K. Morning surge in blood pressure and stroke events in a large modern ambulatory blood pressure monitoring cohort: results of the JAMP study. Hypertension. 2021; Sep 78(3):894–896.
- Mena L, Pintos S, Queipo NV, et al. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005;23(3):505–511.
- Bilo G, Giglio A, Styczkiewicz K, et al. A new method for assessing 24-h blood pressure variability after excluding the contribution of nocturnal blood pressure fall. J Hypertens. 2007;25(10):2058–2066.
- Pina A, Castelletti S. COVID-19 and cardiovascular disease: a global perspective. Curr Cardiol Rep. 2021;23(10):135.
- The task force for the management of COVID-19 of the european society of cardiology, ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 2—care pathways, treatment, and follow-up. Europ Heart J. 2022;43(11):1059–1103.
- Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57.
- The Lancet Gastroenterology Hepatology Drinking alone: COVID-19, lockdown, and alcohol-related harm. Lancet Gastroenterol Hepatol. 2020;5(7):625.
- van Zyl-Smit RN, Richards G, Leone FT. Tobacco smoking and COVID-19 infection. Lancet Respir Med. 2020;8(7):664–665.
- Weber T, Amar J, de Backer T, Covid-19 Task Force of the European Society of Hypertension, et al. Covid-19 associated reduction in hypertension-related diagnostic and therapeutic procedures in excellence centers of the european society of hypertension. Blood Press. 2022;31(1):71–79.
- Girerd N, Meune C, Duarte K, et al. Evidence of a blood pressure reduction During the COVID-19 pandemic and associated lockdown period: insights from e-Health data. Telemed J E Health. 2022;28(2):266–270.
- Burnier M, Kjeldsen SE, Narkiewicz K, et al. Hypertension management during the COVID-19 pandemic: what can we learn for the future? Blood Press. 2022;31(1):47–49.
- Banerjee A, Chen S, Pasea L, et al. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prev Cardiol. 2021;28(14):1599–1609.